A New Route of Fucoidan Immobilization on Low Density Polyethylene and Its Blood Compatibility and Anticoagulation Activity
Abstract
:1. Introduction
2. Results
2.1. Surface Wettability Behaviour
2.2. Scanning Electron Microscopy Characterization
2.3. Atomic Force Microscopy Characterization
2.4. Fourier Transform Infrared Spectra Investigations
2.5. X-ray Photoelectron Spectroscopy Investigations
2.6. Anticoagulation Activity Studied in Vitro
3. Materials and Methods
3.1. Materials and Preparation
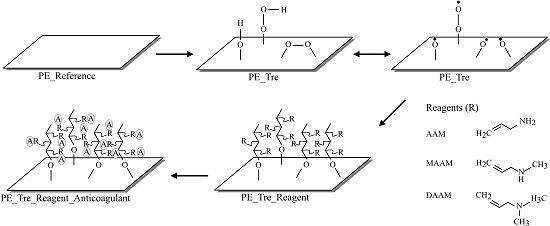
3.2. Plasma Surface Modification and Reagent Immobilization
3.3. Surface Wettability Evaluation
3.4. Scanning Electron Microscopy
3.5. Atomic Force Microscopy
3.6. Fourier Transform Infrared Spectroscopy
3.7. X-ray Photoelectron Spectroscopy
3.8. Anticoagulation Activity Test
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Jung, F.; Braune, S.; Lendlein, A. Hemocompatibility testing of biomaterials using human platelets. Clin. Hemorheol. Microc. 2003, 53, 97–115. [Google Scholar]
- Anderson, J.M.; Rodriguez, A.; Chang, D.T. Foreign body reaction to biomaterials. Semin. Immunol. 2008, 20, 86–100. [Google Scholar] [CrossRef] [PubMed]
- Horbett, T.A. Adsorbed proteis on biomaterials. In Biomaterials Science, an Introduction to Materials in Medicine, 3rd ed.; Ratner, B.D., Hoffman, A.S., Schoen, F.J., Lemons, J.E., Eds.; Elsevier INC.: London, UK, 2013; pp. 394–408. [Google Scholar]
- Xu, L.C.; Siedlecki, C.A. Effects of surface wettability and contact time on protein adhesion to biomaterial surfaces. Biomaterials 2007, 28, 3273–3283. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.C.; Bauer, J.W.; Siedlecki, C.A. Proteins, platelets and blood coagulation at biomaterial interfaces. Biointerfaces 2014, 124, 49–68. [Google Scholar] [CrossRef] [PubMed]
- Seyfert, U.T.; Biehl, V.; Schenk, J. In vitro hemocompatibility testing of biomaterials according to the ISO 10993–4. Biomol. Eng 2002, 19, 91–96. [Google Scholar] [CrossRef]
- Rana, D.; Matsuura, T. Surface modifications for antifouling membranes. Chem. Rev. 2010, 110, 2448–2471. [Google Scholar] [CrossRef] [PubMed]
- Vendra, V.K.; Wu, L.; Krishnan, S. Polymer Thin Films for Biomedical Applications. In Nanostructured Thin Films and Surfaces, 1st ed.; Kumar, C., Ed.; Wiley-VCH: Weinheim, Germany, 2010; pp. 1–54. [Google Scholar]
- Courtney, J.M.; Lamba, N.M.K.; Sundaram, S.; Forbes, C.D. Biomaterials for blood-contacting applications. Biomaterials 1994, 15, 737–744. [Google Scholar] [CrossRef]
- Ikada, Y. Surface modifications of polymers for medical applications. Biomaterials 1994, 15, 725–736. [Google Scholar] [CrossRef]
- Faxalv, L.; Ekblad, T.; Liedberg, B.; Lindahl, T.L. Blood compatibility of photografted hydrogel coatings. Acta Biomater. 2010, 6, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Cashman, J.D.; Kennah, E.; Shuto, A.; Winternitz, C.; Springate, C.M.K. Fucoidan film safely inhibits surgical adhesions in a rat model. J. Surg. Res. 2011, 171, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Yuan, L.; Song, W.; Wu, Z.; Li, D. Biocompatible polymer materials: Role of protein-surface interactions. Prog. Polym. Sci. 2008, 33, 1059–1087. [Google Scholar] [CrossRef]
