Fungal Vaccine Development: State of the Art and Perspectives Using Immunoinformatics
Abstract
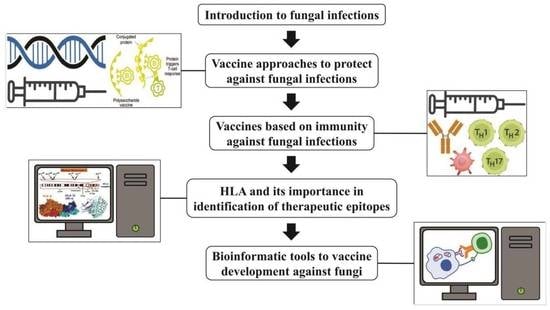
:1. Introduction
2. Vaccine Approaches to Protect against Fungal Infections
2.1. Inactivated and Live-Attenuated Vaccines
| Target Pathogen | Antigen/Strain | Adjuvant/Carrier/Vehicle | Vaccine Type | Model | Route of Injection | Human Clinical Trial | Reference(s) |
|---|---|---|---|---|---|---|---|
| Paracoccidioidomycosis (PCM) | P. brasiliensis | Nd | Inactivated/Live attenuated | Mice | - | Nd | [6] |
| Major 43-kDa antigenic glycoprotein (gp43), (P10) | Plasmid vector | DNA Vaccine | Mice | Intramuscular/Intradermal | - | [16] | |
| Mycobacterium leprae derived HSP65 | Vector pVAX1/ | Recombinant DNA | Mice | Intramuscular | - | [17] | |
| Major 43-kDa antigenic glycoprotein (gp43), (P10) | Plasmid vector/IL-12 recombinant | DNA Vaccine | Mice | Intratracheal | - | [18] | |
| Major 43-kDa antigenic glycoprotein (gp43), (P10) | S. cerevisiae expressing gp43 | Recombinant protein | Mice | Intraperitoneal | - | [19] | |
| P10- FliC fusion protein | Freund adjuvant (CFA)/multiple-antigen peptide (MAP) | Recombinant protein | Mice | Intranasal | - | [20] | |
| Recombinant rPb27 | Corynebacterium parvum/aluminum | Recombinant protein | Mice | Subcutaneous | - | [21] | |
| Heat shock protein 60 (HSP60) | Monophosphoryl lipid A, synthetic trehalose dicorynomycolate, and cell wall skeleton | Recombinant protein | Mice | Subcutaneous | - | [22] | |
| Panfungal | β-glucans of S. cerevisiae | Nd | Heat Killed Yeast (HKY) | Mice | Subcutaneous | Nd | [23] |
| Coccidioidomycosis | Formalin Killed Spherules (FKS) | Nd | Whole organism/Inactivated | Human | Intramuscular | Phase 3 | [12] |
| Antigen 2 (Ag2) | Nd | DNA vaccine | Mice | Intraperitoneal | - | [24] | |
| Coccidioides posadasii CPS1 Deletion Mutant | rAg2/PRA1–106-CSA with MPL-SE (25 μg)/CpG (10 μg) adjuvant | Whole organism/Live-attenuated | Mice | Subcutaneous/Intraperitoneal | - | [14] | |
| Δcts2/ard1/cts3 or ΔT—triple attenuated vaccine | Nd | Whole organism/Live-attenuated | Mice | Subcutaneous | - | [13] | |
| Recombinant Coccidioides polypeptide antigen (rCpa1) encapsulated into glucan-chitin particles (GCP-rCpa1) | Mouse serum albumin (MSA) and incomplete Freund’s adjuvant | Recombinant protein | Mice | Subcutaneous | - | [25] | |
| Blastomycosis | Adhesin BAD1 gene | Nd | Whole organism/Live-attenuated | Mice (T CD4+ depleted) | Subcutaneous | - | [26] |
| Cryptococcosis | C. neoformans strain H99γ | Nd | Live-attenuated | T-cell depleted mice | Nasal inhalation | - | [27] |
| Glucuronoxylomannan (GXM) | Tetanus toxoid (GXM-TT) | Conjugate/Solubleantigenic fractions | Mice | Subcutaneous | - | [28] | |
| C. neoformans Δsgl1 | Nd | Whole organism/Live-attenuated | Mice | Intranasal | - | [29] | |
| C. neoformans deletion of ZNF2 | Nd | Whole organism/Live-attenuated | Mice | Intranasal | - | [30] | |
| Candidiasis | Agglutinin-like sequence 3 (Als3p) | Aluminium hydroxide (Alum) | Recombinant protein (NDV-3) | Mice/Human | Oropharyngeal, Vaginal and Intravenous | Phase I | [31,32] |
| Recombinant secretory aspartyl proteinase (r-SAP-2) | Cholera toxin (CT) | Recombinant | Rat | Intravaginal | - | [33] | |
| PEV7 (r-Sap2 virosomes | Cholera toxin (CT)/Virosomal carrier | Recombinant protein | Mice/Human | Intravaginal | Phase I (delivered by intramuscula) | [34] | |
| Laminarin (Lam) β-glucan | Complete Freund’s adjuvant (CFA) | Lam- diphtheria toxoid CRM197 conjugate | Mice | Priming dose: Subcutaneous Booster: Intranasal | - | [35,36] | |
| Fructose bisphosphate aldolase (Fba) (cytosolic and cell wall peptides) | Alum or monophosphoryl lipid A (MPL) | Subunit | Mice | Subcutaneous | - | [36] | |
| The β-mannose trisaccharide, the Fba peptide T-cell epitope, a dectin-1 ligand, β1,3 glucan hexasaccharide | Freund’s incomplete adjuvant/with and without alum | Conjugate | Mice | Subcutaneous | [37] | ||
| C. albicans serotypes a and b ribosomes | Nonencapsulated Klebsiella pneumoniae proteoglycan | Recombinant/Conjugate capsule | Women with vulvovaginal candidiasis (VVC) | Oral | phase II | [38] | |
| Histoplasmosis | Heat Shock Protein 60 (HSP-60) | Monophosphoryl lipid A, synthetic trehalose dicorynomycolate, and cell wall skeleton | Recombinant protein | Mice | Subcutaneous | [39] | |
| HIS-62 | Complete Freund’s adjuvant (CFA) or incomplete Freund’s adjuvant (IFA) | Recombinant protein | Mice | Subcutaneous | - | [40] | |
| 80-kilodalton antigen | Complete Freund’s adjuvant (CFA) or incomplete Freund’s adjuvant (IFA) | Recombinant protein | Mice | Subcutaneous | - | [41] | |
| H Antigen | Monophosphoryl lipid A, synthetic trehalose dicorynomycolate, and cell wall skeleton | Recombinant protein | Mice | Subcutaneous | - | [42] | |
| Pneumocystosis | Kexin genes | Vector: CMV to express Antigen EF-1α to express CD40L | Kexin-CD40 L DNA vaccine | CD4-deficient mice | Intramuscular | - | [43] |
| Aspergillosis | Aspergillus fumigatus ΔsglA | Nd | Whole organism/Live-attenuated | Mice | Intranasal | - | [44] |
| Antigen Asp f 3 and Asp f 9 (VesiVax® Af3/9) | Lipidated Tucaresol, monophosphoryl lipid A or Pam3CAG | Recombinant protein and VesiVax liposomes | Mice | Subcutaneous and inguinal region | - | [45] | |
| Sporotrichosis | ZR8 peptide is from the GP70 protein | Freund’s incomplete adjuvant | Recombinant protein | Mice | Intramuscular | - | [46] |
2.2. Recombinant (Subunit) Vaccines
2.3. Conjugate Vaccines
2.4. Pan-Fungal Vaccine Strategy
2.5. DNA Vaccines
3. Immune Response against Fungal Infections and Approaches Vaccines
3.1. Vaccines Based on Antibody
3.2. Dendritic Cell Vaccination and Immunotherapy
3.3. Vaccines Based on T Helper Lymphocytes
4. HLA and Its Importance in Identification of Therapeutic Epitopes
| Target Pathogen | HLA | Bioinformatics | Experimental | Model | Reference(s) |
|---|---|---|---|---|---|
| Paracoccidioides spp. | A1 | - | + | Human | [135] |
| A2 | - | + | Human | ||
| B7 | - | + | Human | ||
| B21 | - | + | Human | ||
| CW1 | - | + | Human | ||
| B15 | - | + | Human | ||
| A9 | - | + | Human | [141,142,143,144] | |
| B13 | - | + | Human | ||
| B22 | - | + | Human | ||
| B40 | - | + | Human | ||
| B40 | - | + | Human | [141,144,145] | |
| DRB1-0101 | - | + | Human | [145] | |
| DRB1-0301 | - | + | Human | ||
| DRB1-0401 | - | + | Human | ||
| DRB1-0701 | - | + | Human | ||
| DRB1-1101 | - | + | Human | ||
| DRB1-1301 | - | + | Human | ||
| DRB1-0404 | - | + | Human | ||
| DRB1-0802 | - | + | Human | ||
| DRB1-0205 | - | + | Human | ||
| DRB1-1302 | - | + | Human | ||
| DRB1-1501 | - | + | Human | ||
| Histoplasma spp. | B7 | - | + | Human | |
| B7 | - | + | Human | [146] | |
| DR-15 | - | + | Human | ||
| DQ-6 | - | + | Human | ||
| Cryptococcus spp. | DR4 | - | + | Mouse | |
| C1203 | + | - | Human | [55,147] | |
| DRB1-0101 | + | - | Human | ||
| Coccidioides spp. | DRB1-0401 | - | + | Mouse | [148,149] |
4.1. Paracoccidioidomycosis
4.2. Histoplasmosis
4.3. Cryptococcosis
4.4. Coccidioidomycosis
5. Bioinformatic Tools for Vaccine Development against Fungi
| Pathogen | Subcellular Location and | B Cell Epitope Prediction | T Cell Epitope Prediction | Cytokines | Immunogenicity and Antigenic | Number of Final Targets | Year | Ref. |
|---|---|---|---|---|---|---|---|---|
| Histoplasma capsulatum | PSORT II; McGeoch method; TMHMM | -- | -- | -- | VaxiJen 2.0, | 5 targets | 2023 | [169] |
| Candida auris | TargetP; SignalP; Phobius; FunsecKB; PredGPI; TMHMM; EffectorP; FungalRV; FaaPred; | -- | NetMHCII 2.3 (IEDB) | -- | VaxiJen server | 39 targets | 2022 | [170] |
| Rhizopus delemar | SignalP; PredGPI; TMHMM; GPI- anchor | BCPREDS; Ellipro tool | IEDB (MHC class I and II); MHC class I processing | IL-4Pred; IL-10Pred; IFNepitope | VaxiJen 2.0 | 4 targets | 2022 | [171] |
| Sporothrix brasiliensis | -- | Bepipred 2.0 | PredBALC/C server; | IL-4pred; IFNepitope; 17eScan server; | SsEno | Enolase | 2022 | [172] |
| Cryptococcus neoformans var. grubii | -- | IEDB Bcell epitope prediction tool; BepiPred; ElliPro | IEDB MHC-I prediction tool; IEDB MHC-II prediction tool | -- | Kolaskar and Tongaonkar antigenicity method | heat shock 70 kDa protein | 2021 | [147] |
| Candida glabrata | -- | ElliPro; Bepipred tool from IEDB; | IEDB MHC I prediction tool/IEDB MHC II prediction | -- | Kolaskar and Tongaonkar antigenicity method | Fructose Bisphosphate Aldolase | 2021 | [173] |
