Dental Caries and Oral Health Status of Psychoactive Substance Abusers
Abstract
:1. Introduction
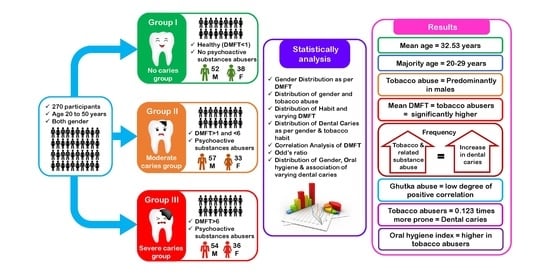
2. Materials and Methods
2.1. Inclusion Criteria for Group A Patients
- Dentate participants of 20–50 years of age.
- History of using tobacco and/or related substances for a minimum of 5 years.
- Residents of Piparia village, Vadodara city.
- Consuming only municipal water.
2.2. Exclusion Criteria for Group A Patients
- Occasional tobacco abusers.
- Participants with special health care needs.
- Participants with systemic disease.
- Pregnant and adolescent females, and females having systemic diseases or hormonal disturbances.
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization. Neuroscience of Psychoactive Substance Use and Dependence; World Health Organization: Geneva, Switzerland, 2004; ISBN 9241562358. [Google Scholar]
- Seitz, N.-N.; Lochbühler, K.; Atzendorf, J.; Rauschert, C.; Pfeiffer-Gerschel, T.; Kraus, L. Trends in Substance Use and Related Disorders: Analysis of the Epidemiological Survey of Substance Abuse 1995 to 2018. Dtsch. Arztebl. Int. 2019, 116, 585. [Google Scholar]
- OECD. Health at A Glance: Asia/Pacific 2020; OECD: Paris, France, 2020; ISBN 9789264445673. [Google Scholar]
- Muttapppallymyalil, J.; Sreedharan, J.; Divakaran, B. Smokeless Tobacco Consumption among School Children. Indian J. Cancer 2010, 47, 19. [Google Scholar] [CrossRef] [PubMed]
- Awan, K.H.; Patil, S. Association of Smokeless Tobacco with Oral Cancer—Evidence from the South Asian Studies: A Systematic Review. J. Coll. Physicians Surg. Pakistan 2016, 26, 775–780. [Google Scholar]
- Chhabra, A.; Hussain, S.; Rashid, S. Recent Trends of Tobacco Use in India. J. Public Health 2021, 29, 27–36. [Google Scholar] [CrossRef]
- Gupta, P.C.; Warnakulasuriya, S. Global Epidemiology of Areca Nut Usage. Addict. Biol. 2002, 7, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Rooban, T.; Rao, A.; Joshua, E.; Ranganathan, K. Dental and Oral Health Status in Drug Abusers in Chennai, India: A Cross-Sectional Study. J. Oral Maxillofac. Pathol. 2008, 12, 16. [Google Scholar] [CrossRef]
- Mack, T.M. The New Pan-Asian Paan Problem. Lancet 2001, 357, 1638–1639. [Google Scholar] [CrossRef]
- Shah, S.; Dave, B.; Shah, R.; Mehta, T.R.; Dave, R. Socioeconomic and Cultural Impact of Tobacco in India. J. Fam. Med. Prim. Care 2018, 7, 1173. [Google Scholar]
- Sauvaget, C.; Ramadas, K.; Thara, S.; Thomas, G.; Sankaranarayanan, R. Tobacco Chewing in India. Int. J. Epidemiol. 2008, 37, 1242–1245. [Google Scholar] [CrossRef] [Green Version]
- Mallikarjuna, R.; Gangwal, R.R.; Shanthraj, S.L.; Dave, B. Report of Gutkha (Smokeless Tobacco) Use in Children Aged 10–12 Years. Case Rep. 2013, 2013, bcr2012008319. [Google Scholar] [CrossRef] [Green Version]
- Awan, K.H.; Hussain, Q.A.; Patil, S.; Maralingannavar, M. Assessing the Risk of Oral Cancer Associated with Gutka and Other Smokeless Tobacco Products: A Case-Control Study. J Contemp Dent Pract. 2016, 17, 740–744. [Google Scholar] [CrossRef] [PubMed]
