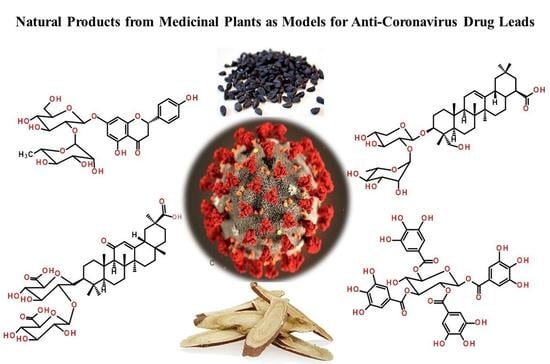
Natural Products from Medicinal Plants with Anti-Human Coronavirus Activities
Abstract
:1. Introduction
2. Medicinal Plants with Anti-HCoV Properties
3. Plant Secondary Metabolites with Anti-HCoV Properties
3.1. Alkaloids
3.2. Anthraquinones
3.3. Flavonoids and Flavonoid Glycosides
3.4. Lignans and Neolignans
3.5. Gallic Acid Derivatives
3.6. Terpenoids
3.6.1. Monoterpenoids
3.6.2. Sesquiterpenoids
3.6.3. Diterpenoids
3.6.4. Triterpenoids
3.6.5. Saponins
4. Future Perspectives and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV); The World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Morse, J.S.; Lalonde, T.; Xu, S.; Liu, W.R. Learning from the past: Possible urgent prevention and treatment options for severe acute respiratory infections caused by 2019-nCoV. Chembiochem 2020, 21, 730–738. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.M.; Wang, W.; Song, Z.G.; Hu, Y.; Tao, Z.W.; Tian, J.H.; Pei, Y.Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Geller, C.; Varbanov, M.; Duval, R.E. Human coronaviruses: Insights into environmental resistance and its influence on the development of new antiseptic strategies. Viruses 2012, 4, 3044–3068. [Google Scholar] [CrossRef] [Green Version]
- Macnaughton, M.R. Occurrence and frequency of coronavirus infections in humans as determined by enzyme-linked immunosorbent assay. Infect. Immun. 1982, 38, 419–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.; Penninger, J.M.; Li, Y.; Zhong, N.; Slutsky, A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020, 46, 586–590. [Google Scholar] [CrossRef] [Green Version]
- Kuhn, J.H.; Radoshitzky, S.R.; Li, W.; Wong, S.K.; Choe, H.; Farzan, M. The SARS Coronavirus receptor ACE2 A potential target for antiviral therapy. In New Concepts of Antiviral Therapy; Holzenburg, A., Bogner, E., Eds.; Springer: Boston, MA, USA, 2006; pp. 397–418. [Google Scholar] [CrossRef]
- Gheblawi, M.; Wang, K.; Viveiros, A.; Nguyen, Q.; Zhong, J.C.; Turner, A.J.; Raizada, M.K.; Grant, M.B.; Oudit, G.Y. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: Celebrating the 20th anniversary of the discovery of ACE2. Circ. Res. 2020, 126, 1456–1474. [Google Scholar] [CrossRef] [PubMed]
- Liang, P.H. Characterization and inhibition of SARS-coronavirus main protease. Curr. Top. Med. Chem. 2006, 6, 361–376. [Google Scholar] [CrossRef] [PubMed]
- Thiel, V.; Ivanov, K.A.; Putics, A.; Hertzig, T.; Schelle, B.; Bayer, S.; Weiβbrich, B.; Snijder, E.J.; Rabenau, H.; Doerr, H.W.; et al. Mechanisms and enzymes involved in SARS coronavirus genome expression. J. Gen. Virol. 2003, 84, 2305–2315. [Google Scholar] [CrossRef] [PubMed]
- Ziebuhr, J.; Snijder, E.J.; Gorbalenya, A.E. Virus-encoded proteinases and proteolytic processing in the Nidovirales. J. Gen. Virol. 2000, 81, 853–879. [Google Scholar] [CrossRef]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Cinatl, J.; Morgenstern, B.; Bauer, G.; Chandra, P.; Rabenau, H.; Doerr, H.W. Treatment of SARS with human interferons. Lancet 2003, 362, 293–294. [Google Scholar] [CrossRef]