| Candida dubliniensis | -- | -- | IEDB B-cell epitope prediction tool; NetMHCII 2.3; NETMHCpan 4.0 web servers | IL2Pred, IL4Pred, and IFNepitope | VaxiJen 2.0; AllergenFP | Secreted aspartyl proteinases (SAP) proteins | 2023 | [174] |
| Candida glabrata | SignalP-5; DeepLoc-1.0 | -- | -- | VaxiJen v2.0 server | 33 targets | 2022 | [175] | |
| Aspergillus fumigatus | -- | -- | NetMHCIIpan ver.3.2 server; | -- | AllergenFP; VaxiJen ver.2.0 | 5,8-linoleate diol synthase; ChainB-chitinase A1 | 2022 | [175] |
| Rhizopus microsporus | SignalP-5.0 server | -- | IEDB MHC I prediction tool/IEDB MHC II prediction; Docking by AutoDock Vina | INF predictionserver | -- | Spore coat (CotH) and Serine protease (SP) proteins as | 2021 | [176] |
| Candida albicans | CELLO2GO | -- | NetCTL server; IEDB MHC I prediction tool/IEDB MHC II prediction | -- | VaxiJen server, ANTIGENpro; AllerTOP; NetChop3.1; MHCII-NP | Als4p, Als3p, Fav2p, Als2p, Eap1p, Hyr1p, Hwp1p, Sap2p | 2020 | [77] |
| Candida auris | CELLO | ABCPred; Ellipro service | NetCTL 1.2; IEDB MHC II prediction | IFNepitope | VaxiJen server; Algpred server | Mitochondrial import receptor subunit, Putative beta-glucanase/Beta-glucan synthetases, 1,3-beta-glucanosyltransferase, Uricase, and a putative SUN family protein. | 2022 | [177] |
| Rhizopus delemar | TMHMM v2.0 server | IEDB Bcell epitope prediction tool (BepiPred and ElliPro) | NetCTL 1.2; IEDB MHC II prediction | IFNepitope; IL4pred; IL10pred | VaxiJen server; AllerTOP v2.0; MHCII-NP (IEDB); NetChop3.1 | Cell membrane by the copper oxidase-iron permease (FTR1) complex | 2022 | [140] |
| Candida tropicalis | CELLO2GO; PSORT II | -- | NETMHC 2.3; NETMHC 4.0; Bepipred (IEDB) | IFNepitope | VaxiJen 2.0; AllergenFP version 1. | Secreted aspartic protease 2 (SAP2) protein | 2022 | [166] |
5.1. T Cell Epitope Prediction
5.2. B Cell Epitope Prediction
5.3. Antigenicity Prediction
6. Concluding Remarks and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, D.W. Global and Multi-National Prevalence of Fungal Diseases—Estimate Precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef]
- Benedict, K.; Jackson, B.R.; Chiller, T.; Beer, K.D. Estimation of Direct Healthcare Costs of Fungal Diseases in the United States. Clin. Infect. Dis. 2019, 68, 1791–1797. [Google Scholar] [CrossRef] [PubMed]
- Seyedjavadi, S.S.; Bagheri, P.; Nasiri, M.J.; Razzaghi-Abyaneh, M.; Goudarzi, M. Fungal Infection in Co-Infected Patients With COVID-19: An Overview of Case Reports/Case Series and Systematic Review. Front. Microbiol. 2022, 13, 888452. [Google Scholar] [CrossRef]
- Skiada, A.; Pavleas, I.; Drogari-Apiranthitou, M. Epidemiology and Diagnosis of Mucormycosis: An Update. J. Fungi 2020, 6, 265. [Google Scholar] [CrossRef]
- Gebrehiwet, T.; Gebremichael, G. Development of Vaccination against Fungal Disease: A Review Article. Int. J. Trop. Dis. 2018, 1, 1–8. [Google Scholar] [CrossRef]
- do Nascimento Martins, E.M.; Reis, B.S.; de Resende, M.A.; de Andrade, A.S.R.; Goes, A.M. Mice Immunization with Radioattenuated Yeast Cells of Paracoccidiodes Brasiliensis: Influence of the Number of Immunizations. Mycopathologia 2009, 168, 51–58. [Google Scholar] [CrossRef]
- Liu, M.; Clemons, K.V.; Johansen, M.E.; Martinez, M.; Chen, V.; Stevens, D.A. Saccharomyces as a Vaccine against Systemic Candidiasis. Immunol. Investig. 2012, 41, 847–855. [Google Scholar] [CrossRef]
- Capilla, J.; Clemons, K.V.; Liu, M.; Levine, H.B.; Stevens, D.A. Saccharomyces Cerevisiae as a Vaccine against Coccidioidomycosis. Vaccine 2009, 27, 3662–3668. [Google Scholar] [CrossRef]
- Ardiani, A.; Higgins, J.P.; Hodge, J.W. Vaccines Based on Whole Recombinant Saccharomyces Cerevisiae Cells. FEMS Yeast Res. 2010, 10, 1060–1069. [Google Scholar] [CrossRef]
- Levine, H.B.; Cobb, J.M.; Smith, C.E. Immunity to Coccidioi-Domycosis Induced in Mice by Purified Spherule, Arthrospore, and Mycelial Vaccines. Trans. N. Y. Acad. Sci. 1960, 22, 436–449. [Google Scholar] [CrossRef]
- Levine, H.B.; Kong, Y.-C.M.; Smith, C.E. Immunization of Mice to Coccidioides Immitis: Dose, Regimen and Spherulation Stage of Killed Spherule Vaccines. J. Immunol. 1965, 94, 132–142. [Google Scholar] [CrossRef]
- Pappagianis, D.; Brown, B.W.; Cunningham, R.; Einstein, H.; Ellsworth, R.; Galgfani, J.; Hampson, C.R.; Holeman, C.W.; Johnson, R.H.; Larwood, T.R.; et al. Evaluation of the Protective Efficacy of the Killed Coccidioides Immitis Spherule Vaccine in Humans. Am. Rev. Respir. Dis. 1993, 148, 656–660. [Google Scholar] [CrossRef]
- Xue, J.; Chen, X.; Selby, D.; Hung, C.Y.; Yu, J.J.; Cole, G.T. A Genetically Engineered Live Attenuated Vaccine of Coccidioides Posadasii Protects BALB/c Mice against Coccidioidomycosis. Infect. Immun. 2009, 77, 3196–3208. [Google Scholar] [CrossRef] [PubMed]
- Narra, H.P.; Shubitz, L.F.; Mandel, M.A.; Trinh, H.T.; Griffin, K.; Buntzman, A.S.; Frelinger, J.A.; Galgiani, J.N.; Orbach, M.J. A Coccidioides Posadasii CPS1 Deletion Mutant Is Avirulent and Protects Mice from Lethal Infection. Infect. Immun. 2016, 84, 3007–3016. [Google Scholar] [CrossRef] [PubMed]
- Mandel, M.A.; Beyhan, S.; Voorhies, M.; Shubitz, L.F.; Galgiani, J.N.; Orbach, M.J.; Sil, A. The WOPR Family Protein Ryp1 Is a Key Regulator of Gene Expression, Development, and Virulence in the Thermally Dimorphic Fungal Pathogen Coccidioides Posadasii. PLoS Pathog. 2022, 18, e1009832. [Google Scholar] [CrossRef]
- Pinto, A.R.; Puccia, R.; Diniz, S.N.; Franco, M.F.; Travassos, L.R. DNA-Based Vaccination against Murine Paracoccidioidomycosis Using the Gp43 Gene from Paracoccidioides Brasiliensis. Vaccine 2000, 18, 3050–3058. [Google Scholar] [CrossRef]
- Ribeiro, A.M.; Bocca, A.L.; Amaral, A.C.; Souza, A.C.C.O.; Faccioli, L.H.; Coelho-Castelo, A.A.M.; Figueiredo, F.; Silva, C.L.; Felipe, M.S.S. HSP65 DNA as Therapeutic Strategy to Treat Experimental Paracoccidioidomycosis. Vaccine 2010, 28, 1528–1534. [Google Scholar] [CrossRef]
- Rittner, G.M.G.; Muñoz, J.E.; Marques, A.F.; Nosanchuk, J.D.; Taborda, C.P.; Travassos, L.R. Therapeutic DNA Vaccine Encoding Peptide P10 against Experimental Paracoccidioidomycosis. PLoS Negl. Trop. Dis. 2012, 6, e1519. [Google Scholar] [CrossRef]
- Assis-Marques, M.A.; Oliveira, A.F.; Ruas, L.P.; dos Reis, T.F.; Roque-Barreira, M.C.; Coelho, P.S.R. Saccharomyces Cerevisiae Expressing Gp43 Protects Mice against Paracoccidioides Brasiliensis Infection. PLoS ONE 2015, 10, e0120201. [Google Scholar] [CrossRef]
- Braga, C.J.M.; Rittner, G.M.G.; Henao, J.E.M.; Teixeira, A.F.; Massis, L.M.; Sbrogio-Almeida, M.E.; Taborda, C.P.; Travassos, L.R.; Ferreira, L.C.S. Paracoccidioides Brasiliensis Vaccine Formulations Based on the Gp43-Derived P10 Sequence and the Salmonella Enterica FliC Flagellin. Infect. Immun. 2009, 77, 1700–1707. [Google Scholar] [CrossRef]
- Fernandes, V.C.; Martins, E.M.N.; Boeloni, J.N.; Coitinho, J.B.; Serakides, R.; Goes, A.M. Additive Effect of RPb27 Immunization and Chemotherapy in Experimental Paracoccidioidomycosis. PLoS ONE 2011, 6, e17885. [Google Scholar] [CrossRef] [PubMed]
- De Bastos Ascenço Soares, R.; Gomez, F.J.; De Almeida Soares, C.M.; Deepe, G.S. Vaccination with Heat Shock Protein 60 Induces a Protective Immune Response against Experimental Paracoccidioides Brasiliensis Pulmonary Infection. Infect. Immun. 2008, 76, 4214–4221. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Clemons, K.V.; Bigos, M.; Medovarska, I.; Brummer, E.; Stevens, D.A. Immune Responses Induced by Heat Killed Saccharomyces Cerevisiae: A Vaccine against Fungal Infection. Vaccine 2011, 29, 1745–1753. [Google Scholar] [CrossRef]
- Jiang, C.; Magee, D.M.; Quitugua, T.N.; Cox, R.A. Genetic Vaccination against Coccidioides Immitis: Comparison of Vaccine Efficacy of Recombinant Antigen 2 and Antigen 2 CDNA. Infect. Immun. 1999, 67, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.-Y.; Zhang, H.; Castro-Lopez, N.; Ostroff, G.R.; Khoshlenar, P.; Abraham, A.; Cole, G.T.; Negron, A.; Forsthuber, T.; Peng, T.; et al. Glucan-Chitin Particles Enhance Th17 Response and Improve Protective Efficacy of a Multivalent Antigen (RCpa1) against Pulmonary Coccidioides Posadasii Infection. Infect. Immun. 2018, 86. [Google Scholar] [CrossRef]
