Risk Factors for Myopia: A Review
Abstract
:1. Introduction
2. Methodology
3. Results
3.1. Genetic Factors
3.2. Environmental Factors
3.2.1. Education and Near Work
3.2.2. Time Outdoors and Light Exposure
3.2.3. Life Environment
3.2.4. Digital Screen Time
| Relationship | Main Findings | Related Factors | |
|---|---|---|---|
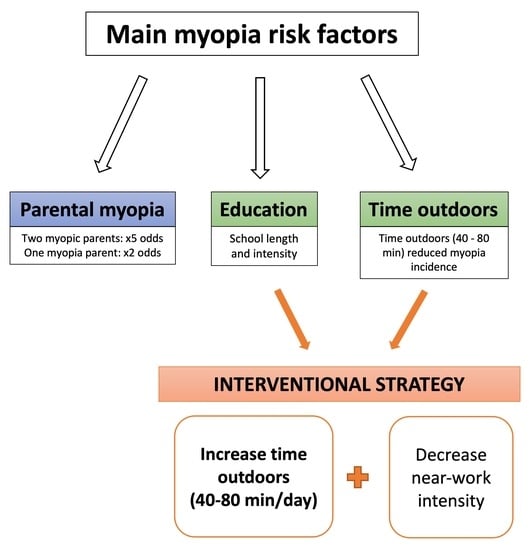
| Parental myopia | Strong | Two myopic parents: ×5 odds * [26,27] One myopia parent: ×2 odds * [26,27] | Gene–environment interaction |
| Education | Strong | School length and the performance intensity associated [48,49,50,51] | Near work Accommodative lag |
| Near work | Moderate | Continuous reading (>30 min): ×1.5 odds * [62] Closer reading distance (<30 cm): ×2.5 odds * [62] | Education Accommodative lag |
| Time outdoors | Strong | Time outdoors between 40–80 min associated with reduced myopia incidence [87,91,92,93] | Light exposure, dopamine release, vitamin D, and increased depth of field |
| Light exposure | Moderate | Slower axial elongation is associated with greater daily light exposure (>3000 lux) [85,98] | Dopamine release, vitamin D, and increased depth of field |
| Life environment | Weak | Higher myopia prevalence in urban environments [44,102,103,104,105] | Education, near work, and time outdoors |
| Digital screen | Weak | Prolonged screen time: ×4–8 odds * [114,117] | Near work and time outdoors |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wallman, J.; Winawer, J. Homeostasis of Eye Growth and the Question of Myopia. Neuron 2004, 43, 447–468. [Google Scholar] [CrossRef]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Fan, D.S.; Lai, C.; Lau, H.H.; Cheung, E.Y.; Lam, D.S. Change in Vision Disorders among Hong Kong Preschoolers in 10 Years. Clin. Exp. Ophthalmol. 2011, 39, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Qu, X.; Zhu, X.; Xu, X.; Zhu, J.; Sankaridurg, P.; Lin, S.; Lu, L.; Zhao, R.; Wang, L.; et al. Age-Specific Prevalence of Visual Impairment and Refractive Error in Children Aged 3-10 Years in Shanghai, China. Investig. Ophthalmol. Vis. Sci. 2016, 57, 6188–6196. [Google Scholar] [CrossRef] [PubMed]
- Quek, T.P.L.; Chua, C.G.; Chong, C.S.; Chong, J.H.; Hey, H.W.; Lee, J.; Lim, Y.F.; Saw, S.M. Prevalence of Refractive Errors in Teenage High School Students in Singapore. Ophthalmic Physiol. Opt. 2004, 24, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.M.; Bertelsen, G.; Cumberland, P.; Wolfram, C.; Verhoeven, V.J.M.; Anastasopoulos, E.; Buitendijk, G.H.S.; Cougnard-Grégoire, A.; Creuzot-Garcher, C.; Erke, M.G.; et al. Increasing Prevalence of Myopia in Europe and the Impact of Education. Ophthalmology 2015, 122, 1489–1497. [Google Scholar] [CrossRef]
- Czepita, D.; Zejmo, M.; Mojsa, A. Prevalence of Myopia and Hyperopia in a Population of Polish Schoolchildren. Ophthalmic Physiol. Opt. 2007, 27, 60–65. [Google Scholar] [CrossRef]
- Pärssinen, O. The Increased Prevalence of Myopia in Finland. Acta Ophthalmol. 2012, 90, 497–502. [Google Scholar] [CrossRef]
- McCullough, S.J.; O’Donoghue, L.; Saunders, K.J. Six Year Refractive Change among White Children and Young Adults: Evidence for Significant Increase in Myopia among White UK Children. PLoS ONE 2016, 11, e0146332. [Google Scholar] [CrossRef]
- Morgan, I.G.; Rose, K.A. Myopia and International Educational Performance. Ophthalmic Physiol. Opt. 2013, 33, 329–338. [Google Scholar] [CrossRef]
- Morgan, I.G.; French, A.N.; Ashby, R.S.; Guo, X.; Ding, X.; He, M.; Rose, K.A. The Epidemics of Myopia: Aetiology and Prevention. Prog. Retin. Eye Res. 2018, 62, 134–149. [Google Scholar] [CrossRef]
- Alvarez-Peregrina, C.C.; Sanchez-Tena, M.A.M.A.; Martinez-Perez, C.C.; Villa-Collar, C.C. Prevalence and Risk Factors of Myopia in Spain. J. Ophthalmol. 2019, 2019, 3419576. [Google Scholar] [CrossRef]