- Bonam, S.R.; Kotla, N.G.; Bohara, R.A.; Rochev, Y.; Webster, T.J.; Bayry, J. Potential immuno-nanomedicine strategies to fight COVID-19 like pulmonary infections. Nano Today 2021, 36, 101051. [Google Scholar] [CrossRef]
- Bonam, S.R.; Kaveri, S.V.; Sakuntabhai, A.; Gilardin, L.; Bayry, J. Adjunct immunotherapies for the management of severely Ill COVID-19 patients. Cell Rep. Med. 2020, 1, 100016. [Google Scholar] [CrossRef] [PubMed]
- Hensel, A.; Bauer, R.; Heinrich, M.; Spiegler, V.; Kayser, O.; Hempel, G.; Kraft, K. Challenges at the time of COVID-19: Opportunities and innovations in antivirals from nature. Planta Med. 2020, 86, 659–664. [Google Scholar] [CrossRef]
- Kumar, V.; Jung, Y.S.; Liang, P.H. Anti-SARS coronavirus agents: A patent review (2008–Present). Expert Opin. Ther. Pat. 2013, 23, 1337–1348. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.J.; Michaelis, M.; Hsu, H.K.; Tsai, C.C.; Yang, K.D.; Wu, Y.C.; Cinatl Jr, J.; Doerr, H.W. Toona sinensis Roem tender leaf extract inhibits SARS coronavirus replication. J. Ethnopharmacol. 2008, 120, 108–111. [Google Scholar] [CrossRef]
- Kim, H.Y.; Shin, H.S.; Park, H.; Kim, Y.C.; Yun, Y.G.; Park, S.; Shin, H.J.; Kim, K. In vitro inhibition of coronavirus replications by the traditionally used medicinal herbal extracts, Cimicifuga rhizoma, Meliae cortex, Coptidis rhizoma, and Phellodendron cortex. J. Clin. Virol. 2008, 41, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Pharmacopoeia of the People’s Republic of China; People’s Medical Publishing House: Beijing, China, 2005; Volume 1, ISBN 978-7-11-706982-3.
- Lau, K.M.; Lee, K.M.; Koon, C.M.; Cheung, C.S.F.; Lau, C.P.; Ho, H.M.; Lee, M.Y.H.; Au, S.W.N.; Cheng, C.H.K.; Bik-San Lau, C.; et al. Immunomodulatory and anti-SARS activities of Houttuynia cordata. J. Ethnopharmacol. 2008, 118, 79–85. [Google Scholar] [CrossRef]
- Lu, H.; Liang, Y.; Yi, L.; Wu, X. Anti-inflammatory effect of Houttuynia cordata injection. J. Ethnopharmacol. 2006, 104, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Li, S.Y.; Chen, C.; Zhang, H.Q.; Guo, H.Y.; Wang, H.; Wang, L.; Zhang, X.; Hua, S.N.; Yu, J.; Xiao, P.G.; et al. Identification of natural compounds with antiviral activities against SARS-associated coronavirus. Antivir. Res. 2005, 67, 18–23. [Google Scholar] [CrossRef]
- Pleschka, S.; Stein, M.; Schoop, R.; Hudson, J.B. Anti-viral properties and mode of action of standardized Echinacea purpurea extract against highly pathogenic avian influenza virus (H5N1, H7N7) and swine-origin H1N1 (S-OIV). Virol. J. 2009, 6, 197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Signer, J.; Jonsdottir, H.R.; Albrich, W.C.; Strasser, M.; Züst, R.; Ryter, S.; Ackermann-Gaumann, R.; Lenz, N.; Siegrist, D.; Suter, A.; et al. In vitro antiviral activity of Echinaforce®, an Echinacea purpurea preparation, against coronaviruses, including common cold coronavirus 229E and SARS-CoV-2. Virol. J. 2020, 17, 136. [Google Scholar] [CrossRef] [PubMed]
