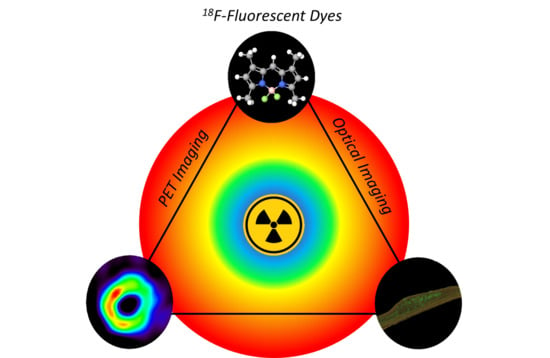
Fluorine-18-Labeled Fluorescent Dyes for Dual-Mode Molecular Imaging
Abstract
:1. Introduction
2. 18F-Labeled Fluorescent Dyes
2.1. BODIPYs
2.2. Fluoresceins and Rhodamines
2.3. Cyanines
2.4. Curcumins
2.5. Others
3. Applications
3.1. Tumor Imaging
3.2. Cardiac Imaging
3.3. Brain Imaging
3.4. Other Applications
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gambhir, S.S. Molecular imaging of cancer with positron emission tomography. Nat. Rev. Cancer 2002, 2, 683–693. [Google Scholar] [CrossRef]
- Giepmans, B.N.G.; Adams, S.R.; Ellisman, M.H.; Tsien, R.Y. The Fluorescent Toolbox for Assessing Protein Location and Function. Science 2006, 312, 217–224. [Google Scholar] [CrossRef] [Green Version]
- Swift, L.M.; Sarvazyan, N. Localization of dichlorofluorescin in cardiac myocytes: Implications for assessment of oxidative stress. Am. J. Physiol. Heart Circ. Physiol. 2000, 278, H982–H990. [Google Scholar] [CrossRef]
- Razgulin, A.; Ma, N.; Rao, J. Strategies for in vivo imaging of enzyme activity: An overview and recent advances. Chem. Soc. Rev. 2011, 40, 4186–4216. [Google Scholar] [CrossRef]
- New, E.J.; Parker, D.; Smith, D.G.; Walton, J.W. Development of responsive lanthanide probes for cellular applications. Curr. Opin. Chem. Biol. 2010, 14, 238–246. [Google Scholar] [CrossRef]
- Hustinx, R.; Bénard, F.; Alavi, A. Whole-body FDG-PET imaging in the management of patients with cancer. Semin. Nucl. Med. 2002, 32, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Lonneux, M.; Reffad, A.-M.; Detry, R.; Kartheuser, A.; Gigot, J.-F.; Pauwels, S. FDG-PET improves the staging and selection of patients with recurrent colorectal cancer. Eur. J. Nucl. Med. 2002, 29, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Fallavollita, J.A.; Dare, J.D.; Carter, R.L.; Baldwa, S.; Canty, J.M. Denervated Myocardium Is Preferentially Associated with Sudden Cardiac Arrest in Ischemic Cardiomyopathy: A Pilot Competing Risks Analysis of Cause-Specific Mortality. Circ. Cardiovasc. Imaging 2017, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Belykh, E.; Martirosyan, N.L.; Yagmurlu, K.; Miller, E.J.; Eschbacher, J.M.; Izadyyazdanabadi, M.; Bardonova, L.A.; Byvaltsev, V.A.; Nakaji, P.; Preul, M.C. Intraoperative Fluorescence Imaging for Personalized Brain Tumor Resection: Current State and Future Directions. Front. Surg. 2016, 3. [Google Scholar] [CrossRef] [Green Version]
- Dizdarevic, S.; Peters, A.M. Imaging of multidrug resistance in cancer. Cancer Imaging 2011, 11, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Massoud, T.F.; Gambhir, S.S. Molecular imaging in living subjects: Seeing fundamental biological processes in a new light. Genes Dev. 2003, 17, 545–580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Louie, A. Multimodality Imaging Probes: Design and Challenges. Chem. Rev. 2010, 110, 3146–3195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.; Chen, J.; Ma, S.; Liu, Q.; Huang, L.; Chen, X.; Lou, K.; Wang, W. Recent developments in multimodality fluorescence imaging probes. Acta Pharm. Sin. B 2018, 8, 320–338. [Google Scholar] [CrossRef] [PubMed]
- Shaner, N.C.; Steinbach, P.A.; Tsien, R.Y. A guide to choosing fluorescent proteins. Nat. Methods 2005, 2, 905–909. [Google Scholar] [CrossRef] [PubMed]
- Numasawa, K.; Hanaoka, K.; Saito, N.; Yamaguchi, Y.; Ikeno, T.; Echizen, H.; Yasunaga, M.; Komatsu, T.; Ueno, T.; Miura, M.; et al. A Fluorescent Probe for Rapid, High-Contrast Visualization of Folate-Receptor-Expressing Tumors In Vivo. Angew. Chem. Int. Ed. 2020, 59, 6015–6020. [Google Scholar] [CrossRef]
- Chinen, A.B.; Guan, C.M.; Ferrer, J.R.; Barnaby, S.N.; Merkel, T.J.; Mirkin, C.A. Nanoparticle Probes for the Detection of Cancer Biomarkers, Cells, and Tissues by Fluorescence. Chem. Rev. 2015, 115, 10530–10574. [Google Scholar] [CrossRef] [Green Version]
- Yong, K.-T.; Ding, H.; Roy, I.; Law, W.-C.; Bergey, E.J.; Maitra, A.; Prasad, P.N. Imaging Pancreatic Cancer Using Bioconjugated InP Quantum Dots. ACS Nano 2009, 3, 502–510. [Google Scholar] [CrossRef]
- Ntziachristos, V. Going deeper than microscopy: The optical imaging frontier in biology. Nat. Methods 2010, 7, 603–614. [Google Scholar] [CrossRef]
- Miller, M.J.; Wei, S.H.; Parker, I.; Cahalan, M.D. Two-Photon Imaging of Lymphocyte Motility and Antigen Response in Intact Lymph Node. Science 2002, 296, 1869–1873. [Google Scholar] [CrossRef] [Green Version]
- Zhu, L.; Ma, Y.; Kiesewetter, D.O.; Wang, Y.; Lang, L.; Lee, S.; Niu, G.; Chen, X. Rational Design of Matrix Metalloproteinase-13 Activatable Probes for Enhanced Specificity. ACS Chem. Biol. 2014, 9, 510–516. [Google Scholar] [CrossRef] [Green Version]
- Azarias, C.; Budzák, Š.; Laurent, A.D.; Ulrich, G.; Jacquemin, D. Tuning ESIPT fluorophores into dual emitters. Chem. Sci. 2016, 7, 3763–3774. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frath, D.; Didier, P.; Mély, Y.; Massue, J.; Ulrich, G. Vectorization and Intracellular Distribution of a Two-Photon-Absorbing, Near-Infrared-Emitting π-Extended Boranil Dye. ChemPhotoChem 2017, 1, 109–112. [Google Scholar] [CrossRef]