- Iribarren, R.; Cortinez, M.F.; Chiappe, J.P. Age of First Distance Prescription and Final Myopic Refractive Error. Ophthalmic Epidemiol. 2009, 16, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Chua, S.Y.L.; Sabanayagam, C.; Cheung, Y.B.; Chia, A.; Valenzuela, R.K.; Tan, D.; Wong, T.Y.; Cheng, C.Y.; Saw, S.M. Age of Onset of Myopia Predicts Risk of High Myopia in Later Childhood in Myopic Singapore Children. Ophthalmic Physiol. Opt. 2016, 36, 388–394. [Google Scholar] [CrossRef]
- Bourne, R.R.A.; Stevens, G.A.; White, R.A.; Smith, J.L.; Flaxman, S.R.; Price, H.; Jonas, J.B.; Keeffe, J.; Leasher, J.; Naidoo, K.; et al. Causes of Vision Loss Worldwide, 1990-2010: A Systematic Analysis. Lancet Glob. Health 2013, 1, e339–e349. [Google Scholar] [CrossRef] [PubMed]
- Fricke, T.R.; Holden, B.A.; Wilson, D.A.; Schlenther, G.; Naidoo, K.S.; Resnikoff, S.; Frick, K.D. Global Cost of Correcting Vision Impairment from Uncorrected Refractive Error. Bull. World Health Organ. 2012, 90, 728–738. [Google Scholar] [CrossRef] [PubMed]
- Flitcroft, D.I. The Complex Interactions of Retinal, Optical and Environmental Factors in Myopia Aetiology. Prog. Retin. Eye Res. 2012, 31, 622–660. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.H.; Chen, R.I.; Lin, S.C. Myopia and Glaucoma: Sorting out the Difference. Curr. Opin. Ophthalmol. 2015, 26, 90–95. [Google Scholar] [CrossRef]
- Mukesh, B.N.; Le, A.; Dimitrov, P.N.; Ahmed, S.; Taylor, H.R.; McCarty, C.A. Development of Cataract and Associated Risk Factors: The Visual Impairment Project. Arch. Ophthalmol. 2006, 124, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.M.; Chang, D.S.T.; Wu, P.C. The Association between Near Work Activities and Myopia in Children-A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0140419. [Google Scholar] [CrossRef]
- Xiong, S.; Sankaridurg, P.; Naduvilath, T.; Zang, J.; Zou, H.; Zhu, J.; Lv, M.; He, X.; Xu, X. Time Spent in Outdoor Activities in Relation to Myopia Prevention and Control: A Meta-Analysis and Systematic Review. Acta Ophthalmol. 2017, 95, 551–566. [Google Scholar] [CrossRef]
- Verhoeven, V.J.M.; Buitendijk, G.H.S.; Rivadeneira, F.; Uitterlinden, A.G.; Vingerling, J.R.; Hofman, A.; Klaver, C.C.W. Education Influences the Role of Genetics in Myopia. Eur. J. Epidemiol. 2013, 28, 973–980. [Google Scholar] [CrossRef] [PubMed]
- Saw, S.M.; Javier Nieto, F.; Katz, J.; Schein, O.D.; Levy, B.; Chew, S.J. Familial Clustering and Myopia Progression in Singapore School Children. Ophthalmic Epidemiol. 2001, 8, 227–236. [Google Scholar] [CrossRef]
- Mutti, D.; Mitchell, G.; Moeschberger, M.L.; Jones, L.A.; Zadnik, K. Parental Myopia, near Work, School Achievement, and Children’s Refractive Error. Investig. Ophthalmol. Vis. Sci. 2002, 43, 3633–3640. [Google Scholar]
- Saw, S.M.; Shankar, A.; Tan, S.B.; Taylor, H.; Tan, D.T.H.; Stone, R.A.; Wong, T.Y. A Cohort Study of Incident Myopia in Singaporean Children. Investig. Ophthalmol. Vis. Sci. 2006, 47, 1839–1844. [Google Scholar] [CrossRef]
- Ip, J.M.; Huynh, S.C.; Robaei, D.; Rose, K.A.; Morgan, I.G.; Smith, W.; Kifley, A.; Mitchell, P. Ethnic Differences in the Impact of Parental Myopia: Findings from a Population-Based Study of 12-Year-Old Australian Children. Investig. Ophthalmol. Vis. Sci. 2007, 48, 2520–2528. [Google Scholar] [CrossRef]
- Jones, L.A.; Sinnott, L.T.; Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Zadnik, K. Parental History of Myopia, Sports and Outdoor Activities, and Future Myopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 3524–3532. [Google Scholar] [CrossRef] [PubMed]
- Lyhne, N.; Sjølie, A.K.; Kyvik, K.O.; Green, A. The Importance of Genes and Environment for Ocular Refraction and Its Determiners: A Population Based Study among 20-45 Year Old Twins. Br. J. Ophthalmol. 2001, 85, 1470–1476. [Google Scholar] [CrossRef] [PubMed]
- Dirani, M.; Chamberlain, M.; Shekar, S.N.; Islam, A.F.M.; Garoufalis, P.; Chen, C.Y.; Guymer, R.H.; Baird, P.N. Heritability of Refractive Error and Ocular Biometrics: The Genes in Myopia (GEM) Twin Study. Investig. Ophthalmol. Vis. Sci. 2006, 47, 4756–4761. [Google Scholar] [CrossRef] [PubMed]