- Kaleekkal, N.J.; Thanigaivelan, A.; Durga, M.; Girish, R.; Rana, D.; Soundararajan, P.; Mohan, D. Graphene oxide nanocomposite incorporated poly(ether imide) mixed matrix membranes for in vitro evaluation of its efficacy in blood purification applications. Ind. Eng. Chem. Res. 2015, 54, 7899–7913. [Google Scholar] [CrossRef]
- Chen, Z.; Wang, Z.; Fu, Q.; Ma, Z.; Fang, P.; He, C. Microstructure and surface state of plasma-treated high-density polyethylene elucidated by energy-tunable positron annihilation and water contact angle measurements. JJAP Conf. Proc. 2014. [Google Scholar] [CrossRef]
- Lehocky, M.; Lapcik, L.; Neves, M.C.; Trindade, T.; Szyk-Warszynska, L.; Warszynski, P.; Hui, D. Deposition/detachment of particles on plasma treated polymer surfaces. Mater. Sci. Forum Vols. 2003, 426–432, 2533–2538. [Google Scholar] [CrossRef]
- Lehocky, M.; Amaral, P.F.F.; Coelho, M.A.Z.; Stahel, P.; Barros-Timmons, A.M.; Coutinho, J.A.P. Attachment/detachment of Saccharomyces Cerevisiae on plasma deposited organosilicon thin films. Czechoslov. J. Phys. 2006, 56, B1256–B1262. [Google Scholar] [CrossRef]
- Lehocky, M.; Lapcik, L.; Dlabaja, R.; Rachunek, L. Influence of artificially accelerated ageing on the adhesive joint of plasma treated polymer materials. Czechoslov. J. Phys. 2004, 54, C533–C538. [Google Scholar] [CrossRef]
- Patel, D.; Wu, J.; Chan, P.; Upreti, S.; Turcotte, G.; Ye, T. Surface modification of low density polyethylene films by homogeneous catalytic ozonation. Chem. Eng. Res. Des. 2012, 90, 1800–1806. [Google Scholar] [CrossRef]
- Garcia, J.L.; Asadinezhad, A.; Pachernik, J.; Lehocky, M.; Junkar, I.; Humpolicek, P.; Saha, P.; Valasek, P. Cell proliferation of HaCaT keratinocytes on collagen films modified by argon plasma treatment. Molecules 2010, 15, 2845–2856. [Google Scholar] [CrossRef] [PubMed]
- Popelka, A.; Novak, I.; Lehocky, M.; Junkar, I.; Mozetic, M.; Kleinova, A.; Janigova, I.; Slouf, M.; Bilek, F.; Chodak, I. A new route for chitosan immobilization onto polyethylene surface. Carbohydr. Polym. 2012, 90, 1501–1508. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.L.; Bilek, F.; Lehocky, M.; Junkar, I.; Mozetic, I.; Sowe, M. Enhanced printability of polyethylene through air plasma treatment. Vacuum 2013, 95, 43–49. [Google Scholar] [CrossRef]
- Bilek, F.; Krizova, T.; Lehocky, M. Preparation of active antibacterial LDPE surface through multistep physicochemical approach: I. Allylamine grafting, attachment of antibacterial agent and antibacterial activity assessment. Colloids Surf. B Biointerfaces 2011, 88, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Nair, L.S.; Laurencin, C.T. Biodegradable polymers as biomaterials. Prog. Polym. Sci. 2007, 32, 762–798. [Google Scholar] [CrossRef]
- Azevedo, T.C.G.; Bezerra, M.E.B.; Santos, M.D.G.D.L.; Souza, L.A.; Marques, C.T.; Benevides, N.M.B.; Leite, E.L. Heparinoids algal and their anticoagulant, hemorrhagic activities and platelet aggregation. Biomed. Pharmacother. 2009, 63, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Dore, C.M.P.G.; Alves, M.G.C.F.; Will, L.S.E.P.; Costa, T.G.; Sabry, D.A.; Rego, L.A.R.S.; Accardo, C.M.; Rocha, H.A.O.; Filgueira, L.G.A.; Leite, E.L. A sulfated polysaccharide, fucans, isolated from brown algae Sargassum vulgare with anticoagulant, antithrombotic, antioxidant and anti-inflammatory effects. Carbohydr. Polym. 2013, 91, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Li, S.; Li, J.; Ye, X.; Ding, T.; Liu, D.; Chen, J.; Ge, Z.; Chen, S. Identification of a highly sulfated fucoidan from sea cucumber Pearsonothuria graeffei with well-repeated tetrasaccharides units. Carbohydr. Polym. 2015, 134, 808–816. [Google Scholar] [CrossRef] [PubMed]