- Bhisey, R.A. Chemistry and Toxicology of Smokeless Tobacco. Indian J. Cancer 2012, 49, 364. [Google Scholar] [CrossRef] [PubMed]
- Barik, A.; Rai, R.K.; Gorain, A.; Majumdar, S.; Chowdhury, A. Socio-Economic Disparities in Tobacco Consumption in Rural India: Evidence from a Health and Demographic Surveillance System. Perspect. Public Health 2016, 136, 278–287. [Google Scholar] [CrossRef]
- Mohanty, V.; Subbannayya, Y.; Patil, S.; Abdulla, R.; Ganesh, M.S.; Pal, A.; Ray, J.G.; Sidransky, D.; Gowda, H.; Prasad, T.S. Molecular Alterations in Oral Cancer between Tobacco Chewers and Smokers Using Serum Proteomics. Cancer Biomark. 2021, 31, 361–373. [Google Scholar] [CrossRef]
- Patil, S.; Jafer, M.; Anil, S. Smokeless Tobacco-Patterns of Consumption, Oral Potentially Malignant Disorders, and Other Oral Health Issues. J. Int. Oral Health 2016, 8, I. [Google Scholar]
- Pitts, N.B.; Twetman, S.; Fisher, J.; Marsh, P.D. Understanding Dental Caries as a Non-Communicable Disease. Br. Dent. J. 2021, 231, 749–753. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Study 2019 (GBD 2019) Reference Life Table|GHDx. Available online: https://ghdx.healthdata.org/record/ihme-data/global-burden-disease-study-2019-gbd-2019-reference-life-table (accessed on 10 April 2022).
- Monse, B.; Heinrich-Weltzien, R.; Benzian, H.; Holmgren, C.; van Palenstein Helderman, W. PUFA–an Index of Clinical Consequences of Untreated Dental Caries. Community Dent. Oral Epidemiol. 2010, 38, 77–82. [Google Scholar] [CrossRef]
- Al-Marzooq, F.; Al Kawas, S.; Rahman, B.; Shearston, J.A.; Saad, H.; Benzina, D.; Weitzman, M. Supragingival Microbiome Alternations as a Consequence of Smoking Different Tobacco Types and Its Relation to Dental Caries. Sci. Rep. 2022, 12, 2861. [Google Scholar] [CrossRef]
- Huang, R.; Li, M.; Gregory, R.L. Effect of Nicotine on Growth and Metabolism of Streptococcus Mutans. Eur. J. Oral Sci. 2012, 120, 319–325. [Google Scholar] [CrossRef]
- Sharma, S.; Mittal, N.; Mishra, S.K. Influence of Tobacco Dependence on Caries Development in Young Male Adults: A Cross-Sectional Study. J. Conserv. Dent. 2018, 21, 597–601. [Google Scholar] [CrossRef]
- Rad, M.; Kakoie, S.; Brojeni, F.N.; Pourdamghan, N. Effect of Long-Term Smoking on Whole-Mouth Salivary Flow Rate and Oral Health. J. Dent. Res. Dent. Clin. Dent. Prospects 2010, 4, 110. [Google Scholar] [PubMed]
- Kanwar, A.; Sah, K.; Grover, N.; Chandra, S.; Singh, R.R. Long-Term Effect of Tobacco on Resting Whole Mouth Salivary Flow Rate and PH: An Institutional Based Comparative Study. Eur. J. Gen. Dent. 2013, 2, 296–299. [Google Scholar] [CrossRef]