- Klein, A.P.; Suktitipat, B.; Duggal, P.; Lee, K.E.; Klein, R.; Bailey-Wilson, J.E.; Klein, B.E.K. Heritability Analysis of Spherical Equivalent, Axial Length, Corneal Curvature, and Anterior Chamber Depth in the Beaver Dam Eye Study. Arch. Ophthalmol. 2009, 127, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Zhu, G.; Hewitt, A.W.; Ruddle, J.B.; Kearns, L.S.; Brown, S.A.; MacKinnon, J.R.; Chen, C.Y.; Hammond, C.J.; Craig, J.E.; Montgomery, G.W.; et al. Genetic Dissection of Myopia: Evidence for Linkage of Ocular Axial Length to Chromosome 5q. Ophthalmology 2008, 115, 1053–1057.e2. [Google Scholar] [CrossRef]
- Tedja, M.S.; Wojciechowski, R.; Hysi, P.G.; Eriksson, N.; Furlotte, N.A.; Verhoeven, V.J.M.; Iglesias, A.I.; Meester-Smoor, M.A.; Tompson, S.W.; Fan, Q.; et al. Genome-Wide Association Meta-Analysis Highlights Light-Induced Signaling as a Driver for Refractive Error. Nat. Genet. 2018, 50, 834–848. [Google Scholar] [CrossRef]
- Kiefer, A.K.; Tung, J.Y.; Do, C.B.; Hinds, D.A.; Mountain, J.L.; Francke, U.; Eriksson, N. Genome-Wide Analysis Points to Roles for Extracellular Matrix Remodeling, the Visual Cycle, and Neuronal Development in Myopia. PLoS Genet. 2013, 9, e1003299. [Google Scholar] [CrossRef] [PubMed]
- Verhoeven, V.J.M.; Hysi, P.G.; Wojciechowski, R.; Fan, Q.; Guggenheim, J.A.; Höhn, R.; Macgregor, S.; Hewitt, A.W.; Nag, A.; Cheng, C.Y.; et al. Genome-Wide Meta-Analyses of Multiancestry Cohorts Identify Multiple New Susceptibility Loci for Refractive Error and Myopia. Nat. Genet. 2013, 45, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Wojciechowski, R.; Yee, S.S.; Simpson, C.L.; Bailey-Wilson, J.E.; Stambolian, D. Matrix Metalloproteinases and Educational Attainment in Refractive Error: Evidence of Gene-Environment Interactions in the Age-Related Eye Disease Study. Ophthalmology 2013, 120, 298–305. [Google Scholar] [CrossRef]
- Fan, Q.; Verhoeven, V.J.M.; Wojciechowski, R.; Barathi, V.A.; Hysi, P.G.; Guggenheim, J.A.; Hohn, R.; Vitart, V.; Khawaja, A.P.; Yamashiro, K.; et al. Meta-Analysis of Gene-Environment-Wide Association Scans Accounting for Education Level Identifies Additional Loci for Refractive Error. Nat. Commun. 2016, 7, 11008. [Google Scholar] [CrossRef]
- Biggin, A.; Holman, K.; Brett, M.; Bennetts, B.; Adès, L. Detection of Thirty Novel FBN1 Mutations in Patients with Marfan Syndrome or a Related Fibrillinopathy. Hum. Mutat. 2004, 23, 99. [Google Scholar] [CrossRef] [PubMed]
- Menzel, O.; Bekkeheien, R.C.J.; Reymond, A.; Fukai, N.; Boye, E.; Kosztolanyi, G.; Aftimos, S.; Deutsch, S.; Scott, H.S.; Olsen, B.R.; et al. Knobloch Syndrome: Novel Mutations in COL18A1, Evidence for Genetic Heterogeneity, and a Functionally Impaired Polymorphism in Endostatin. Hum. Mutat. 2004, 23, 77–84. [Google Scholar] [CrossRef]
- Pusch, C.M.; Zeitz, C.; Brandau, O.; Pesch, K.; Achatz, H.; Feil, S.; Scharfe, C.; Maurer, J.; Jacobi, F.K.; Pinckers, A.; et al. The Complete Form of X-Linked Congenital Stationary Night Blindness Is Caused by Mutations in a Gene Encoding a Leucine-Rich Repeat Protein. Nat. Genet. 2000, 26, 324–327. [Google Scholar] [CrossRef]
- Naiglin, L.; Gazagne, C.; Dallongeville, F.; Thalamas, C.; Idder, A.; Rascol, O.; Malecaze, F.; Calvas, P. A Genome Wide Scan for Familial High Myopia Suggests a Novel Locus on Chromosome 7q36. J. Med. Genet. 2002, 39, 118–124. [Google Scholar] [CrossRef]
- Paluru, P.; Ronan, S.M.; Heon, E.; Devoto, M.; Wildenberg, S.C.; Scavello, G.; Holleschau, A.; Mäkitie, O.; Cole, W.G.; King, R.A.; et al. New Locus for Autosomal Dominant High Myopia Maps to the Long Arm of Chromosome 17. Investig. Ophthalmol. Vis. Sci. 2003, 44, 1830–1836. [Google Scholar] [CrossRef] [PubMed]
- Lam, D.S.C.; Lee, W.S.; Leung, Y.F.; Tam, P.O.S.; Fan, D.S.P.; Fan, B.J.; Pang, C.P. TGFbeta-Induced Factor: A Candidate Gene for High Myopia. Investig. Ophthalmol. Vis. Sci. 2003, 44, 1012–1015. [Google Scholar] [CrossRef]