- Lin, S.; Xie, X.; Patel, M.R.; Yang, Y.-H.; Li, Z.; Cao, F.; Gheysens, O.; Zhang, Y.; Gambhir, S.S.; Rao, J.H.; et al. Quantum dot imaging for embryonic stem cells. BMC Biotechnol. 2007, 7, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zanzonico, P. Principles of Nuclear Medicine Imaging: Planar, SPECT, PET, Multi-modality, and Autoradiography Systems. Radiat. Res. 2012, 177, 349–364. [Google Scholar] [CrossRef]
- Adumeau, P.; Carnazza, K.E.; Brand, C.; Carlin, S.D.; Reiner, T.; Agnew, B.J.; Lewis, J.S.; Zeglis, B.M. A Pretargeted Approach for the Multimodal PET/NIRF Imaging of Colorectal Cancer. Theranostics 2016, 6, 2267–2277. [Google Scholar] [CrossRef]
- Kang, C.M.; Koo, H.-J.; An, G.I.; Choe, Y.S.; Choi, J.Y.; Lee, K.-H.; Kim, B.-T. Hybrid PET/optical imaging of integrin αVβ3 receptor expression using a 64 Cu-labeled streptavidin/biotin-based dimeric RGD peptide. EJNMMI Res. 2015, 5, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Li, D.; Zhang, J.; Chi, C.; Xiao, X.; Wang, J.; Lang, L.; Ali, I.; Niu, G.; Zhang, L.; Tian, J.; et al. First-in-human study of PET and optical dual-modality image-guided surgery in glioblastoma using 68 Ga-IRDye800CW-BBN. Theranostics 2018, 8, 2508–2520. [Google Scholar] [CrossRef]
- Morais, M.; Campello, M.P.C.; Xavier, C.; Heemskerk, J.; Correia, J.D.G.; Lahoutte, T.; Caveliers, V.; Hernot, S.; Santos, I. Radiolabeled Mannosylated Dextran Derivatives Bearing an NIR-Fluorophore for Sentinel Lymph Node Imaging. Bioconjugate Chem. 2014, 25, 1963–1970. [Google Scholar] [CrossRef]
- Hong, H.; Zhang, Y.; Severin, G.W.; Yang, Y.; Engle, J.W.; Niu, G.; Nickles, R.J.; Chen, X.; Leigh, B.R.; Barnhart, T.E.; et al. Multimodality Imaging of Breast Cancer Experimental Lung Metastasis with Bioluminescence and a Monoclonal Antibody Dual-Labeled with 89Zr and IRDye 800CW. Mol. Pharm. 2012, 9, 2339–2349. [Google Scholar] [CrossRef] [Green Version]
- Zeglis, B.M.; Davis, C.B.; Abdel-Atti, D.; Carlin, S.D.; Chen, A.; Aggeler, R.; Agnew, B.J.; Lewis, J.S. Chemoenzymatic Strategy for the Synthesis of Site-Specifically Labeled Immunoconjugates for Multimodal PET and Optical Imaging. Bioconjugate Chem. 2014, 25, 2123–2128. [Google Scholar] [CrossRef] [Green Version]
- Pham, T.T.; Lu, Z.; Davis, C.; Li, C.; Sun, F.; Maher, J.; Yan, R. Iodine-124 Based Dual Positron Emission Tomography and Fluorescent Labeling Reagents for In Vivo Cell Tracking. Bioconjugate Chem. 2020, 31, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- Zettlitz, K.A.; Tsai, W.-T.K.; Knowles, S.M.; Kobayashi, N.; Donahue, T.R.; Reiter, R.E.; Wu, A.M. Dual-Modality Immuno-PET and Near-Infrared Fluorescence Imaging of Pancreatic Cancer Using an Anti–Prostate Stem Cell Antigen Cys-Diabody. J. Nucl. Med. 2018, 59, 1398–1405. [Google Scholar] [CrossRef] [PubMed]
- Lehtiö, K.; Oikonen, V.; Grönroos, T.; Eskola, O.; Kalliokoski, K.; Bergman, J.; Solin, O.; Grénman, R.; Nuutila, P.; Minn, H. Imaging of Blood Flow and Hypoxia in Head and Neck Cancer: Initial Evaluation with [15O]H2O and [18F]Fluoroerythronitroimidazole PET. J. Nucl. Med. 2001, 42, 1643–1652. [Google Scholar] [PubMed]
- Suzuki, K.; Yoshida, Y. Production of [13N]NH3 with ultra-high specific activity. Appl. Radiat. Isot. 1999, 50, 497–503. [Google Scholar] [CrossRef]
- Dweck, M.R.; Chow, M.W.L.; Joshi, N.V.; Williams, M.C.; Jones, C.; Fletcher, A.M.; Richardson, H.; White, A.; McKillop, G.; van Beek, E.J.R.; et al. Coronary Arterial 18F-Sodium Fluoride Uptake: A Novel Marker of Plaque Biology. J. Am. Coll. Cardiol. 2012, 59, 1539–1548. [Google Scholar] [CrossRef] [Green Version]
- Hu, K.; Patnaik, D.; Collier, T.L.; Lee, K.N.; Gao, H.; Swoyer, M.R.; Rotstein, B.H.; Krishnan, H.S.; Liang, S.H.; Wang, J.; et al. Development of [18F]Maleimide-Based Glycogen Synthase Kinase-3β Ligands for Positron Emission Tomography Imaging. ACS Med. Chem. Lett. 2017, 8, 287–292. [Google Scholar] [CrossRef] [Green Version]
- Verhoog, S.; Kee, C.W.; Wang, Y.; Khotavivattana, T.; Wilson, T.C.; Kersemans, V.; Smart, S.; Tredwell, M.; Davis, B.G.; Gouverneur, V. 18F-Trifluoromethylation of Unmodified Peptides with 5-18F-(Trifluoromethyl)dibenzothiophenium Trifluoromethanesulfonate. J. Am. Chem. Soc. 2018, 140, 1572–1575. [Google Scholar] [CrossRef]
- Wei, W.; Rosenkrans, Z.T.; Liu, J.; Huang, G.; Luo, Q.-Y.; Cai, W. ImmunoPET: Concept, Design, and Applications. Chem. Rev. 2020, 120, 3787–3851. [Google Scholar] [CrossRef]
- Jin, Q.; Zhu, W.; Jiang, D.; Zhang, R.; Kutyreff, C.J.; Engle, J.W.; Huang, P.; Cai, W.; Liu, Z.; Cheng, L. Ultra-small iron-gallic acid coordination polymer nanoparticles for chelator-free labeling of 64Cu and multimodal imaging-guided photothermal therapy. Nanoscale 2017, 9, 12609–12617. [Google Scholar] [CrossRef]