- Golpasand Hagh, L.; Zakavi, F.; Ansarifar, S.; Ghasemzadeh, O.; Solgi, G. Association of Dental Caries and Salivary SIgA with Tobacco Smoking. Aust. Dent. J. 2013, 58, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Sinha, D.N.; Gupta, P.C.; Pednekar, M.S. Use of Tobacco Products as Dentifrice among Adolescents in India: Questionnaire Study. BMJ 2004, 328, 323–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benedetti, G.; Campus, G.; Strohmenger, L.; Lingström, P. Tobacco and Dental Caries: A Systematic Review. Acta Odontol. Scand. 2013, 71, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Jiang, X.; Wang, Y.; Huang, R. Correlation between Tobacco Smoking and Dental Caries: A Systematic Review and Meta-Analysis. Tob. Induc. Dis. 2019, 17, 34. [Google Scholar] [CrossRef] [PubMed]
- Pandey, P.; Nandkeoliar, T.; Tikku, A.P.; Singh, D.; Singh, M.K. Prevalence of Dental Caries in the Indian Population: A Systematic Review and Meta-Analysis. J. Int. Soc. Prev. Community Dent. 2021, 11, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Tomar, S.L.; Winn, D.M. Chewing Tobacco Use and Dental Caries among U.S. Men. J. Am. Dent. Assoc. 1999, 130, 1601–1610. [Google Scholar] [CrossRef]
- Aguilar-Zinser, V.; Irigoyen, M.E.; Rivera, G.; Maupomé, G.; Sánchez-Pérez, L.; Velázquez, C. Cigarette Smoking and Dental Caries among Professional Truck Drivers in Mexico. Caries Res. 2008, 42, 255–262. [Google Scholar] [CrossRef]
- Rwenyonyi, C.M.; Muwazi, L.M.; Buwembo, W. Assessment of Factors Associated with Dental Caries in Rural Communities in Rakai District, Uganda. Clin. Oral Investig. 2011, 15, 75–80. [Google Scholar] [CrossRef]
- Hsu, S.C.; Pollack, R.L.; Hsu, A.F.; Going, R.E. Sugars Present in Tobacco Extracts. J. Am. Dent. Assoc. 1980, 101, 915–918. [Google Scholar] [CrossRef] [PubMed]
- Fant, R.V.; Henningfield, J.E.; Nelson, R.A.; Pickworth, W.B. Pharmacokinetics and Pharmacodynamics of Moist Snuff in Humans. Tob. Control 1999, 8, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Rooban, T.; Vidya, K.; Joshua, E.; Rao, A.; Ranganathan, S.; Rao, U.; Ranganathan, K. Tooth Decay in Alcohol and Tobacco Abusers. J. Oral Maxillofac. Pathol. 2011, 15, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, S.; Mehrotra, D.; Mishra, S.; Goel, M.M.; Kumar, S.; Mathur, P.; Choudhary, K.; Pandey, C.M. Epidemiology of Substance Abuse in the Population of Lucknow. J. Oral Biol. Craniofacial Res. 2015, 5, 128–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badel, T.; Savić Pavičin, I.; Jelinić Carek, A.; Šegović, S. Dental Caries Experience and Tobacco Use in 19-Year-Old Croatian Army Recruits. Coll. Antropol. 2014, 38, 677–680. [Google Scholar]
- Axelsson, P.; Paulartder, J.; Lindhe, J. Relationship between Smoking and Dental Status in 35-, 50-, 65-, and 75-Year-Old Individuals. J. Clin. Periodontol. 1998, 25, 297–305. [Google Scholar] [CrossRef]
- Bhonsle, R.B.; Murti, P.R.; Gupta, P.C. Tobacco Habits in India. In Control of Tobacco-Related Cancers and Other Diseases; Oxford University Press: Bombay, India, 1992; pp. 25–46. [Google Scholar]
- Mukherjea, A. Tobacco Industry Co-Optation of Culture? Converging Culturally Specific and Mainstream Tobacco Products in India. Tob. Control 2012, 21, 63–64. [Google Scholar] [CrossRef]
- Raj, A.T.; Patil, S.; Gupta, A.A.; Suveetha, G. Flavored Tobacco to E-Cigarette’s: How the Tobacco Industry Sustains Its Product Flow. Oral Oncol. 2018, 85, 110. [Google Scholar] [CrossRef]