- Wüthrich, M.; Filutowicz, H.I.; Warner, T.; Deepe, G.S.; Klein, B.S. Vaccine Immunity to Pathogenic Fungi Overcomes the Requirement for CD4 Help in Exogenous Antigen Presentation to CD8+ T Cells: Implications for Vaccine Development in Immune-Deficient Hosts. J. Exp. Med. 2003, 197, 1405–1416. [Google Scholar] [CrossRef]
- Wozniak, K.L.; Young, M.L.; Wormley, F.L. Protective Immunity against Experimental Pulmonary Cryptococcosis in T Cell-Depleted Mice. Clin. Vaccine Immunol. 2011, 18, 717–723. [Google Scholar] [CrossRef]
- Devi, S. Preclinical Efficacy of a Glucuronoxylomannan-Tetanus Toxoid Conjugate Vaccine of Cryptococcus Neoformans in a Murine Model. Vaccine 1996, 14, 841–844. [Google Scholar] [CrossRef]
- Normile, T.G.; Del Poeta, M. Three Models of Vaccination Strategies Against Cryptococcosis in Immunocompromised Hosts Using Heat-Killed Cryptococcus Neoformans Δsgl1. Front. Immunol. 2022, 13, 868523. [Google Scholar] [CrossRef]
- Lin, J.; Pham, T.; Hipsher, K.; Glueck, N.; Fan, Y.; Lin, X. Immunoprotection against Cryptococcosis Offered by Znf2 Depends on Capsule and the Hyphal Morphology. mBio 2022, 13, e0278521. [Google Scholar] [CrossRef]
- Schmidt, C.S.; White, C.J.; Ibrahim, A.S.; Filler, S.G.; Fu, Y.; Yeaman, M.R.; Edwards, J.E.; Hennessey, J.P. NDV-3, a Recombinant Alum-Adjuvanted Vaccine for Candida and Staphylococcus Aureus, Is Safe and Immunogenic in Healthy Adults. Vaccine 2012, 30, 7594–7600. [Google Scholar] [CrossRef]
- Spellberg, B.J.; Ibrahim, A.S.; Avanesian, V.; Fu, Y.; Myers, C.; Phan, Q.T.; Filler, S.G.; Yeaman, M.R.; Edwards, J.E. Efficacy of the Anti-Candida RAls3p-N or RAls1p-N Vaccines against Disseminated and Mucosal Candidiasis. J. Infect. Dis. 2006, 194, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Sandini, S.; La Valle, R.; Deaglio, S.; Malavasi, F.; Cassone, A.; De Bernardis, F. A Highly Immunogenic Recombinant and Truncated Protein of the Secreted Aspartic Proteases Family (RSap2t) of Candida Albicans as a Mucosal Anticandidal Vaccine. FEMS Immunol. Med. Microbiol. 2011, 62, 215–224. [Google Scholar] [CrossRef] [PubMed]
- De Bernardis, F.; Amacker, M.; Arancia, S.; Sandini, S.; Gremion, C.; Zurbriggen, R.; Moser, C.; Cassone, A. A Virosomal Vaccine against Candidal Vaginitis: Immunogenicity, Efficacy and Safety Profile in Animal Models. Vaccine 2012, 30, 4490–4498. [Google Scholar] [CrossRef] [PubMed]
- Bromuro, C.; Romano, M.; Chiani, P.; Berti, F.; Tontini, M.; Proietti, D.; Mori, E.; Torosantucci, A.; Costantino, P.; Rappuoli, R.; et al. Beta-Glucan-CRM197 Conjugates as Candidates Antifungal Vaccines. Vaccine 2010, 28, 2615–2623. [Google Scholar] [CrossRef]
- Xin, H.; Cartmell, J.; Bailey, J.J.; Dziadek, S.; Bundle, D.R.; Cutler, J.E. Self-Adjuvanting Glycopeptide Conjugate Vaccine against Disseminated Candidiasis. PLoS ONE 2012, 7, e35106. [Google Scholar] [CrossRef]
- Bundle, D.R.; Paszkiewicz, E.; Elsaidi, H.R.H.; Mandal, S.S.; Sarkar, S. A Three Component Synthetic Vaccine Containing a β-Mannan T-Cell Peptide Epitope and a β-Glucan Dendritic Cell Ligand. Molecules 2018, 23, 1961. [Google Scholar] [CrossRef]
- Levy, D.A.; Bohbot, J.M.; Catalan, F.; Normier, G.; Pinel, A.M.; Dussourd d’Hinterland, L. Phase II Study of D.651, an Oral Vaccine Designed to Prevent Recurrences of Vulvovaginal Candidiasis. Vaccine 1989, 7, 337–340. [Google Scholar] [CrossRef]
- Deepe, G.S.; Gibbons, R.S. Cellular and Molecular Regulation of Vaccination with Heat Shock Protein 60 from Histoplasma Capsulatum. Infect. Immun. 2002, 70, 3759–3767. [Google Scholar] [CrossRef]
- Gomez, F.J.; Gomez, A.N.A.M.; Deepe, G.S. Protective Efficacy of a 62-Kilodalton Antigen, HIS-62, from the Cell Wall and Cell Membrane of Histoplasma Capsulatum Yeast Cells. Infect. Immun. 1991, 59, 4459–4464. [Google Scholar] [CrossRef]
- Gomez, F.J.; Gomez, A.M.; Deepe, G.S. An 80-Kilodalton Antigen from Histoplasma Capsulatum That Has Homology to Heat Shock Protein 70 Induces Cell-Mediated Immune Responses and Protection in Mice. Infect. Immun. 1992, 60, 2565–2571. [Google Scholar] [CrossRef]
- Deepe, G.S.; Gibbons, R. Protective Efficacy of H Antigen from Histoplasma Capsulatum in a Murine Model of Pulmonary Histoplasmosis. Infect. Immun. 2001, 69, 3128–3134. [Google Scholar] [CrossRef]
- Zheng, M.; Ramsay, A.J.; Robichaux, M.B.; Norris, K.A.; Kliment, C.; Crowe, C.; Rapaka, R.R.; Steele, C.; McAllister, F.; Shellito, J.E.; et al. CD4+ T Cell–Independent DNA Vaccination against Opportunistic Infections. J. Clin. Investig. 2005, 115, 3536. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, C.M.; Normile, T.G.; Fabri, J.H.T.M.; Brauer, V.S.; Araújo, G.R.d.S.; Frases, S.; Nimrichter, L.; Malavazi, I.; Del Poeta, M. Vaccination with Live or Heat-Killed Aspergillus Fumigatus ΔsglA Conidia Fully Protects Immunocompromised Mice from Invasive Aspergillosis. mBio 2022, 13, e0232822. [Google Scholar] [CrossRef] [PubMed]
- Slarve, M.; Holznecht, N.; Reza, H.; Gilkes, A.; Slarve, I.; Olson, J.; Ernst, W.; Ho, S.O.; Adler-Moore, J.; Fujii, G. Recombinant Aspergillus Fumigatus Antigens Asp f 3 and Asp f 9 in Liposomal Vaccine Protect Mice against Invasive Pulmonary Aspergillosis. Vaccine 2022, 40, 4160–4168. [Google Scholar] [CrossRef] [PubMed]
- De Almeida, J.R.F.; Jannuzzi, G.P.; Kaihami, G.H.; Breda, L.C.D.; Ferreira, K.S.; De Almeida, S.R. An Immunoproteomic Approach Revealing Peptides from Sporothrix Brasiliensis That Induce a Cellular Immune Response in Subcutaneous Sporotrichosis. Sci. Rep. 2018, 8, 4912. [Google Scholar] [CrossRef]
- Pirofski, L.A.; Casadevall, A. Use of Licensed Vaccines for Active Immunization of the Immunocompromised Host. Clin. Microbiol. Rev. 1998, 11, 1–26. [Google Scholar] [CrossRef]
- Santos, E.; Levitz, S.M. Fungal Vaccines and Immunotherapeutics. Cold Spring Harb. Perspect. Med. 2014, 4, 1–14. [Google Scholar] [CrossRef]
- Wang, B.; Norbury, C.C.; Greenwood, R.; Bennink, J.R.; Yewdell, J.W.; Frelinger, J.A. Multiple Paths for Activation of Naive CD8+ T Cells: CD4-Independent Help. J. Immunol. 2001, 167, 1283–1289. [Google Scholar] [CrossRef]
- Scheckelhoff, M.; Deepe, G.S. The Protective Immune Response to Heat Shock Protein 60 of Histoplasma Capsulatum Is Mediated by a Subset of Vβ8.1/8.2 + T Cells. J. Immunol. 2002, 169, 5818–5826. [Google Scholar] [CrossRef]
- Stuehler, C.; Khanna, N.; Bozza, S.; Zelante, T.; Moretti, S.; Kruhm, M.; Lurati, S.; Conrad, B.; Worschech, E.; Stevanović, S.; et al. Cross-Protective TH1 Immunity against Aspergillus Fumigatus and Candida Albicans. Blood 2011, 117, 5881–5891. [Google Scholar] [CrossRef] [PubMed]
- Ito, J.I.; Lyons, J.M.; Hong, T.B.; Tamae, D.; Liu, Y.K.; Wilczynski, S.P.; Kalkum, M. Vaccinations with Recombinant Variants of Aspergillus Fumigatus Allergen Asp f 3 Protect Mice against Invasive Aspergillosis. Infect. Immun. 2006, 74, 5075–5084. [Google Scholar] [CrossRef] [PubMed]
- Bozza, S.; Clavaud, C.; Giovannini, G.; Fontaine, T.; Beauvais, A.; Sarfati, J.; D’Angelo, C.; Perruccio, K.; Bonifazi, P.; Zagarella, S.; et al. Immune Sensing of Aspergillus Fumigatus Proteins, Glycolipids, and Polysaccharides and the Impact on Th Immunity and Vaccination. J. Immunol. 2009, 183, 2407–2414. [Google Scholar] [CrossRef] [PubMed]
- Specht, C.A.; Nong, S.; Dan, J.M.; Lee, C.K.; Levitz, S.M. Contribution of Glycosylation to T Cell Responses Stimulated by Recombinant Cryptococcus Neoformans Mannoprotein. J. Infect. Dis. 2007, 196, 796–800. [Google Scholar] [CrossRef] [PubMed]
- Specht, C.A.; Lee, C.K.; Huang, H.; Hester, M.M.; Liu, J.; Luckie, B.A.; Torres Santana, M.A.; Mirza, Z.; Khoshkenar, P.; Abraham, A.; et al. Vaccination with Recombinant Cryptococcus Proteins in Glucan Particles Protects Mice against Cryptococcosis in a Manner Dependent upon Mouse Strain and Cryptococcal Species. mBio 2017, 8, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Abuodeh, R.O.; Shubitz, L.F.; Siegel, E.; Snyder, S.; Peng, T.; Orsborn, K.I.; Brummer, E.; Stevens, D.A.; Galgiani, J.N. Resistance to Coccidioides Immitis in Mice after Immunization with Recombinant Protein or a DNA Vaccine of a Proline-Rich Antigen. Infect. Immun. 1999, 67, 2935–2940. [Google Scholar] [CrossRef]
- Hurtgen, B.J.; Hung, C.Y.; Ostroff, G.R.; Levitz, S.M.; Cole, G.T. Construction and Evaluation of a Novel Recombinant T Cell Epitope-Based Vaccine against Coccidioidomycosis. Infect. Immun. 2012, 80, 3960–3974. [Google Scholar] [CrossRef]