- Seibold, U.; Wängler, B.; Schirrmacher, R.; Wängler, C. Bimodal Imaging Probes for Combined PET and OI: Recent Developments and Future Directions for Hybrid Agent Development. Biomed Res. Int. 2014, 2014, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Shi, X.; Gao, K.; Gao, R. 64Cu-Based Pretargeted Immuno-Positron Emission Tomography and Near-Infrared Fluorescence Imaging of the Vascular Endothelial Growth Factor. ACS Omega 2019, 4, 5310–5316. [Google Scholar] [CrossRef]
- Li, Z.; Lin, T.-P.; Liu, S.; Huang, C.-W.; Hudnall, T.W.; Gabbaï, F.P.; Conti, P.S. Rapid aqueous [18F]-labeling of a bodipy dye for positron emission tomography/fluorescence dual modality imaging. Chem. Commun. 2011, 47, 9324. [Google Scholar] [CrossRef] [PubMed]
- Ting, R.; Aguilera, T.A.; Crisp, J.L.; Hall, D.J.; Eckelman, W.C.; Vera, D.R.; Tsien, R.Y. Fast 18F Labeling of a Near-Infrared Fluorophore Enables Positron Emission Tomography and Optical Imaging of Sentinel Lymph Nodes. Bioconjugate Chem. 2010, 21, 1811–1819. [Google Scholar] [CrossRef] [PubMed]
- Preshlock, S.; Tredwell, M.; Gouverneur, V. 18F-Labeling of Arenes and Heteroarenes for Applications in Positron Emission Tomography. Chem. Rev. 2016, 116, 719–766. [Google Scholar] [CrossRef]
- Chansaenpak, K.; Vabre, B.; Gabbaï, F.P. [18F]-Group 13 fluoride derivatives as radiotracers for positron emission tomography. Chem. Soc. Rev. 2016, 45, 954–971. [Google Scholar] [CrossRef]
- Ducongé, F.; Pons, T.; Pestourie, C.; Hérin, L.; Thézé, B.; Gombert, K.; Mahler, B.; Hinnen, F.; Kühnast, B.; Dollé, F.; et al. Fluorine-18-Labeled Phospholipid Quantum Dot Micelles for in Vivo Multimodal Imaging from Whole Body to Cellular Scales. Bioconjugate Chem. 2008, 19, 1921–1926. [Google Scholar] [CrossRef]
- Liu, Q.; Sun, Y.; Li, C.; Zhou, J.; Li, C.; Yang, T.; Zhang, X.; Yi, T.; Wu, D.; Li, F. 18F-Labeled Magnetic-Upconversion Nanophosphors via Rare-Earth Cation-Assisted Ligand Assembly. ACS Nano 2011, 5, 3146–3157. [Google Scholar] [CrossRef]
- Liu, Y.; Welch, M.J. Nanoparticles Labeled with Positron Emitting Nuclides: Advantages, Methods, and Applications. Bioconjugate Chem. 2012, 23, 671–682. [Google Scholar] [CrossRef]
- Klenner, M.A.; Pascali, G.; Massi, M.; Fraser, B.H. Fluorine-18 Radiolabelling and Photophysical Characteristics of Multimodal PET–Fluorescence Molecular Probes. Chem. Eur. J. 2020. [Google Scholar] [CrossRef]
- Treibs, A.; Kreuzer, F.-H. Difluorboryl-Komplexe von Di- und Tripyrrylmethenen. Justus Liebigs Ann. Chem. 1968, 718, 208–223. [Google Scholar] [CrossRef]
- Ulrich, G.; Ziessel, R.; Harriman, A. The Chemistry of Fluorescent Bodipy Dyes: Versatility Unsurpassed. Angew. Chem. Int. Ed. 2008, 47, 1184–1201. [Google Scholar] [CrossRef] [PubMed]
- Ni, Y.; Wu, J. Far-red and near infrared BODIPY dyes: Synthesis and applications for fluorescent pH probes and bio-imaging. Org. Biomol. Chem. 2014, 12, 3774. [Google Scholar] [CrossRef] [PubMed]
- Florès, O.; Pliquett, J.; Abad Galan, L.; Lescure, R.; Denat, F.; Maury, O.; Pallier, A.; Bellaye, P.-S.; Collin, B.; Même, S.; et al. Aza-BODIPY Platform: Toward an Efficient Water-Soluble Bimodal Imaging Probe for MRI and Near-Infrared Fluorescence. Inorg. Chem. 2020, 59, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- Frenette, M.; Hatamimoslehabadi, M.; Bellinger-Buckley, S.; Laoui, S.; La, J.; Bag, S.; Mallidi, S.; Hasan, T.; Bouma, B.; Yelleswarapu, C.; et al. Shining Light on the Dark Side of Imaging: Excited State Absorption Enhancement of a Bis-styryl BODIPY Photoacoustic Contrast Agent. J. Am. Chem. Soc. 2014, 136, 15853–15856. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.; Kim, K.; Son, S.-H.; Choi, J.Y.; Lee, K.-H.; Kim, B.-T.; Byun, Y.; Choe, Y.S. 18F-Labeled BODIPY Dye: A Potential Prosthetic Group for Brain Hybrid PET/Optical Imaging Agents. ACS Chem. Neurosci. 2019, 10, 1445–1451. [Google Scholar] [CrossRef]
- Ono, M.; Watanabe, H.; Ikehata, Y.; Ding, N.; Yoshimura, M.; Sano, K.; Saji, H. Radioiodination of BODIPY and its application to a nuclear and optical dual functional labeling agent for proteins and peptides. Sci. Rep. 2017, 7, 3337. [Google Scholar] [CrossRef]
- Ali, H.; Ouellet, R.; van Lier, J.E.; Guérin, B. Radiolabeled BODIPYs: An overview. J. Porphyr. Phthalocyanines 2019, 23, 781–796. [Google Scholar] [CrossRef]
- Ting, R.; Lo, J.; Adam, M.J.; Ruth, T.J.; Perrin, D.M. Capturing aqueous [18F]-fluoride with an arylboronic ester for PET: Synthesis and aqueous stability of a fluorescent [18F]-labeled aryltrifluoroborate. J. Fluor. Chem. 2008, 129, 349–358. [Google Scholar] [CrossRef]
- Hendricks, J.A.; Keliher, E.J.; Wan, D.; Hilderbrand, S.A.; Weissleder, R.; Mazitschek, R. Synthesis of [18F]BODIPY: Bifunctional Reporter for Hybrid Optical/Positron Emission Tomography Imaging. Angew. Chem. Int. Ed. 2012, 51, 4603–4606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ortmeyer, C.P.; Haufe, G.; Schwegmann, K.; Hermann, S.; Schäfers, M.; Börgel, F.; Wünsch, B.; Wagner, S.; Hugenberg, V. Synthesis and evaluation of a [18F]BODIPY-labeled caspase-inhibitor. Bioorganic Med. Chem. 2017, 25, 2167–2176. [Google Scholar] [CrossRef]