- Ip, J.M.; Rose, K.A.; Morgan, I.G.; Burlutsky, G.; Mitchell, P. Myopia and the Urban Environment: Findings in a Sample of 12-Year-Old Australian School Children. Investig. Ophthalmol. Vis. Sci. 2008, 49, 3858–3863. [Google Scholar] [CrossRef] [PubMed]
- Uzma, N.; Kumar, B.S.; Salar, B.M.K.M.; Zafar, M.A.; Reddy, V.D. A Comparative Clinical Survey of the Prevalence of Refractive Errors and Eye Diseases in Urban and Rural School Children. Can. J. Ophthalmol. 2009, 44, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Li, L.; Chen, L.; Lee, J.; Wu, J.; Yang, A.; Chen, C.; Xu, D.; Lam, D.S.C.; Sharma, A.; et al. Population Density and Refractive Error among Chinese Children. Investig. Ophthalmol. Vis. Sci. 2010, 51, 4969–4976. [Google Scholar] [CrossRef]
- Shimizu, N.; Nomura, H.; Ando, F.; Niino, N.; Miyake, Y.; Shimokata, H. Refractive Errors and Factors Associated with Myopia in an Adult Japanese Population. Jpn. J. Ophthalmol. 2003, 47, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Mirshahi, A.; Ponto, K.A.; Hoehn, R.; Zwiener, I.; Zeller, T.; Lackner, K.; Beutel, M.E.; Pfeiffer, N. Myopia and Level of Education: Results from the Gutenberg Health Study. Ophthalmology 2014, 121, 2047–2052. [Google Scholar] [CrossRef] [PubMed]
- Koh, V.; Yang, A.; Saw, S.M.; Chan, Y.H.; Lin, S.T.; Tan, M.M.H.; Tey, F.; Nah, G.; Ikram, M.K. Differences in Prevalence of Refractive Errors in Young Asian Males in Singapore between 1996-1997 and 2009–2010. Ophthalmic Epidemiol. 2014, 21, 247–255. [Google Scholar] [CrossRef]
- Wu, J.F.; Bi, H.S.; Wang, S.M.; Hu, Y.Y.; Wu, H.; Sun, W.; Lu, T.L.; Wang, X.R.; Jonas, J.B. Refractive Error, Visual Acuity and Causes of Vision Loss in Children in Shandong, China. The Shandong Children Eye Study. PLoS ONE 2013, 8, e82763. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.H.; Liu, Y.L.; Ma, I.H.; Su, C.C.; Lin, C.W.; Lin, L.L.K.; Hsiao, C.K.; Wang, I.J. Evolution of the Prevalence of Myopia among Taiwanese Schoolchildren: A Review of Survey Data from 1983 through 2017. Ophthalmology 2021, 128, 290–301. [Google Scholar] [CrossRef]
- Plotnikov, D.; Williams, C.; Atan, D.; Davies, N.M.; Mojarrad, N.G.; Guggenheim, J.A. Effect of Education on Myopia: Evidence from the United Kingdom ROSLA 1972 Reform. Investig. Ophthalmol. Vis. Sci. 2020, 61, 7. [Google Scholar] [CrossRef] [PubMed]
- Saw, S.M.; Cheng, A.; Fong, A.; Gazzard, G.; Tan, D.T.H.; Morgan, I. School Grades and Myopia. Ophthalmic Physiol. Opt. 2007, 27, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Saw, S.M.; Tan, S.B.; Fung, D.; Chia, K.S.; Koh, D.; Tan, D.T.H.; Stone, R.A. IQ and the Association with Myopia in Children. Investig. Ophthalmol. Vis. Sci. 2004, 45, 2943–2948. [Google Scholar] [CrossRef]
- Saw, S.M.; Chia, K.S.; Wu, H.M.; Seet, B.; Yap, E.; Lee, L.; Wong, T.Y.; Stone, R.A. Academic Achievement, Close up Work Parameters, and Myopia in Singapore Military Conscripts. Br. J. Ophthalmol. 2001, 85, 855–860. [Google Scholar] [CrossRef] [PubMed]
- Ku, P.W.; Steptoe, A.; Lai, Y.J.; Hu, H.Y.; Chu, D.; Yen, Y.F.; Liao, Y.; Chen, L.J. The Associations between Near Visual Activity and Incident Myopia in Children: A Nationwide 4-Year Follow-up Study. Ophthalmology 2019, 126, 214–220. [Google Scholar] [CrossRef]
- Bez, D.; Megreli, J.; Bez, M.; Avramovich, E.; Barak, A.; Levine, H. Association Between Type of Educational System and Prevalence and Severity of Myopia Among Male Adolescents in Israel. JAMA Ophthalmol. 2019, 137, 887–893. [Google Scholar] [CrossRef] [PubMed]
- Saw, S.M.; Chua, W.H.; Hong, C.Y.; Wu, H.M.; Chan, W.Y.; Chia, K.S.; Stone, R.A.; Tan, D. Nearwork in Early-Onset Myopia. Investig. Ophthalmol. Vis. Sci. 2002, 43, 332–339. [Google Scholar]
- French, A.N.; Morgan, I.G.; Mitchell, P.; Rose, K.A. Risk Factors for Incident Myopia in Australian Schoolchildren: The Sydney Adolescent Vascular and Eye Study. Ophthalmology 2013, 120, 2100–2108. [Google Scholar] [CrossRef]