- Sreenivasan, S.T.; Nattala, P.; Rao, G.N.; Sridaramurthy, M.K. So What If I Use Tobacco or Alcohol? It Won’t Hurt Me! How Women Perceive Substance Use: Insights from a Community Study in India. Arch. Womens. Ment. Health 2022, 25, 129–136. [Google Scholar] [CrossRef]
- Weintraub, J.A.; Burt, B. Periodontal Effects and Dental Caries Associated with Smokeless Tobacco Use. Public Health Rep. 1987, 102, 30–35. [Google Scholar]
- Winn, D.M. Tobacco Use and Oral Disease. J. Dent. Educ. 2001, 65, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, T.; Marugame, T.; Ohara, S.; Inoue, M.; Tsugane, S.; Kawaguchi, Y. Relationship of Smoking and Smoking Cessation with Number of Teeth Present: JPHC Oral Health Study. Oral Dis. 2009, 15, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Miyake, Y.; Arakawa, M.; Sasaki, S.; Ohya, Y. Household Smoking and Dental Caries in Schoolchildren: The Ryukyus Child Health Study. BMC Public Health 2010, 10, 335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bloom, B.; Adams, P.F.; Cohen, R.A.; Simile, C. Smoking and Oral Health in Dentate Adults Aged 18-64. NCHS Data Brief 2012, 8, 1–8. [Google Scholar]
- Lashkari, K.P.; Shukla, A. Prevalence of Dental Caries among Smokeless Tobacco Chewers in Dakshina Kannada District Population: A Cross Sectional Study. Oral Health Dent. Manag. 2016, 15, 1–3. [Google Scholar]
- Chaitanya, N.; Boringi, M.; Madathanapalle, R.; Renee, A.; Sree, S.; Priyanka, N.; Sownetha, T.; Marella, K. The Prevalence of Dental Caries in Smokers and Smokeless Tobacco Users. Dent. Hypotheses 2018, 9, 36. [Google Scholar] [CrossRef]
- Shah, S.V.S. Pavement Dwellers in Mumbai, India: Prioritizing Tobacco over Basic Needs. In Tobacco and Poverty: Observation from India and Bangladesh; Efroymson, D., Ed.; PATH: Dhaka, Bangladesh, 2002. [Google Scholar]
- Shah, S.V.S. Choosing Tobacco over Food: Daily Struggles for Existence among Street Children of Mumbai, India. In Tobacco and Poverty: Observation from India and Bangladesh; Efroymson, D., Ed.; PATH: Dhaka, Bangladesh, 2002. [Google Scholar]
- Möller, I.J.; Pindborg, J.J.; Effendi, I. The Relation between Betel Chewing and Dental Caries. Eur. J. Oral Sci. 1977, 85, 64–70. [Google Scholar] [CrossRef]
- El-Ezmerli, N.F.; Gregory, R.L. Effect of Nicotine on Biofilm Formation of Streptococcus Mutans Isolates from Smoking and Non-Smoking Subjects. J. Oral Microbiol. 2019, 11, 1662275. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Qiu, W.; Zhang, K.; Zhou, X.; Ren, B.; He, J.; Xu, X.; Cheng, L.; Li, M. Nicotine Enhances Interspecies Relationship between Streptococcus Mutans and Candida Albicans. Biomed Res. Int. 2017, 2017, 7953920. [Google Scholar] [CrossRef] [Green Version]
- Vallès, Y.; Inman, C.K.; Peters, B.A.; Ali, R.; Wareth, L.A.; Abdulle, A.; Alsafar, H.; Al Anouti, F.; Al Dhaheri, A.; Galani, D. Types of Tobacco Consumption and the Oral Microbiome in the United Arab Emirates Healthy Future (UAEHFS) Pilot Study. Sci. Rep. 2018, 8, 1–11. [Google Scholar]