- Liu, S.; Lin, T.-P.; Li, D.; Leamer, L.; Shan, H.; Li, Z.; Gabbaï, F.P.; Conti, P.S. Lewis Acid-Assisted Isotopic 18F-19F Exchange in BODIPY Dyes: Facile Generation of Positron Emission Tomography/Fluorescence Dual Modality Agents for Tumor Imaging. Theranostics 2013, 3, 181–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hudnall, T.W.; Gabbaï, F.P. A BODIPY boronium cation for the sensing of fluoride ions. Chem. Commun. 2008, 4596–4597. [Google Scholar] [CrossRef]
- Yuan, H.; Cho, H.; Chen, H.H.; Panagia, M.; Sosnovik, D.E.; Josephson, L. Fluorescent and radiolabeled triphenylphosphonium probes for imaging mitochondria. Chem. Commun. 2013, 49, 10361. [Google Scholar] [CrossRef] [PubMed]
- Keliher, E.J.; Klubnick, J.A.; Reiner, T.; Mazitschek, R.; Weissleder, R. Efficient Acid-Catalyzed 18F/19F Fluoride Exchange of BODIPY Dyes. ChemMedChem 2014, 9, 1368–1373. [Google Scholar] [CrossRef] [Green Version]
- Kossatz, S.; Pirovano, G.; De Souza França, P.D.; Strome, A.L.; Sunny, S.P.; Zanoni, D.K.; Mauguen, A.; Carney, B.; Brand, C.; Shah, V.; et al. Validation of the use of a fluorescent PARP1 inhibitor for the detection of oral, oropharyngeal and oesophageal epithelial cancers. Nat. Biomed. Eng. 2020, 4, 272–285. [Google Scholar] [CrossRef]
- Brizet, B.; Goncalves, V.; Bernhard, C.; Harvey, P.D.; Denat, F.; Goze, C. DMAP-BODIPY Alkynes: A Convenient Tool for Labeling Biomolecules for Bimodal PET–Optical Imaging. Chem. Eur. J. 2014, 20, 12933–12944. [Google Scholar] [CrossRef]
- Hudnall, T.W.; Lin, T.-P.; Gabbaï, F.P. Substitution of hydroxide by fluoride at the boron center of a BODIPY dye. J. Fluor. Chem. 2010, 131, 1182–1186. [Google Scholar] [CrossRef]
- Chansaenpak, K.; Wang, H.; Wang, M.; Giglio, B.; Ma, X.; Yuan, H.; Hu, S.; Wu, Z.; Li, Z. Synthesis and Evaluation of [18F]-Ammonium BODIPY Dyes as Potential Positron Emission Tomography Agents for Myocardial Perfusion Imaging. Chem. Eur. J. 2016, 22, 12122–12129. [Google Scholar] [CrossRef]
- Liu, S.; Li, D.; Zhang, Z.; Prakash, G.K.S.; Conti, P.S.; Li, Z. Efficient synthesis of fluorescent-PET probes based on [18F]BODIPY dye. Chem. Commun. 2014, 50, 7371–7373. [Google Scholar] [CrossRef]
- Paulus, A.; Desai, P.; Carney, B.; Carlucci, G.; Reiner, T.; Brand, C.; Weber, W.A. Development of a clickable bimodal fluorescent/PET probe for in vivo imaging. EJNMMI Res. 2015, 5, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Kondo, N.; Temma, T.; Deguchi, J.; Sano, K.; Ono, M.; Saji, H. Development of PEGylated peptide probes conjugated with 18F-labeled BODIPY for PET/optical imaging of MT1-MMP activity. J. Control. Release 2015, 220, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Carlucci, G.; Carney, B.; Brand, C.; Kossatz, S.; Irwin, C.P.; Carlin, S.D.; Keliher, E.J.; Weber, W.; Reiner, T. Dual-Modality Optical/PET Imaging of PARP1 in Glioblastoma. Mol. Imaging Biol. 2015, 17, 848–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paulus, A.; Maenen, M.; Drude, N.; Nascimento, E.B.M.; van Lichtenbelt, W.D.M.; Mottaghy, F.M.; Bauwens, M. Synthesis, radiosynthesis and in vitro evaluation of 18F-Bodipy-C16/triglyceride as a dual modal imaging agent for brown adipose tissue. PLoS ONE 2017, 12, e0182297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lavis, L.D. Teaching Old Dyes New Tricks: Biological Probes Built from Fluoresceins and Rhodamines. Annu. Rev. Biochem. 2017, 86, 825–843. [Google Scholar] [CrossRef]
- Beija, M.; Afonso, C.A.M.; Martinho, J.M.G. Synthesis and applications of Rhodamine derivatives as fluorescent probes. Chem. Soc. Rev. 2009, 38, 2410–2433. [Google Scholar] [CrossRef] [Green Version]
- Heinrich, T.K.; Gottumukkala, V.; Snay, E.; Dunning, P.; Fahey, F.H.; Ted Treves, S.; Packard, A.B. Synthesis of fluorine-18 labeled rhodamine B: A potential PET myocardial perfusion imaging agent. Appl. Radiat. Isot. 2010, 68, 96–100. [Google Scholar] [CrossRef] [Green Version]
- Gottumukkala, V.; Heinrich, T.K.; Baker, A.; Dunning, P.; Fahey, F.H.; Treves, S.T.; Packard, A.B. Biodistribution and stability studies of [18F]Fluoroethylrhodamine B, a potential PET myocardial perfusion agent. Nucl. Med. Biol. 2010, 37, 365–370. [Google Scholar] [CrossRef] [Green Version]
- Bartholomä, M.D.; Gottumukkala, V.; Zhang, S.; Baker, A.; Dunning, P.; Fahey, F.H.; Treves, S.T.; Packard, A.B. Effect of the Prosthetic Group on the Pharmacologic Properties of 18F-Labeled Rhodamine B, a Potential Myocardial Perfusion Agent for Positron Emission Tomography (PET). J. Med. Chem. 2012, 55, 11004–11012. [Google Scholar] [CrossRef] [Green Version]
- Bartholomä, M.D.; Zhang, S.; Akurathi, V.; Pacak, C.A.; Dunning, P.; Fahey, F.H.; Cowan, D.B.; Ted Treves, S.; Packard, A.B. 18F-labeled rhodamines as potential myocardial perfusion agents: Comparison of pharmacokinetic properties of several rhodamines. Nucl. Med. Biol. 2015, 42, 796–803. [Google Scholar] [CrossRef] [Green Version]