- Guo, L.; Yang, J.; Mai, J.; Du, X.; Guo, Y.; Li, P.; Yue, Y.; Tang, D.; Lu, C.; Zhang, W.H. Prevalence and Associated Factors of Myopia among Primary and Middle School-Aged Students: A School-Based Study in Guangzhou. Eye (Lond.) 2016, 30, 796–804. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Vasudevan, B.; Mao, G.Y.; Ciuffreda, K.J.; Jhanji, V.; Li, X.X.; Zhou, H.J.; Wang, N.L.; Liang, Y.B. The Influence of near Work on Myopic Refractive Change in Urban Students in Beijing: A Three-Year Follow-up Report. Graefes Arch. Clin. Exp. Ophthalmol. 2016, 254, 2247–2255. [Google Scholar] [CrossRef]
- Hsu, C.C.; Huang, N.; Lin, P.Y.; Fang, S.Y.; Tsai, D.C.; Chen, S.Y.; Tsai, C.Y.; Woung, L.C.; Chiou, S.H.; Liu, C.J.L. Risk Factors for Myopia Progression in Second-Grade Primary School Children in Taipei: A Population-Based Cohort Study. Br. J. Ophthalmol. 2017, 101, 1611–1617. [Google Scholar] [CrossRef] [PubMed]
- Ip, J.M.; Saw, S.M.; Rose, K.A.; Morgan, I.G.; Kifley, A.; Wang, J.J.; Mitchell, P. Role of near Work in Myopia: Findings in a Sample of Australian School Children. Investig. Ophthalmol. Vis. Sci. 2008, 49, 2903–2910. [Google Scholar] [CrossRef] [PubMed]
- Pärssinen, O.; Kauppinen, M. Risk Factors for High Myopia: A 22-Year Follow-up Study from Childhood to Adulthood. Acta Ophthalmol. 2019, 97, 510–518. [Google Scholar] [CrossRef]
- Guggenheim, J.A.; Northstone, K.; McMahon, G.; Ness, A.R.; Deere, K.; Mattocks, C.; St. Pourcain, B.; Williams, C. Time Outdoors and Physical Activity as Predictors of Incident Myopia in Childhood: A Prospective Cohort Study. Investig. Ophthalmol. Vis. Sci. 2012, 53, 2856–2865. [Google Scholar] [CrossRef]
- Saw, S.M.; Nieto, F.J.; Katz, J.; Schein, O.D.; Levy, B.; Chew, S.J. Factors Related to the Progression of Myopia in Singaporean Children. Optom. Vis. Sci. 2000, 77, 549–554. [Google Scholar] [CrossRef]
- Jones-Jordan, L.A.; Sinnott, L.T.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Mutti, D.O.; Daniel Twelker, J.; Zadnik, K. Time Outdoors, Visual Activity, and Myopia Progression in Juvenile-Onset Myopes. Investig. Ophthalmol. Vis. Sci. 2012, 53, 7169–7175. [Google Scholar] [CrossRef]
- Jones-Jordan, L.A.; Lynn Mitchell, G.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Mutti, D.O.; Daniel Twelker, J.; Sims, J.R.; Zadnik, K. Visual Activity before and after the Onset of Juvenile Myopia. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1841–1850. [Google Scholar] [CrossRef]
- Williams, C.; Miller, L.L.; Gazzard, G.; Saw, S.M. A Comparison of Measures of Reading and Intelligence as Risk Factors for the Development of Myopia in a UK Cohort of Children. Br. J. Ophthalmol. 2008, 92, 1117–1121. [Google Scholar] [CrossRef] [PubMed]
- Li, S.M.; Li, S.Y.; Kang, M.T.; Zhou, Y.; Liu, L.R.; Li, H.; Wang, Y.P.; Zhan, S.Y.; Gopinath, B.; Mitchell, P.; et al. Near Work Related Parameters and Myopia in Chinese Children: The Anyang Childhood Eye Study. PLoS ONE 2015, 10, e0134514. [Google Scholar] [CrossRef] [PubMed]
- Scheiman, M.; Zhang, Q.; Gwiazda, J.; Hyman, L.; Harb, E.; Weissberg, E.; Weise, K.K.; Dias, L. Visual Activity and Its Association with Myopia Stabilisation. Ophthalmic Physiol. Opt. 2014, 34, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Gwiazda, J.; Thorn, F.; Held, R. Accommodation, Accommodative Convergence, and Response AC/A Ratios before and at the Onset of Myopia in Children. Optom. Vis. Sci. 2005, 82, 273–278. [Google Scholar] [CrossRef]
- Harb, E.; Thorn, F.; Troilo, D. Characteristics of Accommodative Behavior during Sustained Reading in Emmetropes and Myopes. Vis. Res. 2006, 46, 2581–2592. [Google Scholar] [CrossRef]
- Langaas, T.; Riddell, P.M.; Svarverud, E.; Ystenæs, A.E.; Langeggen, I.; Bruenech, J.R. Variability of the Accommodation Response in Early Onset Myopia. Optom. Vis. Sci. 2008, 85, 37–48. [Google Scholar] [CrossRef]