- Halboub, E.; Al-Ak’hali, M.S.; Alamir, A.H.; Homeida, H.E.; Baraniya, D.; Chen, T.; Al-Hebshi, N.N. Tongue Microbiome of Smokeless Tobacco Users. BMC Microbiol. 2020, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Alaizari, N.A.; Al-Anazi, J.R. Oral Candida Carriage in Smokers and Tobacco Users: A Systematic Review and Meta-Analysis of Observational Studies. J. Oral Biosci. 2020, 62, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, M.D. Tobacco and Dental Caries. J. Am. Coll. Dent. 1952, 19, 365–367. [Google Scholar]
- Schmidt, H.J. Tobacco Smoke and the Teeth. Stoma 1951, 4, 111–125. [Google Scholar]
- Hugoson, A.; Hellqvist, L.; Rolandsson, M.; Birkhed, D. Dental Caries in Relation to Smoking and the Use of Swedish Snus: Epidemiological Studies Covering 20 Years (1983–2003). Acta Odontol. Scand. 2012, 70, 289–296. [Google Scholar] [CrossRef]
- Sgan-Cohen, H.D.; Katz, J.; Horev, T.; Dinte, A.; Eldad, A. Trends in Caries and Associated Variables among Young Israeli Adults over 5 Decades. Community Dent. Oral Epidemiol. 2000, 28, 234–240. [Google Scholar] [CrossRef]
- Manisha Kaul, A.P. Association of Tobacco Habits with Dental Caries and Streptococcus Mutans Count. Int. J. Appl. Dent. Sci. Age 2019, 5, 479–483. [Google Scholar]
| Gender | Grade of DMFT | Total | p-Value | Chi-Square χ2 | |||||
|---|---|---|---|---|---|---|---|---|---|
| No Caries Moderate Caries Severe Caries | |||||||||
| N | % | N | % | N | % | ||||
| Male | 52 | 31.90% | 57 | 34.97% | 54 | 33.13% | 163 | 0.745 | |
| Female | 38 | 35.51% | 33 | 30.84% | 36 | 33.64% | 107 | 4.211 | |
| Total | 90 | 33.33% | 90 | 33.33% | 90 | 33.33% | 270 | ||
| Type of Habit | Male | Female | Total | p-Value |
|---|---|---|---|---|
| No Habit | 58 (35.58%) | 77 (71.96%) | 135 (50.00%) | 0.001 |
| Tobacco (padiki) | 35 (21.47%) | 17 (15.89%) | 52 (13.70%) | |
| Gutkha | 43 (26.38%) | 6 (5.61%) | 49 (25.19%) | |
| Smoking | 25 (15.34%) | 1 (0.93%) | 26 (10.74%) | |
| Betel Nuts | 0 (0.00%) | 5 (4.67%) | 5 (0.37%) | |
| Mixed | 2 (1.23%) | 1 (0.93%) | 3 (1.11%) | |
| Total | 163 | 107 | 270 |
| Dental Caries Status | Tobacco User | Tobacco Non User | t Value | dF | p-Value | Mean Difference | Std. Error Difference | 95% Confidence Interval of the Difference | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Lower | Upper | ||||||
| Total DMFT | 4.73 | 4.32 | 3.17 | 3.11 | 3.39 | 243.48 | 0.0010 | 1.5556 | 0.4583 | 0.6528 | 2.4583 |
| Total D | 2.24 | 2.05 | 1.67 | 1.96 | 2.37 | 267.45 | 0.0190 | 0.5778 | 0.2440 | 0.0974 | 1.0582 |
| Total Missing | 0.58 | 0.97 | 0.31 | 0.83 | 2.43 | 262.34 | 0.0160 | 0.2667 | 0.1097 | 0.0506 | 0.4828 |
| Total Filled | 0.93 | 1.29 | 1.47 | 1.82 | −2.81 | 242.22 | 0.0050 | −0.5407 | 0.1919 | −0.9187 | −0.1628 |
| OHI | 3.62 | 1.23 | 2.64 | 1.11 | 6.87 | 265.18 | 0.0001 | 0.9776 | 0.1423 | 0.6975 | 1.2578 |
| DMFT | p | |
|---|---|---|
| Gender | 0.184 (NS) | |
| Male | 4.20 ± 3.93 | |