- Inkster, J.A.H.; Zhang, S.; Akurathi, V.; Belanger, A.; Dubey, S.; Treves, S.T.; Packard, A.B. New chemical and radiochemical routes to [18F]Rho6G-DEG-F, a delocalized lipophilic cation for myocardial perfusion imaging with PET. Med. Chem. Commun. 2017, 8, 1891–1896. [Google Scholar] [CrossRef]
- Liu, Z.; Li, Y.; Lozada, J.; Pan, J.; Lin, K.-S.; Schaffer, P.; Perrin, D.M. Rapid, one-step, high yielding 18F-labeling of an aryltrifluoroborate bioconjugate by isotope exchange at very high specific activity. J. Label. Compd. Radiopharm. 2012, 55, 491–496. [Google Scholar] [CrossRef]
- Liu, Z.; Li, Y.; Lozada, J.; Schaffer, P.; Adam, M.J.; Ruth, T.J.; Perrin, D.M. Stoichiometric Leverage: Rapid 18F-Aryltrifluoroborate Radiosynthesis at High Specific Activity for Click Conjugation. Angew. Chem. Int. Ed. 2013, 52, 2303–2307. [Google Scholar] [CrossRef] [PubMed]
- Ting, R.; Adam, M.J.; Ruth, T.J.; Perrin, D.M. Arylfluoroborates and Alkylfluorosilicates as Potential PET Imaging Agents: High-Yielding Aqueous Biomolecular 18F-Labeling. J. Am. Chem. Soc. 2005, 127, 13094–13095. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.E.; Sladen, H.L.; Biagini, S.C.G.; Blower, P.J. Inorganic approaches for radiolabelling biomolecules with fluorine-18 for imaging with Positron Emission Tomography. Dalton Trans. 2011, 40, 6196–6205. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Pourghiasian, M.; Radtke, M.A.; Lau, J.; Pan, J.; Dias, G.M.; Yapp, D.; Lin, K.-S.; Bénard, F.; Perrin, D.M. An Organotrifluoroborate for Broadly Applicable One-Step 18F-Labeling. Angew. Chem. Int. Ed. 2014, 53, 11876–11880. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Radtke, M.A.; Wong, M.Q.; Lin, K.-S.; Yapp, D.T.; Perrin, D.M. Dual Mode Fluorescent 18F-PET Tracers: Efficient Modular Synthesis of Rhodamine-[cRGD]2-[18F]-Organotrifluoroborate, Rapid, and High Yielding One-Step 18F-Labeling at High Specific Activity, and Correlated in Vivo PET Imaging and ex Vivo Fluorescence. Bioconjugate Chem. 2014, 25, 1951–1962. [Google Scholar] [CrossRef]
- Kommidi, H.; Guo, H.; Chen, N.; Kim, D.; He, B.; Wu, A.P.; Aras, O.; Ting, R. An [18F]-Positron-Emitting, Fluorescent, Cerebrospinal Fluid Probe for Imaging Damage to the Brain and Spine. Theranostics 2017, 7, 2377–2391. [Google Scholar] [CrossRef]
- Guo, H.; Kommidi, H.; Maachani, U.B.; Voronina, J.C.; Zhang, W.; Magge, R.S.; Ivanidze, J.; Wu, A.P.; Souweidane, M.M.; Aras, O.; et al. An [18F]-Positron Emitting Fluorophore Allows Safe Evaluation of Small Molecule Distribution in the CSF, CSF Fistulas, and CNS Device Placement. Mol. Pharm. 2019, 16, 3636–3646. [Google Scholar] [CrossRef]
- AlJammaz, I.; Al-Otaibi, B.; AlHindas, H.; Okarvi, S.M. Novel synthesis and initial preclinical evaluation of 18F-[FDG] labeled rhodamine: A potential PET myocardial perfusion imaging agent. Nucl. Med. Biol. 2015, 42, 804–808. [Google Scholar] [CrossRef]
- Williams, C. Researches on Chinoline and its Homologues. Trans. R. Soc. Edinb. 1857, 21, 377–401. [Google Scholar] [CrossRef] [Green Version]
- Sun, W.; Guo, S.; Hu, C.; Fan, J.; Peng, X. Recent Development of Chemosensors Based on Cyanine Platforms. Chem. Rev. 2016, 116, 7768–7817. [Google Scholar] [CrossRef] [PubMed]
- Kulinich, A.V.; Ishchenko, A.A. Merocyanine dyes: Synthesis, structure, properties and applications. Russ. Chem. Rev. 2009, 78, 141–164. [Google Scholar] [CrossRef]
- Li, B.; Lu, L.; Zhao, M.; Lei, Z.; Zhang, F. An Efficient 1064 nm NIR-II Excitation Fluorescent Molecular Dye for Deep-Tissue High-Resolution Dynamic Bioimaging. Angew. Chem. Int. Ed. 2018. [Google Scholar] [CrossRef]
- Alander, J.T.; Kaartinen, I.; Laakso, A.; Pätilä, T.; Spillmann, T.; Tuchin, V.V.; Venermo, M.; Välisuo, P. A Review of Indocyanine Green Fluorescent Imaging in Surgery. Int. J. Biomed. Imaging 2012, 2012. [Google Scholar] [CrossRef]
- Adams, A.; Mali, W.P.T.M.; Elias, S.G.; Mourik, J.E.M.; Pearlman, P.C.; van der Voort, M.; Nielsen, T. Estimation of detection limits of a clinical fluorescence optical mammography system for the near-infrared fluorophore IRDye800CW: Phantom experiments. JBO 2012, 17, 076022. [Google Scholar] [CrossRef]
- Rodriguez, E.A.; Wang, Y.; Crisp, J.L.; Vera, D.R.; Tsien, R.Y.; Ting, R. New Dioxaborolane Chemistry Enables [18F]-Positron-Emitting, Fluorescent [18F]-Multimodality Biomolecule Generation from the Solid Phase. Bioconjugate Chem. 2016, 27, 1390–1399. [Google Scholar] [CrossRef] [Green Version]
- An, F.-F.; Kommidi, H.; Chen, N.; Ting, R. A Conjugate of Pentamethine Cyanine and 18F as a Positron Emission Tomography/Near-Infrared Fluorescence Probe for Multimodality Tumor Imaging. Int. J. Mol. Sci. 2017, 18, 1214. [Google Scholar] [CrossRef] [Green Version]
- Wang, M.; Kommidi, H.; Tosi, U.; Guo, H.; Zhou, Z.; Schweitzer, M.E.; Wu, L.Y.; Singh, R.; Hou, S.; Law, B.; et al. A Murine Model for Quantitative, Real-Time Evaluation of Convection-Enhanced Delivery (RT-CED) Using an [18F]-Positron Emitting, Fluorescent Derivative of Dasatinib. Mol. Cancer 2017, 16, 2902–2912. [Google Scholar] [CrossRef] [Green Version]