- Schaeffel, F.; Troilo, D.; Wallman, J.; Howland, H.C. Developing Eyes That Lack Accommodation Grow to Compensate for Imposed Defocus. Vis. Neurosci. 1990, 4, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Wildsoet, C.F. Neural Pathways Subserving Negative Lens-Induced Emmetropization in Chicks--Insights from Selective Lesions of the Optic Nerve and Ciliary Nerve. Curr. Eye Res. 2003, 27, 371–385. [Google Scholar] [CrossRef]
- Choh, V.; Lew, M.J.Y.; Nadel, M.W.; Wildsoet, C.F. Effects of Interchanging Hyperopic Defocus and Form Deprivation Stimuli in Normal and Optic Nerve-Sectioned Chicks. Vis. Res. 2006, 46, 1070–1079. [Google Scholar] [CrossRef]
- Hung, L.F.; Crawford, M.L.J.; Smith, E.L. Spectacle Lenses Alter Eye Growth and the Refractive Status of Young Monkeys. Nat. Med. 1995, 1, 761–765. [Google Scholar] [CrossRef] [PubMed]
- Troilo, D.; Quinn, N.; Baker, K. Accommodation and Induced Myopia in Marmosets. Vis. Res. 2007, 47, 1228–1244. [Google Scholar] [CrossRef]
- Nakatsuka, C.; Hasebe, S.; Nonaka, F.; Ohtsuki, H. Accommodative Lag under Habitual Seeing Conditions: Comparison between Adult Myopes and Emmetropes. Jpn. J. Ophthalmol. 2003, 47, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Rosenfield, M.; Desai, R.; Portello, J.K. Do Progressing Myopes Show Reduced Accommodative Responses? Optom. Vis. Sci. 2002, 79, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Mutti, D.O.; Mitchell, G.L.; Hayes, J.R.; Jones, L.A.; Moeschberger, M.L.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.; Zadnik, K.; et al. Accommodative Lag before and after the Onset of Myopia. Investig. Ophthalmol. Vis. Sci. 2006, 47, 837–846. [Google Scholar] [CrossRef] [PubMed]
- Weizhong, L.; Zhikuan, Y.; Wen, L.; Xiang, C.; Jian, G. A Longitudinal Study on the Relationship between Myopia Development and near Accommodation Lag in Myopic Children. Ophthalmic Physiol. Opt. 2008, 28, 57–61. [Google Scholar] [CrossRef]
- Berntsen, D.A.; Sinnott, L.T.; Mutti, D.O.; Zadnik, K. Accommodative Lag and Juvenile-Onset Myopia Progression in Children Wearing Refractive Correction. Vis. Res. 2011, 51, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Koomson, N.Y.; Amedo, A.O.; Opoku-Baah, C.; Ampeh, P.B.; Ankamah, E.; Bonsu, K. Relationship between Reduced Accommodative Lag and Myopia Progression. Optom. Vis. Sci. 2016, 93, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Rose, K.A.; Morgan, I.G.; Ip, J.; Kifley, A.; Huynh, S.; Smith, W.; Mitchell, P. Outdoor Activity Reduces the Prevalence of Myopia in Children. Ophthalmology 2008, 115, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.C.; Tsai, C.L.; Hu, C.H.; Yang, Y.H. Effects of Outdoor Activities on Myopia among Rural School Children in Taiwan. Ophthalmic Epidemiol. 2010, 17, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.C.; Tsai, C.L.; Wu, H.L.; Yang, Y.H.; Kuo, H.K. Outdoor Activity during Class Recess Reduces Myopia Onset and Progression in School Children. Ophthalmology 2013, 120, 1080–1085. [Google Scholar] [CrossRef]
- Lu, B.; Congdon, N.; Liu, X.; Choi, K.; Lam, D.S.C.; Zhang, M.; Zheng, M.; Zhou, Z.; Li, L.; Liu, X.; et al. Associations between near Work, Outdoor Activity, and Myopia among Adolescent Students in Rural China: The Xichang Pediatric Refractive Error Study Report No. 2. Arch. Ophthalmol. 2009, 127, 769–775. [Google Scholar] [CrossRef]
- Low, W.; Dirani, M.; Gazzard, G.; Chan, Y.H.; Zhou, H.J.; Selvaraj, P.; Eong, K.G.A.; Young, T.L.; Mitchell, P.; Wong, T.Y.; et al. Family History, near Work, Outdoor Activity, and Myopia in Singapore Chinese Preschool Children. Br. J. Ophthalmol. 2010, 94, 1012–1016. [Google Scholar] [CrossRef]
- Shah, R.L.; Huang, Y.; Guggenheim, J.A.; Williams, C. Time Outdoors at Specific Ages During Early Childhood and the Risk of Incident Myopia. Investig. Ophthalmol. Vis. Sci. 2017, 58, 1158–1166. [Google Scholar] [CrossRef]