- Orsborn, K.I.; Shubitz, L.F.; Peng, T.; Kellner, E.M.; Orbach, M.J.; Haynes, P.A.; Galgiani, J.N. Protein Expression Profiling of Coccidioides Posadasii by Two-Dimensional Differential in-Gel Electrophoresis and Evaluation of a Newly Recognized Peroxisomal Matrix Protein as a Recombinant Vaccine Candidate. Infect. Immun. 2006, 74, 1865–1872. [Google Scholar] [CrossRef]
- Shubitz, L.F.; Yu, J.J.; Hung, C.Y.; Kirkland, T.N.; Peng, T.; Perrill, R.; Simons, J.; Xue, J.; Herr, R.A.; Cole, G.T.; et al. Improved Protection of Mice against Lethal Respiratory Infection with Coccidioides Posadasii Using Two Recombinant Antigens Expressed as a Single Protein. Vaccine 2006, 24, 5904–5911. [Google Scholar] [CrossRef]
- Tarcha, E.J.; Basrur, V.; Hung, C.Y.; Gardner, M.J.; Cole, G.T. A Recombinant Aspartyl Protease of Coccidioides Posadasii Induces Protection against Pulmonary Coccidioidomycosis in Mice. Infect. Immun. 2006, 74, 516–527. [Google Scholar] [CrossRef]
- Ibrahim, A.S.; Luo, G.; Gebremariam, T.; Lee, H.; Schmidt, C.S.; Hennessey, J.P.; French, S.W.; Yeaman, M.R.; Filler, S.G.; Edwards, J.E. NDV-3 Protects Mice from Vulvovaginal Candidiasis through T- and B-Cell Immune Response. Vaccine 2013, 31, 5549–5556. [Google Scholar] [CrossRef] [PubMed]
- Baquir, B.; Lin, L.; Ibrahim, A.S.; Fu, Y.; Avanesian, V.; Tu, A.; Edwards, J., Jr.; Spellberg, B. Immunological Reactivity of Blood from Healthy Humans to the RAls3p-N Vaccine Protein. J. Infect. Dis. 2010, 201, 473–477. [Google Scholar] [CrossRef]
- Li, W.Q.; Hu, X.C.; Zhang, X.; Ge, Y.; Zhao, S.; Hu, Y.; Ashman, R.B. Immunisation with the Glycolytic Enzyme Enolase Confers Effective Protection against Candida Albicans Infection in Mice. Vaccine 2011, 29, 5526–5533. [Google Scholar] [CrossRef]
- Nami, S.; Mohammadi, R.; Vakili, M.; Khezripour, K.; Mirzaei, H.; Morovati, H. Fungal Vaccines, Mechanism of Actions and Immunology: A Comprehensive Review. Biomed. Pharmacother. 2019, 109, 333–344. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, R.; Ramachandran, S. Immunoinformatics as a Tool for New Antifungal Vaccines. Methods Mol. Biol. 2017, 1625, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Ibrahim, A.S.; Xu, X.; Farber, J.M.; Avanesian, V.; Baquir, B.; Fu, Y.; French, S.W.; Edwards, J.E.; Spellberg, B. Th1-Th17 Cells Mediate Protective Adaptive Immunity against Staphylococcus Aureus and Candida Albicans Infection in Mice. PLoS Pathog. 2009, 5. [Google Scholar] [CrossRef]
- Spellberg, B.; Ibrahim, A.S.; Yeaman, M.R.; Lin, L.; Fu, Y.; Avanesian, V.; Bayer, A.S.; Filler, S.G.; Lipke, P.; Otoo, H.; et al. The Antifungal Vaccine Derived from the Recombinant N Terminus of Als3p Protects Mice against the Bacterium Staphylococcus Aureus. Infect. Immun. 2008, 76, 4574–4580. [Google Scholar] [CrossRef]
- Edwards, J.E.; Schwartz, M.M.; Schmidt, C.S.; Sobel, J.D.; Nyirjesy, P.; Schodel, F.; Marchus, E.; Lizakowski, M.; Demontigny, E.A.; Hoeg, J.; et al. A Fungal Immunotherapeutic Vaccine (NDV-3A) for Treatment of Recurrent Vulvovaginal Candidiasis-A Phase 2 Randomized, Double-Blind, Placebo-Controlled Trial. Clin. Infect. Dis. 2018, 66, 1928–1936. [Google Scholar] [CrossRef]
- Alqarihi, A.; Singh, S.; Edwards, J.E.; Ibrahim, A.S.; Uppuluri, P. NDV-3A Vaccination Prevents C. Albicans Colonization of Jugular Vein Catheters in Mice. Sci. Rep. 2019, 9, 6194. [Google Scholar] [CrossRef]
- NCT. Safety and Immunogenicity Study of a Virosomal Vaccine Against Recurrent Vulvovaginal Candida Infection. 2010. Available online: https://clinicaltrials.gov/show/NCT01067131 (accessed on 18 May 2023).
- Luo, G.; Ibrahim, A.S.; Spellberg, B.; Nobile, C.J.; Mitchell, A.P.; Fu, Y. Candida Albicans Hyr1p Confers Resistance to Neutrophil Killing and Is a Potential Vaccine Target. J. Infect. Dis. 2010, 201, 1718–1728. [Google Scholar] [CrossRef]
- Nitz, M.; Ling, C.C.; Otter, A.; Cutler, J.E.; Bundle, D.R. The Unique Solution Structure and Immunochemistry of the Candida Albicans β-1,2-Mannopyranan Cell Wall Antigens. J. Biol. Chem. 2002, 277, 3440–3446. [Google Scholar] [CrossRef] [PubMed]
- De Bernardis, F.; Graziani, S.; Tirelli, F.; Antonopoulou, S. Candida Vaginitis: Virulence, Host Response and Vaccine Prospects. Med. Mycol. 2018, 56, S26–S31. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, L. Vaccination with Phage-Displayed Antigenic Epitope. Methods Mol. Biol. 2017, 1625, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.L.; Eberle, K.; Colón, J.R.; Courville, E.; Xin, H. Synthetic Conjugate Peptide Fba-Met6 (MP12) Induces Complement-Mediated Resistance against Disseminated Candida Albicans. Vaccine 2021, 39, 4099–4107. [Google Scholar] [CrossRef]
- Rappuoli, R.; Bottomley, M.J.; D’Oro, U.; Finco, O.; De Gregorio, E. Reverse Vaccinology 2.0: Human Immunology Instructs Vaccine Antigen Design. J. Exp. Med. 2016, 213, 469–481. [Google Scholar] [CrossRef]
- Tarang, S.; Kesherwani, V.; LaTendresse, B.; Lindgren, L.; Rocha-Sanchez, S.M.; Weston, M.D. In Silico Design of a Multivalent Vaccine Against Candida Albicans. Sci. Rep. 2020, 10, 1066. [Google Scholar] [CrossRef]
- Pizza, M.; Scarlato, V.; Masignani, V.; Giuliani, M.M.; Arico, B.; Comanducci, M.; Jennings, G.T.; Baldi, L.; Bartolini, E.; Capecchi, B.; et al. Identification of Vaccine Candidates against Serogroup B Meningococcus by Whole-Genome Sequencing Identification of Vaccine Candidates Against Serogroup B Meningococcus by Whole-Genome Sequencing. Science (1979) 2000, 287, 1816–1820. [Google Scholar]
- Karch, C.P.; Burkhard, P. Vaccine Technologies: From Whole Organisms to Rationally Designed Protein Assemblies. Biochem. Pharmacol. 2016, 120, 1–14. [Google Scholar] [CrossRef]
- Pietrella, D.; Rachini, A.; Torosantucci, A.; Chiani, P.; Brown, A.J.P.; Bistoni, F.; Costantino, P.; Mosci, P.; D’Enfert, C.; Rappuoli, R.; et al. A β-Glucan-Conjugate Vaccine and Anti-β-Glucan Antibodies Are Effective against Murine Vaginal Candidiasis as Assessed by a Novel in Vivo Imaging Technique. Vaccine 2010, 28, 1717–1725. [Google Scholar] [CrossRef]
- Guazzelli, L.; Crawford, C.J.; Ulc, R.; Bowen, A.; McCabe, O.; Jedlicka, A.J.; Wear, M.P.; Casadevall, A.; Oscarson, S. A Synthetic Glycan Array Containing Cryptococcus Neoformans Glucuronoxylomannan Capsular Polysaccharide Fragments Allows the Mapping of Protective Epitopes. Chem. Sci. 2020, 11, 9209–9217. [Google Scholar] [CrossRef]
- Han, Y.; Ulrich, M.A.; Cutler, J.E. Candida Albicans Mannan Extract–Protein Conjugates Induce a Protective Immune Response against Experimental Candidiasis. J. Infect. Dis. 1999, 179, 1477–1484. [Google Scholar] [CrossRef] [PubMed]
- Xin, H.; Glee, P.; Adams, A.; Mohiuddin, F.; Eberle, K. Design of a Mimotope-Peptide Based Double Epitope Vaccine against Disseminated Candidiasis. Vaccine 2019, 37, 2430–2438. [Google Scholar] [CrossRef] [PubMed]
- Clemons, K.V.; Danielson, M.E.; Michel, K.S.; Liu, M.; Ottoson, N.C.; Leonardo, S.M.; Martinez, M.; Chen, V.; Antonysamy, M.A.; Stevens, D.A. Whole Glucan Particles as a Vaccine against Murine Aspergillosis. J. Med. Microbiol. 2014, 63, 1750–1759. [Google Scholar] [CrossRef] [PubMed]
- Paulovičová, E.; Machová, E.; Tulinská, J.; Bystrický, S. Cell and Antibody Mediated Immunity Induced by Vaccination with Novel Candida Dubliniensis Mannan Immunogenic Conjugate. Int. Immunopharmacol. 2007, 7, 1325–1333. [Google Scholar] [CrossRef] [PubMed]
- Xin, H.; Dziadek, S.; Bundle, D.R.; Cutler, J.E. Synthetic Glycopeptide Vaccines Combining β-Mannan and Peptide Epitopes Induce Protection against Candidiasis. Proc. Natl. Acad. Sci. USA 2008, 105, 13526–13531. [Google Scholar] [CrossRef]
- Rivera, A.; Hohl, T.M. Calnexin Bridges the Gap toward a Pan-Fungal Vaccine. Cell Host Microbe 2015, 17, 421–423. [Google Scholar] [CrossRef]
- Torosantucci, A.; Bromuro, C.; Chiani, P.; De Bernardis, F.; Berti, F.; Galli, C.; Norelli, F.; Bellucci, C.; Polonelli, L.; Costantino, P.; et al. A Novel Glyco-Conjugate Vaccine against Fungal Pathogens. J. Exp. Med. 2005, 202, 597–606. [Google Scholar] [CrossRef]
- Wüthrich, M.; Gern, B.; Hung, C.Y.; Ersland, K.; Rocco, N.; Pick-Jacobs, J.; Galles, K.; Filutowicz, H.; Warner, T.; Evans, M.; et al. Vaccine-Induced Protection against 3 Systemic Mycoses Endemic to North America Requires Th17 Cells in Mice. J. Clin. Investig. 2011, 121, 554–568. [Google Scholar] [CrossRef]
- Wüthrich, M.; Brandhorst, T.T.; Sullivan, T.D.; Filutowicz, H.; Sterkel, A.; Stewart, D.; Li, M.; Lerksuthirat, T.; Lebert, V.; Shen, Z.T.; et al. Calnexin Induces Expansion of Antigen-Specific CD4+ T Cells That Confer Immunity to Fungal Ascomycetes via Conserved Epitopes. Cell Host Microbe 2015, 17, 452–465. [Google Scholar] [CrossRef]