- Jin, W.; Zhang, Q.; Wang, J.; Zhang, W. A comparative study of the anticoagulant activities of eleven fucoidans. Carbohydr. Polym. 2013, 91, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Yang, R.; Li, M.; Liang, X.; Elmada, Z.C. Effects of dietary fucoidan on the blood constituents, anti-oxidation and innate immunity of juvenile yellow catfisch (Pelteobagrus fulvidraco). Fish Shelfish Immunol. 2014, 41, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Tengdelius, M.; Lee, C.J.; Grenegard, M.; Griffith, M.; Pahlsson, P.; Konradsson, P. Synthesis and biological evaluation of fucoidan-mimetic glycopolymers through cyanoxyl-mediated free-radical polymerization. Biomacromolecules 2014, 15, 2359–2368. [Google Scholar] [CrossRef] [PubMed]
- Vesel, A.; Mozetic, M.; Strnad, S. Improvement of adhesion of fucoidan on polyethylene terephthalate surface using gas plasma treatments. Vacuum 2011, 85, 1083–1086. [Google Scholar] [CrossRef]
- Pielesz, A.; Binias, W. Cellulose acetate membrane electrophoresis and FTIR spectroscopy as methods of identifying a fucoidan in fucus vesiculosus linnaeus. Carbohydr. Res. 2010, 345, 2676–2682. [Google Scholar] [CrossRef] [PubMed]
- Rabanal, M.; Ponce, N.M.; Navarro, D.; Gomez, R.M.; Stortz, C. The system of fucoidans from the brown seaweed dictyota dichotoma: Chemical analysis and antiviral activity. Carbohydr. Polym. 2014, 101, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Dong, S.; Wang, J.; Li, F.; Chen, A.; Li, B. A comparative study of antithrombotic and antiplatelet activities of different fucoidans from Laminaria japonica. Thromb. Res. 2012, 129, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Ale, M.T.; Maruyama, H.; Tamauchi, H.; Mikkelsen, J.D.; Meyer, A.S. Fucoidan from Sargassum sp. and Fucus vesiculosus reduces cell viability of lung carcinoma and melanoma cells in vitro and activates natural killer cells in mice in vivo. Int. J. Biol. Macromol. 2011, 49, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Ustyuzhanina, N.E.; Bilan, M.I.; Gerbst, A.G.; Ushakova, N.A.; Tsvetkova, E.A.; Dmitrenok, A.S.; Usov, A.I.; Nifantiev, N.E. Anticoagulant and antithrombotic activities of modified xylofucan sulfate from the brown alga Punctaria plantaginea. Carbohydr. Polym. 2016, 136, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Zhang, Q.; Chen, L.; Ren, S.; Xu, P.; Tang, Y. Luo, D. Higher specificity of the activity of low molecular weight fucoidan for thrombin-induced platelet aggregation. Thromb. Res. 2010, 125, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Durig, J.; Bruhn, T.; Zurborn, K.H.; Gutensohn, K.; Bruhn, H.D.; Beress, L. Anticoagulant fucoidan fractions from fucus vesiculosus induce platelet activation in vitro. Thromb. Res. 1997, 85, 479–491. [Google Scholar] [CrossRef]
- Fitton, J.H. Therapies from fucoidan; multifunctional marine polymers. Mar. Drugs 2011, 9, 1731–1760. [Google Scholar] [CrossRef] [PubMed]