- Kommidi, H.; Guo, H.; Nurili, F.; Vedvyas, Y.; Jin, M.M.; McClure, T.D.; Ehdaie, B.; Sayman, H.B.; Akin, O.; Aras, O.; et al. 18F-Positron Emitting/Trimethine Cyanine-Fluorescent Contrast for Image-Guided Prostate Cancer Management. J. Med. Chem. 2018, 61, 4256–4262. [Google Scholar] [CrossRef]
- Guo, H.; Kommidi, H.; Vedvyas, Y.; McCloskey, J.E.; Zhang, W.; Chen, N.; Nurili, F.; Wu, A.P.; Sayman, H.B.; Akin, O.; et al. A Fluorescent, [18F]-Positron-Emitting Agent for Imaging Prostate-Specific Membrane Antigen Allows Genetic Reporting in Adoptively Transferred, Genetically Modified Cells. ACS Chem. Biol. 2019, 14, 1449–1459. [Google Scholar] [CrossRef]
- Al-Karmi, S.; Albu, S.A.; Vito, A.; Janzen, N.; Czorny, S.; Banevicius, L.; Nanao, M.; Zubieta, J.; Capretta, A.; Valliant, J.F. Preparation of an 18F-Labeled Hydrocyanine Dye as a Multimodal Probe for Reactive Oxygen Species. Chem. Eur. J. 2017, 23, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Priem, T.; Bouteiller, C.; Camporese, D.; Brune, X.; Hardouin, J.; Romieu, A.; Renard, P.-Y. A novel sulfonated prosthetic group for [18F]-radiolabelling and imparting water solubility of biomolecules and cyanine fluorophores. Org. Biomol. Chem. 2012, 11, 469–479. [Google Scholar] [CrossRef] [PubMed]
- Schwegmann, K.; Hohn, M.; Hermann, S.; Schäfers, M.; Riemann, B.; Haufe, G.; Wagner, S.; Breyholz, H.-J. Optimizing the Biodistribution of Radiofluorinated Barbiturate Tracers for Matrix Metalloproteinase Imaging by Introduction of Fluorescent Dyes as Pharmacokinetic Modulators. Bioconjugate Chem. 2020, 31, 1117–1132. [Google Scholar] [CrossRef] [PubMed]
- Priyadarsini, K.I. Photophysics, photochemistry and photobiology of curcumin: Studies from organic solutions, bio-mimetics and living cells. J. Photochem. Photobiol. C: Photochem. Rev. 2009, 10, 81–95. [Google Scholar] [CrossRef]
- Anand, P.; Sundaram, C.; Jhurani, S.; Kunnumakkara, A.B.; Aggarwal, B.B. Curcumin and cancer: An “old-age” disease with an “age-old” solution. Cancer Lett. 2008, 267, 133–164. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Du, Z.-Y.; Zheng, X.; Li, D.-L.; Zhou, R.-P.; Zhang, K. Use of curcumin in diagnosis, prevention, and treatment of Alzheimer’s disease. Neural Regen. Res. 2018, 13, 742. [Google Scholar] [CrossRef]
- Chen, P.-Z.; Niu, L.-Y.; Chen, Y.-Z.; Yang, Q.-Z. Difluoroboron β-diketonate dyes: Spectroscopic properties and applications. Coord. Chem. Rev. 2017, 350, 196–216. [Google Scholar] [CrossRef]
- Ran, C.; Xu, X.; Raymond, S.B.; Ferrara, B.J.; Neal, K.; Bacskai, B.J.; Medarova, Z.; Moore, A. Design, Synthesis, and Testing of Difluoroboron-Derivatized Curcumins as Near-Infrared Probes for in Vivo Detection of Amyloid-β Deposits. J. Am. Chem. Soc. 2009, 131, 15257–15261. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, S.; Chakravarty, A.R. Metal Complexes of Curcumin for Cellular Imaging, Targeting, and Photoinduced Anticancer Activity. Acc. Chem. Res. 2015, 48, 2075–2083. [Google Scholar] [CrossRef]
- Ryu, E.K.; Choe, Y.S.; Lee, K.-H.; Choi, Y.; Kim, B.-T. Curcumin and Dehydrozingerone Derivatives: Synthesis, Radiolabeling, and Evaluation for β-Amyloid Plaque Imaging. J. Med. Chem. 2006, 49, 6111–6119. [Google Scholar] [CrossRef]
- Lee, I.; Yang, J.; Lee, J.H.; Choe, Y.S. Synthesis and evaluation of 1-(4-[18F]fluoroethyl)-7-(4′-methyl)curcumin with improved brain permeability for β-amyloid plaque imaging. Bioorganic Med. Chem. Lett. 2011, 21, 5765–5769. [Google Scholar] [CrossRef] [PubMed]
- Rokka, J.; Snellman, A.; Zona, C.; La Ferla, B.; Nicotra, F.; Salmona, M.; Forloni, G.; Haaparanta-Solin, M.; Rinne, J.O.; Solin, O. Synthesis and evaluation of a 18F-curcumin derivate for β-amyloid plaque imaging. Bioorganic Med. Chem. 2014, 22, 2753–2762. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.; Koo, H.-J.; Lee, I.; Choe, Y.S.; Choi, J.Y.; Lee, K.-H.; Kim, B.-T. Synthesis and characterization of 18F-labeled hydrazinocurcumin derivatives for tumor imaging. RSC Adv. 2015, 5, 96733–96745. [Google Scholar] [CrossRef]
- Kim, H.; Im, Y.H.; Ahn, J.; Yang, J.; Choi, J.Y.; Lee, K.-H.; Kim, B.-T.; Choe, Y.S. Synthesis and in vivo characterization of 18F-labeled difluoroboron-curcumin derivative for β-amyloid plaque imaging. Sci. Rep. 2019, 9, 6747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, J.; Cheng, R.; Fu, H.; Yang, J.; Kumar, M.; Lu, J.; Xu, Y.; Liang, S.H.; Cui, M.; Ran, C. Half-curcumin analogues as PET imaging probes for amyloid beta species. Chem. Commun. 2019, 55, 3630–3633. [Google Scholar] [CrossRef] [PubMed]
- Aras, O.; Ting, R.; An, F.; Chen, N. One-Step, Fast, 18F-19F Isotopic Exchange Radiolabeling of Difluoro-Dioxaborinins and Use of Such Compounds in Treatment. 2019. Available online: https://patentscope2.wipo.int/search/en/detail.jsf?docId=WO2019226962 (accessed on 2 April 2020).