- Rayens, E.; Rabacal, W.; Willems, H.M.E.; Kirton, G.M.; Barber, J.P.; Mousa, J.J.; Celia-Sanchez, B.N.; Momany, M.; Norris, K.A. Immunogenicity and Protective Efficacy of a Pan-Fungal Vaccine in Preclinical Models of Aspergillosis, Candidiasis, and Pneumocystosis. PNAS Nexus 2022, 1, pgac248. [Google Scholar] [CrossRef]
- Lee, J.; Arun Kumar, S.; Jhan, Y.Y.; Bishop, C.J. Engineering DNA Vaccines against Infectious Diseases. Acta Biomater. 2018, 80, 31–47. [Google Scholar] [CrossRef] [PubMed]
- de Amorim, J.; Magalhães, A.; Muñoz, J.E.; Rittner, G.M.G.; Nosanchuk, J.D.; Travassos, L.R.; Taborda, C.P. DNA Vaccine Encoding Peptide P10 against Experimental Paracoccidioidomycosis Induces Long-Term Protection in Presence of Regulatory T Cells. Microbes Infect. 2013, 15, 181–191. [Google Scholar] [CrossRef]
- Ivey, F.D.; Magee, D.M.; Woitaske, M.D.; Johnston, S.A.; Cox, R.A. Identification of a Protective Antigen of Coccidioides Immitis by Expression Library Immunization. Vaccine 2003, 21, 4359–4367. [Google Scholar] [CrossRef] [PubMed]
- Shafaati, M.; Saidijam, M.; Soleimani, M.; Hazrati, F.; Mirzaei, R.; Amirheidari, B.; Tanzadehpanah, H.; Karampoor, S.; Kazemi, S.; Yavari, B.; et al. A Brief Review on DNA Vaccines in the Era of COVID-19. Future Virol. 2022, 17, 49–66. [Google Scholar] [CrossRef] [PubMed]
- Faiolla, R.C.L.; Coelho, M.C.; de Santana, R.C.; Martinez, R. Histoplasmosis in Immunocompetent Individuals Living in an Endemic Area in the Brazilian Southeast. Rev. Soc. Bras. Med. Trop. 2013, 46, 461–465. [Google Scholar] [CrossRef]
- Fox, J. Gene Therapy Safety Issues Come to Fore. Nat. Biotechnol. 1999, 17, 1153. [Google Scholar] [CrossRef]
- Gow, N.A.R.; Netea, M.G. Medical Mycology and Fungal Immunology: New Research Perspectives Addressing a Major World Health Challenge. Philos. Trans. R. Soc. B Biol. Sci. 2016, 371, 20150462. [Google Scholar] [CrossRef]
- Mendes, R.P.; de Cavalcante, R.S.; Marques, S.A.; Marques, M.E.A.; Venturini, J.; Sylvestre, T.F.; Paniago, A.M.M.; Pereira, A.C.; da de Silva, J.F.; Fabro, A.T.; et al. Paracoccidioidomycosis: Current Perspectives from Brazil. Open Microbiol. J. 2017, 11, 224–282. [Google Scholar] [CrossRef]
- Bongomin, F. Post-Tuberculosis Chronic Pulmonary Aspergillosis: An Emerging Public Health Concern. PLoS Pathog. 2020, 16, e1008742. [Google Scholar] [CrossRef]
- Romani, L. Immunity to Fungal Infections. Nat. Rev. Immunol. 2004, 4, 11–24. [Google Scholar] [CrossRef]
- Kurosawa, M.; Yonezumi, M.; Hashino, S.; Tanaka, J.; Nishio, M.; Kaneda, M.; Ota, S.; Koda, K.; Suzuki, N.; Yoshida, M.; et al. Epidemiology and Treatment Outcome of Invasive Fungal Infections in Patients with Hematological Malignancies. Int. J. Hematol. 2012, 96, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Bacher, P.; Hohnstein, T.; Beerbaum, E.; Röcker, M.; Blango, M.G.; Kaufmann, S.; Röhmel, J.; Eschenhagen, P.; Grehn, C.; Seidel, K.; et al. Human Anti-Fungal Th17 Immunity and Pathology Rely on Cross-Reactivity against Candida Albicans. Cell 2019, 176, 1340–1355.e15. [Google Scholar] [CrossRef] [PubMed]
- Benard, G. An Overview of the Immunopathology of Human Paracoccidioidomycosis. Mycopathologia 2008, 165, 209–221. [Google Scholar] [CrossRef] [PubMed]
- Wormley, F.L.; Perfect, J.R.; Steele, C.; Cox, G.M. Protection against Cryptococcosis by Using a Murine Gamma Interferon-Producing Cryptococcus Neoformans Strain. Infect. Immun. 2007, 75, 1453–1462. [Google Scholar] [CrossRef] [PubMed]
- Mochon, A.B.; Cutler, J.E. Is a Vaccine Needed against Candida Albicans? Med. Mycol. 2005, 43, 97–115. [Google Scholar] [CrossRef]
- Oliveira, L.V.N.; Wang, R.; Specht, C.A.; Levitz, S.M. Vaccines for Human Fungal Diseases: Close but Still a Long Way to Go. NPJ Vaccines 2021, 6, 1–8. [Google Scholar] [CrossRef]
- Rabaan, A.A.; Alfaraj, A.H.; Alshengeti, A.; Alawfi, A.; Alwarthan, S.; Alhajri, M.; Al-Najjar, A.H.; Al Fares, M.A.; Najim, M.A.; Almuthree, S.A.; et al. Antibodies to Combat Fungal Infections: Development Strategies and Progress. Microorganisms 2023, 11, 671. [Google Scholar] [CrossRef]
- Karwa, R.; Wargo, K.A. Efungumab: A Novel Agent in the Treatment of Invasive Candidiasis. Ann. Pharmacother. 2009, 43, 1818–1823. [Google Scholar] [CrossRef]
- Pachl, J.; Svoboda, P.; Jacobs, F.; Vandewoude, K.; van der Hoven, B.; Spronk, P.; Masterson, G.; Malbrain, M.; Aoun, M.; Garbino, J.; et al. A Randomized, Blinded, Multicenter Trial of Lipid-Associated Amphotericin B Alone versus in Combination with an Antibody-Based Inhibitor of Heat Shock Protein 90 in Patients with Invasive Candidiasis. Clin. Infect. Dis. 2006, 42, 1404–1413. [Google Scholar] [CrossRef]
- Loreto, É.S.; Tondolo, J.S.M.; Alves, S.H.; Santurio, J.M. Immunotherapy for Fungal Infections. In Immunotherapy—Myths, Reality, Ideas, Future; InTech: Houston, TX, USA, 2017. [Google Scholar]
- Omaetxebarria, M.; Moragues, M.; Elguezabal, N.; Rodriguez-Alejandre, A.; Brena, S.; Schneider, J.; Polonelli, L.; Ponton, J. Antifungal and Antitumor Activities of a Monoclonal Antibody Directed Against a Stress Mannoprotein of Candida Albicans. Curr. Mol. Med. 2005, 5, 393–401. [Google Scholar] [CrossRef]
- Brena, S.; Omaetxebarría, M.J.; Elguezabal, N.; Cabezas, J.; Moragues, M.D.; Pontón, J. Fungicidal Monoclonal Antibody C7 Binds to Candida Albicans Als3. Infect. Immun. 2007, 75, 3680–3682. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.J.; Schneider, J.; Moragues, M.D.; Martínez-Conde, R.; Pontón, J.; Aguirre, J.M. Cross-Reactivity between Candida Albicans and Oral Squamous Cell Carcinoma Revealed by Monoclonal Antibody C7. Anticancer Res. 2007, 27, 3639–3643. [Google Scholar] [PubMed]
- Singh, S.; Uppuluri, P.; Mamouei, Z.; Alqarihi, A.; Elhassan, H.; French, S.; Lockhart, S.R.; Chiller, T.; Edwards, J.E.; Ibrahim, A.S. The NDV-3A Vaccine Protects Mice from Multidrug Resistant Candida Auris Infection. PLoS Pathog. 2019, 15. [Google Scholar] [CrossRef] [PubMed]
- Matveev, A.L.; Krylov, V.B.; Khlusevich, Y.A.; Baykov, I.K.; Yashunsky, D.V.; Emelyanova, L.A.; Tsvetkov, Y.E.; Karelin, A.A.; Bardashova, A.V.; Wong, S.S.W.; et al. Novel Mouse Monoclonal Antibodies Specifically Recognizing β-(1!3)-D-Glucan Antigen. PLoS ONE 2019, 14. [Google Scholar] [CrossRef]
- Boniche, C.; Rossi, S.A.; Kischkel, B.; Barbalho, F.V.; Moura, Á.N.D.; Nosanchuk, J.D.; Travassos, L.R.; Taborda, C.P. Immunotherapy against Systemic Fungal Infections Based on Monoclonal Antibodies. J. Fungi 2020, 6, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.D.; Denning, D.W.; Gow, N.A.R.R.; Levitz, S.M.; Netea, M.G.; White, T.C. Hidden Killers: Human Fungal Infections. Sci. Transl. Med. 2012, 4, 1–10. [Google Scholar] [CrossRef]
- Ramirez-Ortiz, Z.G.; Means, T.K. The Role of Dendritic Cells in the Innate Recognition of Pathogenic Fungi (A. fumigatus, C. neoformans and C. albicans). Virulence 2012, 3, 635–646. [Google Scholar] [CrossRef]
- Sabado, R.L.; Balan, S.; Bhardwaj, N. Dendritic Cell-Based Immunotherapy. Cell Res. 2017, 27, 74–95. [Google Scholar] [CrossRef]
- Bozza, S.; Perruccio, K.; Montagnoli, C.; Gaziano, R.; Bellocchio, S.; Burchielli, E.; Nkwanyuo, G.; Pitzurra, L.; Velardi, A.; Romani, L. A Dendritic Cell Vaccine against Invasive Aspergillosis in Allogeneic Hematopoietic Transplantation. Blood 2003, 102, 3807–3814. [Google Scholar] [CrossRef]
- Bozza, S.; Gaziano, R.; Lipford, G.B.; Montagnoli, C.; Bacci, A.; Di Francesco, P.; Kurup, V.P.; Wagner, H.; Romani, L. Vaccination of Mice against Invasive Aspergillosis with Recombinant Aspergillus Proteins and CpG Oligodeoxynucleotides as Adjuvants. Microbes Infect. 2002, 4, 1281–1290. [Google Scholar] [CrossRef]
- Shao, C.; Qu, J.; He, L.; Zhang, Y.; Wang, J.; Zhou, H.; Wang, Y.; Liu, X. Dendritic Cells Transduced with an Adenovirus Vector Encoding Interleukin-12 Are a Potent Vaccine for Invasive Pulmonary Aspergillosis. Genes Immun. 2005, 6, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Ueno, K.; Kinjo, Y.; Okubo, Y.; Aki, K.; Urai, M.; Kaneko, Y.; Shimizu, K.; Wang, D.N.; Okawara, A.; Nara, T.; et al. Dendritic Cell-Based Immunization Ameliorates Pulmonary Infection with Highly Virulent Cryptococcus Gattii. Infect. Immun. 2015, 83, 1577–1586. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, A.; Ferreira, K.S.; Almeida, S.R.; Nosanchuk, J.D.; Travassos, L.R.; Taborda, C.P. Prophylactic and Therapeutic Vaccination Using Dendritic Cells Primed with Peptide 10 Derived from the 43-Kilodalton Glycoprotein of Paracoccidioides Brasiliensis. Clin. Vaccine Immunol. 2012, 19, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Borghi, M.; Renga, G.; Puccetti, M.; Oikonomou, V.; Palmieri, M.; Galosi, C.; Bartoli, A.; Romani, L. Antifungal Th Immunity: Growing up in Family. Front. Immunol. 2014, 5, 506. [Google Scholar] [CrossRef]