| Female | 3.57 ± 3.68 | |
| Habit | 0.001 (HS) | |
| No Habit | 3.17 ± 3.11 | |
| Habit Present | 4.73 ± 4.32 | |
| Tobacco (padiki) | 0.424 (NS) | |
| Non-user | 3.85 ± 3.73 | |
| Abuser | 4.37 ± 4.26 | |
| Gutka | 0.017 (S) | |
| Non-user | 3.64 ± 3.62 | |
| Abuser | 5.33 ± 4.50 | |
| Smoking | 0.676 (NS) | |
| Non-user | 3.91 ± 3.82 | |
| Abuser | 4.27 ± 4.11 | |
| Betel Nut | 0.706 (NS) | |
| Non-user | 3.93 ± 3.83 | |
| Abuser | 4.80 ± 4.76 | |
| Mixed Habit | 0.772 (NS) | |
| Non-user | 3.94 ± 3.83 | |
| Abuser | 5.00 ± 5.57 |
| Frequency | Duration | Tobacco (Padiki) | Gutka | Smoking | Betel Nut | Mixed | ||
|---|---|---|---|---|---|---|---|---|
| Total DMFT | Pearson Correlation | 0.15 | 0.24 | 0.05 | 0.17 | 0.03 | 0.03 | 0.03 |
| p value | 0.013 | 0.000 | 0.384 | 0.005 | 0.655 | 0.617 | 0.634 |
| Unstandardized Coefficients | Odds Ratio | t | p-Value | ||
|---|---|---|---|---|---|
| B | Std. Error | ||||
| (Constant) | 3.170 | 0.325 | 9.748 | 0.000 | |
| Tobacco | 1.195 | 0.617 | 0.123 | 1.938 | 0.054 |
| Gutka | 2.156 | 0.630 | 0.217 | 3.421 | 0.001 |
| Smoking | 1.099 | 0.809 | 0.085 | 1.358 | 0.176 |
| Betel Nut | 1.630 | 1.721 | 0.057 | 0.947 | 0.345 |
| Mixed | 1.830 | 2.206 | 0.050 | 0.829 | 0.408 |
| Gender | OHI | Grade of DMFT | Total | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| No Caries | % | Mod Caries | % | Severe Caries | % | ||||
| Male | Good | 6 | 85.71% | 1 | 14.29% | 0 | 0.00% | 7 | 0.001 |
| Fair | 34 | 50.00% | 19 | 27.94% | 15 | 22.06% | 68 | ||
| Poor | 12 | 13.64% | 37 | 42.05% | 39 | 44.32% | 88 | ||
| Total | 52 | 31.90% | 57 | 34.97% | 54 | 33.13% | 163 | ||
| Female | Good | 2 | 66.67% | 1 | 33.33% | 0 | 0.00% | 3 | 0.020 |
| Fair | 26 | 48.15% | 15 | 27.78% | 13 | 24.07% | 54 | ||
| Poor | 10 | 20.00% | 17 | 34.00% | 23 | 46.00% | 50 | ||
| Total | 38 | 35.51% | 33 | 30.84% | 36 | 33.64% | 107 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhavsar, R.; Shah, V.; Ajith, N.A.; Shah, K.; Al-amoudi, A.; Bahammam, H.A.; Bahammam, S.A.; Zidane, B.; Albar, N.H.M.; Bhandi, S.; et al. Dental Caries and Oral Health Status of Psychoactive Substance Abusers. Int. J. Environ. Res. Public Health 2022, 19, 5818. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph19105818
Bhavsar R, Shah V, Ajith NA, Shah K, Al-amoudi A, Bahammam HA, Bahammam SA, Zidane B, Albar NHM, Bhandi S, et al. Dental Caries and Oral Health Status of Psychoactive Substance Abusers. International Journal of Environmental Research and Public Health. 2022; 19(10):5818. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph19105818
Chicago/Turabian StyleBhavsar, Rashmi, Vandana Shah, Namratha A. Ajith, Kinjal Shah, Ahmed Al-amoudi, Hammam Ahmed Bahammam, Sarah Ahmed Bahammam, Bassam Zidane, Nassreen Hassan Mohammad Albar, Shilpa Bhandi, and et al. 2022. "Dental Caries and Oral Health Status of Psychoactive Substance Abusers" International Journal of Environmental Research and Public Health 19, no. 10: 5818. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph19105818