- Hai-Bin, T.; Duan-Zhi, Y.; Lan, Z.; Li-Hua, W.; Chun-Fu, Z.; Ming-Wei, W.; Chun-Ying, W.; Gu-Cai, L.; Yong-Xian, W. Dopamine D4 receptor antagonist 3-(4-[18F]fluorobenzyl)-8-methoxy-1,2,3,4-tetrahydrochromeno[3,4-c]pyridin-5-one([18F]FMTP): Radiosynthesis and in vivo characterization in rats. Appl. Radiat. Isot. 2005, 63, 333–342. [Google Scholar] [CrossRef]
- Li, G.-C.; Yin, D.-Z.; Wang, M.-W.; Cheng, D.-F.; Wang, Y.-X. Syntheses of two potential dopamine D4 receptor radioligands: 18F labelled chromeno[3,4-c]pyridin-5-ones. Radiochim. Acta 2006, 94, 119–122. [Google Scholar] [CrossRef]
- Li, G.-C.; Yin, D.-Z.; Cheng, D.-F.; Zheng, M.-Q.; Han, Y.-J.; Cai, H.-C.; Xia, J.-Y.; Liang, S.; Xu, W.-B.; Wang, Y.-X. In vitro and in vivo evaluation of [18F]FHTP as a potential dopamine D4 receptor PET imaging agent. J. Radioanal. Nucl. Chem. 2009, 280, 15–20. [Google Scholar] [CrossRef]
- Pan, J.; Lau, J.; Mesak, F.; Hundal, N.; Pourghiasian, M.; Liu, Z.; Bénard, F.; Dedhar, S.; Supuran, C.T.; Lin, K.-S. Synthesis and evaluation of 18F-labeled carbonic anhydrase IX inhibitors for imaging with positron emission tomography. J. Enzym. Inhib. Med. Chem. 2014, 29, 249–255. [Google Scholar] [CrossRef]
- Cao, D.; Liu, Z.; Verwilst, P.; Koo, S.; Jangjili, P.; Kim, J.S.; Lin, W. Coumarin-Based Small-Molecule Fluorescent Chemosensors. Chem. Rev. 2019, 119, 10403–10519. [Google Scholar] [CrossRef]
- Ranyuk, E.; Ali, H.; Guérin, B.; van Lier, J.E. A new approach for the synthesis of 18F-radiolabelled phthalocyanines and porphyrins as potential bimodal/theranostic agents. J. Porphyr. Phthalocyanines 2013, 17, 850–856. [Google Scholar] [CrossRef]
- Simões, A.V.C.; Pinto, S.M.A.; Calvete, M.J.F.; Gomes, C.M.F.; Ferreira, N.C.; Castelo-Branco, M.; Llop, J.; Pereira, M.M.; Abrunhosa, A.J. Synthesis of a new 18F labeled porphyrin for potential application in positron emission tomography. In vivo imaging and cellular uptake. RSC Adv. 2015, 5, 99540–99546. [Google Scholar] [CrossRef]
- Entract, G.M.; Bryden, F.; Domarkas, J.; Savoie, H.; Allott, L.; Archibald, S.J.; Cawthorne, C.; Boyle, R.W. Development of PDT/PET Theranostics: Synthesis and Biological Evaluation of an 18F-Radiolabeled Water-Soluble Porphyrin. Mol. Pharm. 2015, 12, 4414–4423. [Google Scholar] [CrossRef] [PubMed]
- Kavali, R.R.; Lee, B.C.; Moon, B.S.; Yang, S.D.; Chun, K.S.; Choi, C.W.; Lee, C.-H.; Chi, D.Y. Efficient methods for the synthesis of 5-(4-[18F]fluorophenyl)-10,15,20-tris(3-methoxyphenyl)porphyrin as a potential imaging agent for tumor. J. Label Compd. Radiopharm. 2005, 48, 749–758. [Google Scholar] [CrossRef]
- Matsumura, K.; Ono, M.; Kimura, H.; Ueda, M.; Nakamoto, Y.; Togashi, K.; Okamoto, Y.; Ihara, M.; Takahashi, R.; Saji, H. 18F-Labeled Phenyldiazenyl Benzothiazole for in vivo Imaging of Neurofibrillary Tangles in Alzheimer’s Disease Brains. ACS Med. Chem. Lett. 2012, 3, 58–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X.; Jin, H.; Padakanti, P.K.; Li, J.; Yang, H.; Fan, J.; Mach, R.H.; Kotzbauer, P.; Tu, Z. Radiosynthesis and in vivo Evaluation of Two PET Radioligands for Imaging α-Synuclein. Appl. Sci. 2014, 4, 66–78. [Google Scholar] [CrossRef] [Green Version]
- Watanabe, H.; Ono, M.; Kimura, H.; Kagawa, S.; Nishii, R.; Fuchigami, T.; Haratake, M.; Nakayama, M.; Saji, H. A dual fluorinated and iodinated radiotracer for PET and SPECT imaging of β-amyloid plaques in the brain. Bioorganic Med. Chem. Lett. 2011, 21, 6519–6522. [Google Scholar] [CrossRef]
- Ono, M.; Watanabe, R.; Kawashima, H.; Cheng, Y.; Kimura, H.; Watanabe, H.; Haratake, M.; Saji, H.; Nakayama, M. Fluoro-pegylated Chalcones as Positron Emission Tomography Probes for in Vivo Imaging of β-Amyloid Plaques in Alzheimer’s Disease. J. Med. Chem. 2009, 52, 6394–6401. [Google Scholar] [CrossRef]
- Shimadzu, H.; Suemoto, T.; Suzuki, M.; Shiomitsu, T.; Okamura, N.; Kudo, Y.; Sawada, T. A novel probe for imaging amyloid-β: Synthesis of F-18 labelled BF-108, an Acridine Orange analog. J. Label. Compd. Radiopharm. 2003, 46, 765–772. [Google Scholar] [CrossRef]
- Price, T.W.; Firth, G.; Eling, C.J.; Kinnon, M.; Long, N.J.; Sturge, J.; Stasiuk, G.J. A 18F radiolabelled Zn(II) sensing fluorescent probe. Chem. Commun. 2018, 54, 3227–3230. [Google Scholar] [CrossRef]
- Prakash, G.K.S.; Alauddin, M.M.; Hu, J.; Conti, P.S.; Olah, G.A. Expedient synthesis of [18F]-labeled α-trifluoromethyl ketones. J. Label. Compd. Radiopharm. 2003, 46, 1087–1092. [Google Scholar] [CrossRef]