- Speakman, E.A.; Dambuza, I.M.; Salazar, F.; Brown, G.D. T Cell Antifungal Immunity and the Role of C-Type Lectin Receptors. Trends Immunol. 2020, 41, 61–76. [Google Scholar] [CrossRef] [PubMed]
- Kumaresan, P.R.; da Silva, T.A.; Kontoyiannis, D.P. Methods of Controlling Invasive Fungal Infections Using CD8+ T Cells. Front. Immunol. 2018, 8, 1939. [Google Scholar] [CrossRef]
- Gilbert, S.C. T-Cell-Inducing Vaccines—What’s the Future. Immunology 2012, 135, 19–26. [Google Scholar] [CrossRef]
- Li, D.; Li, X.; Zhou, W.L.; Huang, Y.; Liang, X.; Jiang, L.; Yang, X.; Sun, J.; Li, Z.; Han, W.D.; et al. Genetically Engineered t Cells for Cancer Immunotherapy. Signal Transduct. Target. Ther. 2019, 4, 1–17. [Google Scholar] [CrossRef]
- Lum, L.G.; Bollard, C.M. Specific Adoptive T-Cell Therapy for Viral and Fungal Infections. In Management of Infections in the Immunocompromised Host; Springer International Publishing: Berlin/Heidelberg, Germany, 2018; pp. 395–411. ISBN 9783319776743. [Google Scholar]
- Cenci, E.; Mencacci, A.; Bacci, A.; Bistoni, F.; Kurup, V.P.; Romani, L. T Cell Vaccination in Mice with Invasive Pulmonary Aspergillosis. J. Immunol. 2000, 165, 381–388. [Google Scholar] [CrossRef]
- Sun, Z.; Zhu, P.; Li, L.; Wan, Z.; Zhao, Z.; Li, R. Adoptive Immunity Mediated by HLA-A*0201 Restricted Asp F16 Peptides-Specific CD8+ T Cells against Aspergillus Fumigatus Infection. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 3089–3096. [Google Scholar] [CrossRef]
- Posch, W.; Steger, M.; Wilflingseder, D.; Lass-Flörl, C. Promising Immunotherapy against Fungal Diseases. Expert Opin. Biol. Ther. 2017, 17, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Dias, M.F.; Pereira, A.C.; Pereira, A.; Alves, M.S. The Role of HLA Antigens in the Development of Paracoccidioidomycosis. J. Eur. Acad. Dermatol. Venereol. 2000, 14, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Trincado, J.L.; Gomez-Perosanz, M.; Reche, P.A. Fundamentals and Methods for T- and B-Cell Epitope Prediction. J. Immunol. Res. 2017, 2017, 2680160. [Google Scholar] [CrossRef] [PubMed]
- Osama, A.; Sati, M.; Abdelmoneim, A.H. Multi-Epitope Peptide Vaccine Prediction for Candida Albicans Targeting Pyruvate Kinase Protein; an Immunoinformatics Approach Vaccines Designing View Project Monosoduim Glutamate Toxicity View Project SEE PROFILE. bioRxiv 2019. [Google Scholar] [CrossRef]
- Raoufi, E.; Hemmati, M.; Eftekhari, S.; Khaksaran, K.; Mahmodi, Z.; Farajollahi, M.M.; Mohsenzadegan, M. Epitope Prediction by Novel Immunoinformatics Approach: A State-of-the-Art Review. Int. J. Pept. Res. Ther. 2020, 26, 1155–1163. [Google Scholar] [CrossRef]
- Repac, J.; Mandić, M.; Lunić, T.; Božić, B.; Božić Nedeljković, B. Mining the Capacity of Human-Associated Microorganisms to Trigger Rheumatoid Arthritis—A Systematic Immunoinformatics Analysis of T Cell Epitopes. PLoS ONE 2021, 16, e0253918. [Google Scholar] [CrossRef]
- Araf, Y.; Moin, A.T.; Timofeev, V.I.; Faruqui, N.A.; Saiara, S.A.; Ahmed, N.; Parvez, M.S.A.; Rahaman, T.I.; Sarkar, B.; Ullah, M.A.; et al. Immunoinformatic Design of a Multivalent Peptide Vaccine Against Mucormycosis: Targeting FTR1 Protein of Major Causative Fungi. Front. Immunol. 2022, 13, 863234. [Google Scholar] [CrossRef]
- Goldani, L.Z.; Monteiro, C.M.C.; Donadi, E.A.; Martinez, R.; Voltarelli, J.C. HLA Antigens in Brazilian Patients with Paracoccidioidomycosis. Mycopathologia 1991, 114, 89–91. [Google Scholar] [CrossRef]
- de Restrepo, F.M.; Restrepo, M.; Restrepo, A. Blood Groups and HLA Antigens in Paracoccidioidomycosis. Med. Mycol. 1983, 21, 35–39. [Google Scholar] [CrossRef]
- González, N.; Albornoz, M.; Ríos, R.; Prado, L. HLA y Paracoccidioidomycosis. Cien. Tecnol. Venez. 1985, 2, 229–234. [Google Scholar]
- Lacerda, G.B.; Arce-Gomez, B.; Filho, F.Q.T.; Mycology, V.; Mkdica, M.; Clinicas, H. De Increased Frequency of HLA-B40 in Patients with Paracoccidioidomycosis. Med. Mycol. 1988, 26, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Mamoni, R.L.; Blotta, M.H.S.L. Flow-Cytometric Analysis of Cytokine Production in Human Paracoccidioidomycosis. Cytokine 2006, 35, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Braley, R.E.; Meredith, T.A.; Aaberg, T.M.; Koethe, S.M.; Witkowski, J.A. The Prevalence of HLA-B7 in Presumed Ocular Histoplasmosis. Am. J. Ophthalmol. 1978, 85, 859–861. [Google Scholar] [CrossRef]
- Elhassan, R.M.; Alsony, N.M.; Othman, K.M.; Izz-Aldin, D.T.; Alhaj, T.A.; Ali, A.A.; Abashir, L.A.; Ahmed, O.H.; Hassan, M.A. Epitope-Based Immunoinformatic Approach on Heat Shock 70 KDa Protein Complex of Cryptococcus Neoformans Var. Grubii. J. Immunol. Res. 2021, 2021, 1–16. [Google Scholar] [CrossRef]
- Hurtgen, B.J.; Castro-Lopez, N.; Jiménez-Alzate, M.d.P.; Cole, G.T.; Hung, C.-Y. Preclinical Identification of Vaccine Induced Protective Correlates in Human Leukocyte Antigen Expressing Transgenic Mice Infected with Coccidioides Posadasii. Vaccine 2016, 34, 5336–5343. [Google Scholar] [CrossRef] [PubMed]
- Campuzano, A.; Devi Pentakota, K.; Liao, Y.-R.; Zhang, H.; Ostroff, G.; Hung, C.-Y. A Recombinant Multivalent Vaccine (RCpa1) Induces Protection for C57BL/6 and HLA Transgenic Mice Against Pulmonary Infection 2 with Both Species of Coccidioides. bioRxiv 2021. [Google Scholar] [CrossRef]
- Kurita, N.; Biswas, S.K.; Oarada, M.; Sano, A.; Nishimura, K.; Miyaji, M. Fungistatic and Fungicidal Activities of Murine Polymorphonuclear Leucocytes against Yeast Cells of Paracoccidioides Brasiliensis. Med. Mycol. 1999, 37, 19–24. [Google Scholar] [CrossRef]
- Iwai, L.K.; Yoshida, M.; Sidney, J.; Shikanai-Yasuda, M.A.; Goldberg, A.C.; Juliano, M.A.; Hammer, J.; Juliano, L.; Sette, A.; Kalil, J.; et al. In Silico Prediction of Peptides Binding to Multiple HLA-DR Molecules Accurately Identifies Immunodominant Epitopes from Gp43 of Paracoccidioides Brasiliensis Frequently Recognized in Primary Peripheral Blood Mononuclear Cell Responses from Sensitized Ind. Mol. Med. 2003, 9, 209–219. [Google Scholar] [CrossRef]
- Iwai, L.K.; Yoshida, M.; Sadahiro, A.; da Silva, W.R.; Marin, M.L.; Goldberg, A.C.; Juliano, M.A.; Juliano, L.; Shikanai-Yasuda, M.A.; Kalil, J.; et al. T-Cell Recognition of Paracoccidioides Brasiliensis Gp43-Derived Peptides in Patients with Paracoccidioidomycosis and Healthy Individuals. Clin. Vaccine Immunol. 2007, 14, 474–476. [Google Scholar] [CrossRef]
- Travassos, L.R.; Rodrigues, E.G.; Iwai, L.K.; Taborda, C.P. Attempts at a Peptide Vaccine against Paracoccidioidomycosis, Adjuvant to Chemotherapy. Mycopathologia 2008, 165, 341–352. [Google Scholar] [CrossRef]
- de Almeida, S.M.; Rebelatto, C.L.K.; Queiroz-telles, F.; Werneck, L.C.; Monteiro, S.; Almeida, D.; Lu, C.; Queiroz-telles, F.; Cesar, L. Major Histocompatibility Complex and Central Nervous System Involvement by Paracoccidioidomycosis. J. Infect. 2005, 51, 140–143. [Google Scholar] [CrossRef] [PubMed]
- Torres, I.; Hernandez, O.; Tamayo, D.; Muñoz, J.F.; García, A.M.; Gómez, B.L.; Restrepo, A.; McEwen, J.G. Paracoccidioides Brasiliensis PbP27 Gene: Knockdown Procedures and Functional Characterization. FEMS Yeast Res. 2014, 14, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Dabil, H.; Kaplan, H.J.; Duffy, B.F.; Phelan, D.L.; Mohanakumar, T.; Jaramillo, A. Association of the HLA-DR15/HLA-DQ6 Haplotype with Development of Choroidal Neovascular Lesions in Presumed Ocular Histoplasmosis Syndrome. Hum. Immunol. 2003, 64, 960–964. [Google Scholar] [CrossRef] [PubMed]
- Kischkel, B.; Boniche-Alfaro, C.; de Menezes, I.G.; Rossi, S.A.; Angeli, C.B.; de Almeida, S.R.; Palmisano, G.; Lopes-Bezerra, L.; Nosanchuk, J.D.; Taborda, C.P. Immunoproteomic and Immunopeptidomic Analyses of Histoplasma Capsulatum Reveal Promiscuous and Conserved Epitopes Among Fungi With Vaccine Potential. Front. Immunol. 2021, 12, 764501. [Google Scholar] [CrossRef] [PubMed]