- Bilek, F.; Sulovska, K.; Lehocky, M.; Saha, P.; Humpolicek, P.; Mozetic, M.; Junkar, I. Preparation of active antibacterial LDPE surface through multistep physicochemical approach II: Graft type effect on antibacterial properties. Colloids Surf. B Biointerfaces 2013, 102, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.Y.; Yang, M.C. Surface immobilization of chondroitin 6-sulfate/heparin multilayer on stainless steel for developing drug-eluting coronary stents. Colloids Surf. B Biointerfaces 2008, 61, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Humpolicek, P.; Kucekova, Z.; Kasparkova, V.; Pelkova, J.; Modic, M.; Junkar, I.; Trchova, M.; Bober, P.; Stejskal, J.; Lehocky, M. Blood coagulation and platelet adhesion on polyaniline films. Colloids Surf. B Biointerfaces 2015, 133, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Wijesinghe, W.A.J.P.; Jeon, Y.J. Biological activities and potential industrial applications of fucose rich sulfated polysaccharides and fucoidans isolated from brown seaweeds: A review. Carbohydr. Polym. 2012, 88, 13–20. [Google Scholar] [CrossRef]
- Friedrich, J. Polymer surface modification with monosort functional groups. In The Plasma Chemistry of Polymer Surfaces: Advanced Techniques for Surface Design; Wiley-VCH: Weinheim, Germany, 2012; pp. 249–302. [Google Scholar]





| Samples | PE | PEH | PEF | PET | PETH | PETF |
|---|---|---|---|---|---|---|
| θw (°) | 85.3 (±3.4) | 81.9 (±12.2) | 79.4 (±8.3) | 56.9 (±11) | 79.6 (±5.3) | 59.1 (±9) |
| Ra (nm) | 24.2 | 13.9 | 20.3 | 46.7 | 17.9 | 24 |
| Samples | C1s% | O1s% | N1s% | S2p% | O1s/C1s | N1s/C1s | S2p/C1s |
|---|---|---|---|---|---|---|---|
| PE | 98.7 | 1.3 | - | - | 0.013 | - | - |
| PEH | 98.6 | 1.4 | - | - | 0.014 | - | - |
| PEF | 98.7 | 1.3 | - | - | 0.013 | - | - |
| PET | 87.2 | 11.7 | 1.1 | - | 0.134 | 0.013 | - |
| PETH | 85.7 | 13.3 | 0.8 | 0.2 | 0.155 | 0.009 | 0.0023 |
| PETF | 82.3 | 14.8 | 0.5 | 2.4 | 0.18 | 0.006 | 0.0292 |
| Samples | PT (S) | aPTT (S) | TT (S) |
|---|---|---|---|
| PE (Reference) | 11.5 | 24.8 | 15.9 |
| PEH | 11.5 | 25 | 16.5 |
| PEF | 11.2 | 24.1 | 16.8 |
| PET | 11.4 | 25.9 | 16.8 |
| PETH | 11.5 | 25.7 | 16.6 |
| PETF | 10.9 | 27.3 | 20.9 |
| PETA | 11.5 | 25.2 | 16.3 |
| PETAH | 11.6 | 26.5 | 17.2 |
| PETAF | 11.1 | 26.5 | 18 |
| PETM | 11.7 | 26.4 | 16.9 |
| PETMH | 11.4 | 25.2 | 16.7 |
| PETMF | 11 | 24.2 | 16.5 |
| PETD | 11.4 | 24.2 | 16.6 |
| PETDH | 11.4 | 24.1 | 16.5 |
| PETDF | 11 | 27.1 | 19.5 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozaltin, K.; Lehocký, M.; Humpolíček, P.; Pelková, J.; Sáha, P. A New Route of Fucoidan Immobilization on Low Density Polyethylene and Its Blood Compatibility and Anticoagulation Activity. Int. J. Mol. Sci. 2016, 17, 908. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17060908
Ozaltin K, Lehocký M, Humpolíček P, Pelková J, Sáha P. A New Route of Fucoidan Immobilization on Low Density Polyethylene and Its Blood Compatibility and Anticoagulation Activity. International Journal of Molecular Sciences. 2016; 17(6):908. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17060908
Chicago/Turabian StyleOzaltin, Kadir, Marián Lehocký, Petr Humpolíček, Jana Pelková, and Petr Sáha. 2016. "A New Route of Fucoidan Immobilization on Low Density Polyethylene and Its Blood Compatibility and Anticoagulation Activity" International Journal of Molecular Sciences 17, no. 6: 908. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17060908