- Chu, W.; Chepetan, A.; Zhou, D.; Shoghi, K.I.; Xu, J.; Dugan, L.L.; Gropler, R.J.; Mintun, M.A.; Mach, R.H. Development of a PET radiotracer for non-invasive imaging of the reactive oxygen species, superoxide, in vivo. Org. Biomol. Chem. 2014, 12, 4421–4431. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Tong, X.; Lang, L.; Jacobson, O.; Yung, B.C.; Yang, X.; Bai, R.; Kiesewetter, D.O.; Ma, Y.; Wu, H.; et al. Quantification of Tumor Vascular Permeability and Blood Volume by Positron Emission Tomography. Theranostics 2017, 7, 2363–2376. [Google Scholar] [CrossRef] [PubMed]
- Heerdt, A.S. Lymphatic Mapping and Sentinel Lymph Node Biopsy or Breast Cancer. JAMA Oncol. 2018, 4, 431. [Google Scholar] [CrossRef]
- Stummer, W.; Pichlmeier, U.; Meinel, T.; Wiestler, O.D.; Zanella, F.; Reulen, H.-J. Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: A randomised controlled multicentre phase III trial. Lancet Oncol. 2006, 7, 392–401. [Google Scholar] [CrossRef]
- He, K.; Chi, C.; Li, D.; Zhang, J.; Niu, G.; Lv, F.; Wang, J.; Che, W.; Zhang, L.; Ji, N.; et al. Resection and survival data from a clinical trial of glioblastoma multiforme-specific IRDye800-BBN fluorescence-guided surgery. Bioeng. Transl. Med. 2020, e10182. [Google Scholar] [CrossRef]
- Jorns, J.M.; Visscher, D.; Sabel, M.; Breslin, T.; Healy, P.; Daignaut, S.; Myers, J.L.; Wu, A. Intraoperative frozen section analysis of margins in breast conserving surgery significantly decreases reoperative rates: One year experience at an ambulatory surgical center. Am. J. Clin. Pathol. 2012, 138, 657–669. [Google Scholar] [CrossRef] [Green Version]
- Klein, R.; Celiker-Guler, E.; Rotstein, B.H.; deKemp, R.A. PET and SPECT Tracers for Myocardial Perfusion Imaging. Semin. Nucl. Med. 2020, 50, 208–218. [Google Scholar] [CrossRef]
- Cowan, D.B.; Yao, R.; Akurathi, V.; Snay, E.R.; Thedsanamoorthy, J.K.; Zurakowski, D.; Ericsson, M.; Friehs, I.; Wu, Y.; Levitsky, S.; et al. Intracoronary Delivery of Mitochondria to the Ischemic Heart for Cardioprotection. PLoS ONE 2016, 11, e0160889. [Google Scholar] [CrossRef] [Green Version]
- Taggart, D.P.; Choudhary, B.; Anastasiadis, K.; Abu-Omar, Y.; Balacumaraswami, L.; Pigott, D.W. Preliminary experience with a novel intraoperative fluorescence imaging technique to evaluate the patency of bypass grafts in total arterial revascularization. Ann. Thorac. Surg. 2003, 75, 870–873. [Google Scholar] [CrossRef]
- Verjans, J.W.; Osborn, E.A.; Ughi, G.J.; Calfon Press, M.A.; Hamidi, E.; Antoniadis, A.P.; Papafaklis, M.I.; Conrad, M.F.; Libby, P.; Stone, P.H.; et al. Targeted Near-Infrared Fluorescence Imaging of Atherosclerosis. JACC Cardiovasc. Imaging 2016, 9, 1087–1095. [Google Scholar] [CrossRef] [PubMed]
- Christian, D.; Sabine, W.; Detlef, R.; Andre, I.; Lars, B.; Eckart, T.; Karl, W.; Hermann, R.; Bruno, R. Fluorescent Cardiac Imaging. Circulation 2007, 116, 1007–1014. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; An, F.-F.; Chan, M.; Friedman, B.; Rodriguez, E.A.; Tsien, R.Y.; Aras, O.; Ting, R. 18F-positron-emitting/fluorescent labeled erythrocytes allow imaging of internal hemorrhage in a murine intracranial hemorrhage model. J. Cereb. Blood Flow Metab. 2017, 37, 776–786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paulus, A.; Drude, N.; Nascimento, E.B.M.; Buhl, E.M.; Berbée, J.F.P.; Rensen, P.C.N.; van Marken Lichtenbelt, W.D.; Mottaghy, F.M.; Bauwens, M. [18F]BODIPY-triglyceride-containing chylomicron-like particles as an imaging agent for brown adipose tissue in vivo. Sci. Rep. 2019, 9, 2706. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, M.; Chansaenpak, K.; Liu, Y.; Yuan, H.; Xie, J.; Yin, H.; Branca, R.T.; Li, Z.; Wu, Z. A Novel PET Probe for Brown Adipose Tissue Imaging in Rodents. Mol. Imaging Biol. 2019. [Google Scholar] [CrossRef] [PubMed]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Munch, M.; Rotstein, B.H.; Ulrich, G. Fluorine-18-Labeled Fluorescent Dyes for Dual-Mode Molecular Imaging. Molecules 2020, 25, 6042. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules25246042
Munch M, Rotstein BH, Ulrich G. Fluorine-18-Labeled Fluorescent Dyes for Dual-Mode Molecular Imaging. Molecules. 2020; 25(24):6042. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules25246042
Chicago/Turabian StyleMunch, Maxime, Benjamin H. Rotstein, and Gilles Ulrich. 2020. "Fluorine-18-Labeled Fluorescent Dyes for Dual-Mode Molecular Imaging" Molecules 25, no. 24: 6042. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules25246042