- Allendoerfer, R.; Maresca, B.; Deepe, G.S. Cellular Immune Responses to Recombinant Heat Shock Protein 70 from Histoplasma Capsulatum. Infect. Immun. 1996, 64, 4123–4128. [Google Scholar] [CrossRef] [PubMed]
- Leopold Wager, C.M.; Wormley, F.L. Is Development of a Vaccine against Cryptococcus Neoformans Feasible? PLoS Pathog. 2015, 11, e1004843. [Google Scholar] [CrossRef]
- Datta, K.; Pirofski, L. Towards a Vaccine for Cryptococcus Neoformans: Principles and Caveats. FEMS Yeast Res. 2006, 6, 525–536. [Google Scholar] [CrossRef]
- Elhassan, R.M.; Alsony, N.M.; Othman, K.M.; Izz-Aldin, D.T.; Alhaj, T.A.; Ali, A.A.; Abashir, L.A.; Ahmed, O.H.; Hassan, M.A. Computational Vaccinology Approach: Designing an Efficient Multi-Epitope Peptide Vaccine against Cryptococcus Neoformans Var. Grubii’s Heat Shock 70KDa Protein. bioRxiv 2019. [Google Scholar] [CrossRef]
- Williams, P.L.; Sable, D.L.; Sorgen, S.P.; Pappagianis, D.; Levine, H.B.; Brodine, S.K.; Brown, B.W.; Grumet, F.C.; Stevens, D.A. Immunologic Responsiveness and Safety Associated with the Coccidioides Immitis Spherule Vaccine in Volunteers of White, Black, and Filipino Ancestry. Am. J. Epidemiol. 1984, 119, 591–602. [Google Scholar] [CrossRef]
- Soleymani, S.; Tavassoli, A.; Housaindokht, M.R. An Overview of Progress from Empirical to Rational Design in Modern Vaccine Development, with an Emphasis on Computational Tools and Immunoinformatics Approaches. Comput. Biol. Med. 2021, 140, 105057. [Google Scholar] [CrossRef]
- Bonilla, F.A.; Boston, P. Update: Vaccines in Primary Immunodeficiency. J. Allergy Clin. Immunol. 2018, 141, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Almeida, F.; Rodrigues, M.L.; Coelho, C. The Still Underestimated Problem of Fungal Diseases Worldwide. Front. Microbiol. 2019, 10, 214. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, N.; Singh, A.; Upadhyay, A.K.; Mannan, M.A.-u. Design of a Multi-Epitope Vaccine against the Pathogenic Fungi Candida Tropicalis Using an in Silico Approach. J. Genet. Eng. Biotechnol. 2022, 20, 140. [Google Scholar] [CrossRef]
- World Health Organization. WHO Fungal Priority Pathogens List to Guide Research, Development and Public Health Action; World Health Organization: Geneva, Switzerland, 2022; Volume 1, ISBN 9789240060241. [Google Scholar]
- Chaudhuri, R.; Ansari, F.A.; Raghunandanan, M.V.; Ramachandran, S. FungalRV: Adhesin Prediction and Immunoinformatics Portal for Human Fungal Pathogens. BMC Genom. 2011, 12, 192. [Google Scholar] [CrossRef] [PubMed]
- Almeida, P.C.S.; Roque, B.S.; Felice, A.G.; Jaiswal, A.K.; Tiwari, S.; Azevedo, V.; Silva-Vergara, M.L.; de Castro Soares, S.; Ferreira-Paim, K.; Fonseca, F.M. Comparative Genomics of Histoplasma Capsulatum and Prediction of New Vaccines and Drug Targets. J. Fungi 2023, 9, 193. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.K.; Osmanoglu, Ö.; Minocha, R.; Bandi, S.R.; Bencurova, E.; Srivastava, M.; Dandekar, T. Genome-Wide Scan for Potential CD4+ T-Cell Vaccine Candidates in Candida Auris by Exploiting Reverse Vaccinology and Evolutionary Information. Front. Med. 2022, 9, 1008527. [Google Scholar] [CrossRef]
- Pritam, M.; Singh, G.; Kumar, R.; Singh, S.P. Screening of Potential Antigens from Whole Proteome and Development of Multi-Epitope Vaccine against Rhizopus Delemar Using Immunoinformatics Approaches. J. Biomol. Struct. Dyn. 2023, 41, 2118–2145. [Google Scholar] [CrossRef]
- Portuondo, D.L.; Batista-Duharte, A.; Cardenas, C.; de Oliveira, C.S.; Borges, J.C.; Téllez-Martínez, D.; Santana, P.A.; Gauna, A.; Mercado, L.; Mateus de Castilho, B.; et al. A Sporothrix Spp. Enolase Derived Multi-Epitope Vaccine Confers Protective Response in BALB/c Mice Challenged with Sporothrix Brasiliensis. Microb. Pathog. 2022, 166, 105539. [Google Scholar] [CrossRef]
- Elamin Elhasan, L.M.; Hassan, M.B.; Elhassan, R.M.; Abdelrhman, F.A.; Salih, E.A.; Ibrahim, H.A.; Mohamed, A.A.; Osman, H.S.; Khalil, M.S.M.; Alsafi, A.A.; et al. Epitope-Based Peptide Vaccine Design against Fructose Bisphosphate Aldolase of Candida Glabrata: An Immunoinformatics Approach. J. Immunol. Res. 2021, 2021, 1–19. [Google Scholar] [CrossRef]
- Akhtar, N.; Magdaleno, J.S.L.; Ranjan, S.; Wani, A.K.; Grewal, R.K.; Oliva, R.; Shaikh, A.R.; Cavallo, L.; Chawla, M. Secreted Aspartyl Proteinases Targeted Multi-Epitope Vaccine Design for Candida Dubliniensis Using Immunoinformatics. Vaccines 2023, 11, 364. [Google Scholar] [CrossRef]
- Kamli, M.R.; Sabir, J.S.M.; Malik, M.A.; Ahmad, A. Characterization of the Secretome of Pathogenic Candida Glabrata and Their Effectiveness against Systemic Candidiasis in BALB/c Mice for Vaccine Development. Pharmaceutics 2022, 14, 1989. [Google Scholar] [CrossRef] [PubMed]
- Soltan, M.A.; Eldeen, M.A.; Elbassiouny, N.; Kamel, H.L.; Abdelraheem, K.M.; El-Gayyed, H.A.; Gouda, A.M.; Sheha, M.F.; Fayad, E.; Ali, O.A.A.; et al. In Silico Designing of a Multitope Vaccine against Rhizopus Microsporus with Potential Activity against Other Mucormycosis Causing Fungi. Cells 2021, 10, 3014. [Google Scholar] [CrossRef] [PubMed]
- Khan, T.; Suleman, M.; Ali, S.S.; Sarwar, M.F.; Ali, I.; Ali, L.; Khan, A.; Rokhan, B.; Wang, Y.; Zhao, R.; et al. Subtractive Proteomics Assisted Therapeutic Targets Mining and Designing Ensemble Vaccine against Candida Auris for Immune Response Induction. Comput. Biol. Med. 2022, 145, 105462. [Google Scholar] [CrossRef] [PubMed]
- Duraes, F.V.; Niven, J.; Dubrot, J.; Hugues, S.; Gannagé, M. Macroautophagy in Endogenous Processing of Self- and Pathogen-Derived Antigens for MHC Class II Presentation. Front. Immunol. 2015, 6, 459. [Google Scholar] [CrossRef] [PubMed]
- Sette, A.; Rappuoli, R. Reverse Vaccinology: Developing Vaccines in the Era of Genomics. Immunity 2010, 33, 530–541. [Google Scholar] [CrossRef]
- Vita, R.; Mahajan, S.; Overton, J.A.; Dhanda, S.K.; Martini, S.; Cantrell, J.R.; Wheeler, D.K.; Sette, A.; Peters, B. The Immune Epitope Database (IEDB): 2018 Update. Nucleic Acids Res. 2019, 47, D339–D343. [Google Scholar] [CrossRef]
- Paul, S.; Lindestam Arlehamn, C.S.; Scriba, T.J.; Dillon, M.B.C.; Oseroff, C.; Hinz, D.; McKinney, D.M.; Carrasco Pro, S.; Sidney, J.; Peters, B.; et al. Development and Validation of a Broad Scheme for Prediction of HLA Class II Restricted T Cell Epitopes. J. Immunol. Methods 2015, 422, 28–34. [Google Scholar] [CrossRef]
- Cezar-dos-Santos, F.; Assolini, J.P.; Okuyama, N.C.M.; Viana, K.F.; de Oliveira, K.B.; Itano, E.N. Unraveling the Susceptibility of Paracoccidioidomycosis: Insights towards the Pathogen-Immune Interplay and Immunogenetics. Infect. Genet. Evol. 2020, 86, 104586. [Google Scholar] [CrossRef]
- Kar, P.; Ruiz-Perez, L.; Arooj, M.; Mancera, R.L. Current Methods for the Prediction of T-Cell Epitopes. Pept. Sci. 2018, 110, e24046. [Google Scholar] [CrossRef]
- Dhanda, S.K.; Mahajan, S.; Paul, S.; Yan, Z.; Kim, H.; Jespersen, M.C.; Jurtz, V.; Andreatta, M.; Greenbaum, J.A.; Marcatili, P.; et al. IEDB-AR: Immune Epitope Database - Analysis Resource in 2019. Nucleic Acids Res. 2019, 47, W502–W506. [Google Scholar] [CrossRef]
- Ansari, H.R.; Raghava, G.P. Identification of Conformational B-Cell Epitopes in an Antigen from Its Primary Sequence. Immunome Res. 2010, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Reynisson, B.; Alvarez, B.; Paul, S.; Peters, B.; Nielsen, M. NetMHCpan-4.1 and NetMHCIIpan-4.0: Improved Predictions of MHC Antigen Presentation by Concurrent Motif Deconvolution and Integration of MS MHC Eluted Ligand Data. Nucleic Acids Res. 2020, 48, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, S.; Parmar, J.; Kumar, A. Structure-Based Immunogenicity Prediction of Uricase from Fungal (Aspergillus Flavus), Bacterial (Bacillus Subtillis) and Mammalian Sources Using Immunoinformatic Approach. Protein J. 2020, 39, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Bhargav, A.; Fatima, F.; Chaurasia, P.; Seth, S.; Ramachandran, S. Computer-Aided Tools and Resources for Fungal Pathogens: An Application of Reverse Vaccinology for Mucormycosis. Monoclon. Antibodies Immunodiagn. Immunother. 2022, 41, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Raghava, G.P.S. ProPred1: Prediction of Promiscuous MHC Class-I Binding Sites. Bioinformatics 2003, 19, 1009–1014. [Google Scholar] [CrossRef]