- Jin, J.X.; Hua, W.J.; Jiang, X.; Wu, X.Y.; Yang, J.W.; Gao, G.P.; Fang, Y.; Pei, C.L.; Wang, S.; Zhang, J.Z.; et al. Effect of Outdoor Activity on Myopia Onset and Progression in School-Aged Children in Northeast China: The Sujiatun Eye Care Study. BMC Ophthalmol. 2015, 15, 73. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Xiang, F.; Zeng, Y.; Mai, J.; Chen, Q.; Zhang, J.; Smith, W.; Rose, K.; Morgan, I.G. Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China: A Randomized Clinical Trial. JAMA 2015, 314, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.C.; Chen, C.T.; Lin, K.K.; Sun, C.C.; Kuo, C.N.; Huang, H.M.; Poon, Y.C.; Yang, M.L.; Chen, C.Y.; Huang, J.C.; et al. Myopia Prevention and Outdoor Light Intensity in a School-Based Cluster Randomized Trial. Ophthalmology 2018, 125, 1239–1250. [Google Scholar] [CrossRef]
- Öner, V.; Bulut, A.; Oruç, Y.; Özgür, G. Influence of Indoor and Outdoor Activities on Progression of Myopia during Puberty. Int. Ophthalmol. 2016, 36, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Pärssinen, O.; Kauppinen, M.; Viljanen, A. The Progression of Myopia from Its Onset at Age 8-12 to Adulthood and the Influence of Heredity and External Factors on Myopic Progression. A 23-Year Follow-up Study. Acta Ophthalmol. 2014, 92, 730–739. [Google Scholar] [CrossRef] [PubMed]
- Saxena, R.; Vashist, P.; Tandon, R.; Pandey, R.M.; Bhardawaj, A.; Gupta, V.; Menon, V. Incidence and Progression of Myopia and Associated Factors in Urban School Children in Delhi: The North India Myopia Study (NIM Study). PLoS ONE 2017, 12, e0189774. [Google Scholar] [CrossRef]
- French, A.N.; Ashby, R.S.; Morgan, I.G.; Rose, K.A. Time Outdoors and the Prevention of Myopia. Exp. Eye Res. 2013, 114, 58–68. [Google Scholar] [CrossRef] [PubMed]
- Read, S.A.; Collins, M.J.; Vincent, S.J. Light Exposure and Eye Growth in Childhood. Investig. Ophthalmol. Vis. Sci. 2015, 56, 6779–6787. [Google Scholar] [CrossRef]
- Feldkaemper, M.; Schaeffel, F. An Updated View on the Role of Dopamine in Myopia. Exp. Eye Res. 2013, 114, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Mutti, D.O.; Marks, A.R. Blood Levels of Vitamin D in Teens and Young Adults with Myopia. Optom. Vis. Sci. 2011, 88, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Tideman, J.W.L.; Polling, J.R.; Voortman, T.; Jaddoe, V.W.V.; Uitterlinden, A.G.; Hofman, A.; Vingerling, J.R.; Franco, O.H.; Klaver, C.C.W. Low Serum Vitamin D Is Associated with Axial Length and Risk of Myopia in Young Children. Eur. J. Epidemiol. 2016, 31, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Saw, S.M.; Hong, R.Z.; Zhang, M.Z.; Fu, Z.F.; Ye, M.; Tan, D.; Chew, S.J. Near-Work Activity and Myopia in Rural and Urban Schoolchildren in China. J. Pediatr. Ophthalmol. Strabismus 2001, 38, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Dandona, R.; Dandona, L.; Srinivas, M.; Giridhar, P.; McCarty, C.A.; Rao, G.N. Population-Based Assessment of Refractive Error in India: The Andhra Pradesh Eye Disease Study. Clin. Exp. Ophthalmol. 2002, 30, 84–93. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Huang, W.; Zheng, Y.; Huang, L.; Ellwein, L.B. Refractive Error and Visual Impairment in School Children in Rural Southern China. Ophthalmology 2007, 114, 374–382. [Google Scholar] [CrossRef]
- Gao, Z.; Meng, N.; Muecke, J.; Chan, W.O.; Piseth, H.; Kong, A.; Jnguyenphamhh, T.; Dehghan, Y.; Selva, D.; Casson, R.; et al. Refractive Error in School Children in an Urban and Rural Setting in Cambodia. Ophthalmic Epidemiol. 2012, 19, 16–22. [Google Scholar] [CrossRef]
- He, M.; Zheng, Y.; Xiang, F. Prevalence of Myopia in Urban and Rural Children in Mainland China. Optom. Vis. Sci. 2009, 86, 40–44. [Google Scholar] [CrossRef]
- Shih, Y.F.; Chiang, T.H.; Hsiao, C.K.; Chen, C.J.; Hung, P.T.; Lin, L.L.K. Comparing Myopic Progression of Urban and Rural Taiwanese Schoolchildren. Jpn. J. Ophthalmol. 2010, 54, 446–451. [Google Scholar] [CrossRef]
- Sperduto, R.D.; Seigel, D.; Roberts, J.; Rowland, M. Prevalence of Myopia in the United States. Arch. Ophthalmol. 1983, 101, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.Y.; Mok, A.Y.T.; Do, C.-w.; Lee, P.H.; Chan, H.H.-l. The Diversified Defocus Profile of the Near-Work Environment and Myopia Development. Ophthalmic Physiol. Opt. 2020, 40, 463–471. [Google Scholar] [CrossRef]