- Reche, P.A.; Glutting, J.P.; Zhang, H.; Reinherz, E.L. Enhancement to the RANKPEP Resource for the Prediction of Peptide Binding to MHC Molecules Using Profiles. Immunogenetics 2004, 56, 405–419. [Google Scholar] [CrossRef]
- Bhasin, M.; Raghava, G.P.S. A Hybrid Approach for Predicting Promiscuous MHC Class I Restricted T Cell Epitopes. J. Biosci. 2007, 32, 31–42. [Google Scholar] [CrossRef]
- Specht, C.A.; Homan, E.J.; Lee, C.K.; Mou, Z.; Gomez, C.L.; Hester, M.M.; Abraham, A.; Rus, F.; Ostroff, G.R.; Levitz, S.M. Protection of Mice against Experimental Cryptococcosis by Synthesized Peptides Delivered in Glucan Particles. mBio 2022, 13. [Google Scholar] [CrossRef]
- Zhang, J.; Zhao, X.; Sun, P.; Gao, B.; Ma, Z. Conformational B-Cell Epitopes Prediction from Sequences Using Cost-Sensitive Ensemble Classifiers and Spatial Clustering. BioMed Res. Int. 2014, 2014, 689219. [Google Scholar] [CrossRef]
- Kalita, P.; Tripathi, T. Methodological Advances in the Design of Peptide-Based Vaccines. Drug Discov. Today 2022, 27, 1367–1380. [Google Scholar] [CrossRef]
- Sharma, V.; Singh, S.; Ratnakar, T.S.; Prajapati, V.K. Immunoinformatics and Reverse Vaccinology Methods to Design Peptide-Based Vaccines. In Advances in Protein Molecular and Structural Biology Methods; Academic Press: Cambridge, MA, USA, 2022; pp. 477–487. ISBN 9780323902649. [Google Scholar]
- Rodrigues, A.M.; Kubitschek-Barreira, P.H.; Fernandes, G.F.; de Almeida, S.R.; Lopes-Bezerra, L.M.; de Camargo, Z.P. Immunoproteomic Analysis Reveals a Convergent Humoral Response Signature in the Sporothrix Schenckii Complex. J. Proteom. 2015, 115, 8–22. [Google Scholar] [CrossRef] [PubMed]
- Martins, L.M.S.; De Andrade, H.M.; Vainstein, M.H.; Wanke, B.; Schrank, A.; Balaguez, C.B.; Dos Santos, P.R.; Santi, L.; Pires, S.D.F.; Da Silva, A.S.; et al. Immunoproteomics and Immunoinformatics Analysis of Cryptococcus Gattii: Novel Candidate Antigens for Diagnosis. Future Microbiol. 2013, 8, 549–563. [Google Scholar] [CrossRef] [PubMed]
- Sircar, G.; Jana, K.; Dasgupta, A.; Saha, S.; Bhattacharya, S.G. Epitope Mapping of Rhi o 1 and Generation of a Hypoallergenic Variant. J. Biol. Chem. 2016, 291, 18016–18029. [Google Scholar] [CrossRef]
- Moreira, A.L.E.; Oliveira, M.A.P.; Silva, L.O.S.; Inácio, M.M.; Bailão, A.M.; Parente-Rocha, J.A.; Cruz-Leite, V.R.M.; Paccez, J.D.; de Almeida Soares, C.M.; Weber, S.S.; et al. Immunoproteomic Approach of Extracellular Antigens From Paracoccidioides Species Reveals Exclusive B-Cell Epitopes. Front. Microbiol. 2020, 10, 2968. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, A.M.; Kubitschek-Barreira, P.H.; Pinheiro, B.G.; Teixeira-Ferreira, A.; Hahn, R.C.; de Camargo, Z.P. Immunoproteomic Analysis Reveals Novel Candidate Antigens for the Diagnosis of Paracoccidioidomycosis Due to Paracoccidioides Lutzii. J. Fungi 2020, 6, 357. [Google Scholar] [CrossRef]
- Kringelum, J.V.; Lundegaard, C.; Lund, O.; Nielsen, M. Reliable B Cell Epitope Predictions: Impacts of Method Development and Improved Benchmarking. PLoS Comput. Biol. 2012, 8, e1002829. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Chen, Z.; Zhang, L.; Yan, D.; Mao, T.; Tang, K.; Qiu, T.; Cao, Z. SEPPA 3.0—Enhanced Spatial Epitope Prediction Enabling Glycoprotein Antigens. Nucleic Acids Res. 2019, 47, W388–W394. [Google Scholar] [CrossRef]
- Sweredoski, M.J.; Baldi, P. PEPITO: Improved Discontinuous B-Cell Epitope Prediction Using Multiple Distance Thresholds and Half Sphere Exposure. Bioinformatics 2008, 24, 1459–1460. [Google Scholar] [CrossRef]
- Ponomarenko, J.; Bui, H.-H.H.; Li, W.; Fusseder, N.; Bourne, P.E.; Sette, A.; Peters, B. ElliPro: A New Structure-Based Tool for the Prediction of Antibody Epitopes. BMC Bioinform. 2008, 9, 514. [Google Scholar] [CrossRef]
- Rubinstein, N.D.; Mayrose, I.; Martz, E.; Pupko, T. Epitopia: A Web-Server for Predicting B-Cell Epitopes. BMC Bioinform. 2009, 10, 287. [Google Scholar] [CrossRef]
- Xu, X.L.; Sun, J.; Liu, Q.; Wang, X.J.; Xu, T.L.; Zhu, R.X.; Wu, D.; Cao, Z.W. Evaluation of Spatial Epitope Computational Tools Based on Experimentally-Confirmed Dataset for Protein Antigens. Chin. Sci. Bull. 2010, 55, 2169–2174. [Google Scholar] [CrossRef]
- El-Manzalawy, Y.; Dobbs, D.; Honavar, V.G. In Silico Prediction of Linear B-Cell Epitopes on Proteins. Methods Mol. Biol. 2017, 1484, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.A.; Ami, J.Q.; Faisal, K.; Chowdhury, R.; Ghosh, P.; Hossain, F.; Abd El Wahed, A.; Mondal, D. An Immunoinformatic Approach Driven by Experimental Proteomics: In Silico Design of a Subunit Candidate Vaccine Targeting Secretory Proteins of Leishmania Donovani Amastigotes. Parasites Vectors 2020, 13, 1–21. [Google Scholar] [CrossRef]
- Sanches, R.C.O.; Tiwari, S.; Ferreira, L.C.G.; Oliveira, F.M.; Lopes, M.D.; Passos, M.J.F.; Maia, E.H.B.; Taranto, A.G.; Kato, R.; Azevedo, V.A.C.; et al. Immunoinformatics Design of Multi-Epitope Peptide-Based Vaccine Against Schistosoma Mansoni Using Transmembrane Proteins as a Target. Front. Immunol. 2021, 12, 490. [Google Scholar] [CrossRef] [PubMed]
- Vilela Rodrigues, T.C.; Jaiswal, A.K.; Lemes, M.R.; da Silva, M.V.; Sales-Campos, H.; Alcântara, L.C.J.; de Tosta, S.F.O.; Kato, R.B.; Alzahrani, K.J.; Barh, D.; et al. An Immunoinformatics-Based Designed Multi-Epitope Candidate Vaccine (Mpme-VAC/STV-1) against Mycoplasma Pneumoniae. Comput. Biol. Med. 2022, 142, 105194. [Google Scholar] [CrossRef]
- Doytchinova, I.A.; Flower, D.R. VaxiJen: A Server for Prediction of Protective Antigens, Tumour Antigens and Subunit Vaccines. BMC Bioinform. 2007, 8, 4. [Google Scholar] [CrossRef]
- Vivona, S.; Bernante, F.; Filippini, F. NERVE: New Enhanced Reverse Vaccinology Environment. BMC Biotechnol. 2006, 6, 35. [Google Scholar] [CrossRef]
- Xiang, Z.; He, Y. Vaxign: A Web-Based Vaccine Target Design Program for Reverse Vaccinology. Procedia Vaccinol. 2009, 1, 23–29. [Google Scholar] [CrossRef]
- Magnan, C.N.; Zeller, M.; Kayala, M.A.; Vigil, A.; Randall, A.; Felgner, P.L.; Baldi, P. High-Throughput Prediction of Protein Antigenicity Using Protein Microarray Data. Bioinformatics 2010, 26, 2936–2943. [Google Scholar] [CrossRef]
- Jaiswal, V.; Chanumolu, S.K.; Gupta, A.; Chauhan, R.S.; Rout, C. Jenner-Predict Server: Prediction of Protein Vaccine Candidates (PVCs) in Bacteria Based on Host-Pathogen Interactions. BMC Bioinform. 2013, 14, 211. [Google Scholar] [CrossRef]
- Moise, L.; Gutierrez, A.; Kibria, F.; Martin, R.; Tassone, R.; Liu, R.; Terry, F.; Martin, B.; De Groot, A.S. Ivax: An Integrated Toolkit for the Selection and Optimization of Antigens and the Design of Epitope-Driven Vaccines. Hum. Vaccines Immunother. 2015, 11, 2312–2321. [Google Scholar] [CrossRef] [PubMed]
- Rizwan, M.; Naz, A.; Ahmad, J.; Naz, K.; Obaid, A.; Parveen, T.; Ahsan, M.; Ali, A. VacSol: A High Throughput in Silico Pipeline to Predict Potential Therapeutic Targets in Prokaryotic Pathogens Using Subtractive Reverse Vaccinology. BMC Bioinform. 2017, 18, 106. [Google Scholar] [CrossRef] [PubMed]
- Doytchinova, I. Flower DR Bioinformatic Approach for Identifying Parasite and Fungal Candidate Subunit Vaccines. Open Vaccine J. 2008, 1, 4. [Google Scholar] [CrossRef]
- Flower, D.R.; Doytchinova, I.; Zaharieva, N.; Dimitrov, I. Immunogenicity Prediction by VaxiJen: A Ten Year Overview. J. Proteomics Bioinform. 2017, 10, 298–310. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inácio, M.M.; Moreira, A.L.E.; Cruz-Leite, V.R.M.; Mattos, K.; Silva, L.O.S.; Venturini, J.; Ruiz, O.H.; Ribeiro-Dias, F.; Weber, S.S.; Soares, C.M.d.A.; et al. Fungal Vaccine Development: State of the Art and Perspectives Using Immunoinformatics. J. Fungi 2023, 9, 633. https://0-doi-org.brum.beds.ac.uk/10.3390/jof9060633
Inácio MM, Moreira ALE, Cruz-Leite VRM, Mattos K, Silva LOS, Venturini J, Ruiz OH, Ribeiro-Dias F, Weber SS, Soares CMdA, et al. Fungal Vaccine Development: State of the Art and Perspectives Using Immunoinformatics. Journal of Fungi. 2023; 9(6):633. https://0-doi-org.brum.beds.ac.uk/10.3390/jof9060633
Chicago/Turabian StyleInácio, Moisés Morais, André Luís Elias Moreira, Vanessa Rafaela Milhomem Cruz-Leite, Karine Mattos, Lana O’Hara Souza Silva, James Venturini, Orville Hernandez Ruiz, Fátima Ribeiro-Dias, Simone Schneider Weber, Célia Maria de Almeida Soares, and et al. 2023. "Fungal Vaccine Development: State of the Art and Perspectives Using Immunoinformatics" Journal of Fungi 9, no. 6: 633. https://0-doi-org.brum.beds.ac.uk/10.3390/jof9060633