- Guo, Y.; Liu, L.J.; Xu, L.; Lv, Y.Y.; Tang, P.; Feng, Y.; Meng, M.; Jonas, J.B. Outdoor Activity and Myopia among Primary Students in Rural and Urban Regions of Beijing. Ophthalmology 2013, 120, 277–283. [Google Scholar] [CrossRef]
- Choi, K.Y.; Yu, W.Y.; Lam, C.H.I.; Li, Z.C.; Chin, M.P.; Lakshmanan, Y.; Wong, F.S.Y.; Do, C.W.; Lee, P.H.; Chan, H.H.L. Childhood Exposure to Constricted Living Space: A Possible Environmental Threat for Myopia Development. Ophthalmic Physiol. Opt. 2017, 37, 568–575. [Google Scholar] [CrossRef]
- Read, S.A.; Vincent, S.J.; Tan, C.S.; Ngo, C.; Collins, M.J.; Saw, S.M. Patterns of Daily Outdoor Light Exposure in Australian and Singaporean Children. Transl. Vis. Sci. Technol. 2018, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Rose, K.A.; Morgan, I.G.; Smith, W.; Burlutsky, G.; Mitchell, P.; Saw, S.M. Myopia, Lifestyle, and Schooling in Students of Chinese Ethnicity in Singapore and Sydney. Arch. Ophthalmol. 2008, 126, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Saxena, R.; Vashist, P.; Tandon, R.; Pandey, R.M.; Bhardawaj, A.; Menon, V.; Mani, K. Prevalence of Myopia and Its Risk Factors in Urban School Children in Delhi: The North India Myopia Study (NIM Study). PLoS ONE 2015, 10, e0117349. [Google Scholar] [CrossRef]
- Harrington, S.C.; Stack, J.; O’dwyer, V. Risk Factors Associated with Myopia in Schoolchildren in Ireland. Br. J. Ophthalmol. 2019, 103, 1803–1809. [Google Scholar] [CrossRef]
- Hansen, M.H.; Laigaard, P.P.; Olsen, E.M.; Skovgaard, A.M.; Larsen, M.; Kessel, L.; Munch, I.C. Low Physical Activity and Higher Use of Screen Devices Are Associated with Myopia at the Age of 16-17 Years in the CCC2000 Eye Study. Acta Ophthalmol. 2020, 98, 315–321. [Google Scholar] [CrossRef]
- Singh, N.K.; James, R.M.; Yadav, A.; Kumar, R.; Asthana, S.; Labani, S. Prevalence of Myopia and Associated Risk Factors in Schoolchildren in North India. Optom. Vis. Sci. 2019, 96, 200–205. [Google Scholar] [CrossRef]
- McCrann, S.; Flitcroft, I.; Lalor, K.; Butler, J.; Bush, A.; Loughman, J. Parental Attitudes to Myopia: A Key Agent of Change for Myopia Control? Ophthalmic Physiol. Opt. 2018, 38, 298–308. [Google Scholar] [CrossRef]
- Liu, S.; Ye, S.; Xi, W.; Zhang, X. Electronic Devices and Myopic Refraction among Children Aged 6-14 Years in Urban Areas of Tianjin, China. Ophthalmic Physiol. Opt. 2019, 39, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Terasaki, H.; Yamashita, T.; Yoshihara, N.; Kii, Y.; Sakamoto, T. Association of Lifestyle and Body Structure to Ocular Axial Length in Japanese Elementary School Children. BMC Ophthalmol. 2017, 17, 123. [Google Scholar] [CrossRef]
- Dirani, M.; Crowston, J.G.; Wong, T.Y. From Reading Books to Increased Smart Device Screen Time. Br. J. Ophthalmol. 2019, 103, 1. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Study types | Articles, reviews, systematic reviews, and clinical trials | Studies with animals, case reports or books |
| Publication year | January 2000–May 2023 | Before 2000 |
| Age | Children and teenagers 5–30 years * | Adults Older than 30 years |
| Ethnicity | Caucasian and Asian | Others |
| Language | English | Other languages |
| Accessibility | Full-text available online | Full-text non-available online |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Albert, N.; Bueno-Gimeno, I.; Gené-Sampedro, A. Risk Factors for Myopia: A Review. J. Clin. Med. 2023, 12, 6062. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12186062
Martínez-Albert N, Bueno-Gimeno I, Gené-Sampedro A. Risk Factors for Myopia: A Review. Journal of Clinical Medicine. 2023; 12(18):6062. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12186062
Chicago/Turabian StyleMartínez-Albert, Noelia, Inmaculada Bueno-Gimeno, and Andrés Gené-Sampedro. 2023. "Risk Factors for Myopia: A Review" Journal of Clinical Medicine 12, no. 18: 6062. https://0-doi-org.brum.beds.ac.uk/10.3390/jcm12186062