- Ulasli, M.; Gurses, S.A.; Bayraktar, R.; Yumrutas, O.; Oztuzcu, S.; Igci, M.; Igci, Y.Z.; Cakmak, E.A.; Arslan, A. The effects of Nigella sativa (Ns), Anthemis hyalina (Ah) and Citrus sinensis (Cs) extracts on the replication of coronavirus and the expression of TRP genes family. Mol. Biol. Rep. 2014, 41, 1703–1711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, C.H.; Hwang, K.C.; Chao, C.L.; Chang, S.G.; Ho, M.S.; Lin, J.G.; Chang, H.H.; Kao, S.T.; Chen, Y.M.; Chou, P. An evaluation of the additive effect of natural herbal medicine on SARS or SARS-like infectious diseases in 2003: A randomized, double-blind, and controlled pilot study. Evid. Based Complement. Alternat. Med. 2008, 5, 355–362. [Google Scholar] [CrossRef] [Green Version]
- Sultan, M.T.; Buttxs, M.S.; Qayyum, M.M.N.; Suleria, H.A.R. Immunity: Plants as effective mediators. Crit. Rev. Food Sci. Nutr. 2014, 54, 1298–1308. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Wang, C.Z.; Hesse-Fong, J.; Lin, J.G.; Yuan, C.S. Application of Chinese medicine in acute and critical medical conditions. Am. J. Chin. Med. 2019, 47, 1223–1235. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.E.; Min, J.S.; Jang, M.S.; Lee, J.Y.; Shin, Y.S.; Park, C.M.; Song, J.H.; Kim, H.R.; Kim, S.; Jin, Y.H.; et al. Natural bis-benzylisoquinoline alkaloids-tetrandrine, fangchinoline, and cepharanthine, inhibit human coronavirus OC43 infection of MRC-5 human lung cells. Biomolecules 2019, 9, 696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, C.Y.; Jan, J.T.; Ma, S.H.; Kuo, C.J.; Juan, H.F.; Cheng, Y.S.E.; Hsu, H.H.; Huang, H.C.; Wu, D.; Brik, A.; et al. Small molecules targeting severe acute respiratory syndrome human coronavirus. Proc. Natl. Acad. Sci. USA 2004, 101, 10012–10017. [Google Scholar] [CrossRef] [Green Version]
- Ho, T.Y.; Wu, S.L.; Chen, J.C.; Li, C.C.; Hsiang, C.Y. Emodin blocks the SARS coronavirus spike protein and angiotensin-converting enzyme 2 interaction. Antivir. Res. 2007, 74, 92–101. [Google Scholar] [CrossRef]
- Deng, Y.; Aluko, R.; Jin, Q.; Zhang, Y.; Yuan, L. Inhibitory activities of baicalin against renin and angiotensin-converting enzyme. Pharm. Biol. 2012, 50, 401–406. [Google Scholar] [CrossRef]
- Cho, J.K.; Curtis-Long, M.J.; Lee, K.H.; Kim, D.W.; Ryu, H.W.; Yuk, H.J.; Park, K.H. Geranylated flavonoids displaying SARS-CoV papain-like protease inhibition from the fruits of Paulownia tomentosa. Bioorg. Med. Chem. 2013, 21, 3051–3057. [Google Scholar] [CrossRef] [PubMed]
- Ryu, Y.B.; Jeong, H.J.; Kim, J.H.; Kim, Y.M.; Park, J.Y.; Kim, D.; Naguyen, T.T.H.; Park, S.J.; Chang, J.S.; Park, K.H.; et al. Biflavonoids from Torreya nucifera displaying SARS-CoV 3CLpro inhibition. Bioorg. Med. Chem. 2010, 18, 7940–7947. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.C.; Kuo, Y.H.; Jan, J.T.; Liang, P.H.; Wang, S.Y.; Liu, H.G.; Lee, C.K.; Chang, S.T.; Kuo, C.J.; Lee, S.S.; et al. Specific plant terpenoids and lignoids possess potent antiviral activities against severe acute respiratory syndrome coronavirus. J. Med. Chem. 2007, 50, 4087–4095. [Google Scholar] [CrossRef] [Green Version]
- Xi, S.; Li, Y.; Yue, L.Y.; Gong, Y.; Qian, L.; Liang, T.; Ye, Y. Role of traditional chinese medicine in the management of viral pneumonia. Front. Pharmacol. 2020, 11, 1599. [Google Scholar] [CrossRef] [PubMed]
- Loizzo, M.R.; Saab, A.M.; Tundis, R.; Statti, G.A.; Menichini, F.; Lampronti, I.; Gambari, R.; Cinatl, J., Jr.; Doerr, H.W. Phytochemical analysis and in vitro antiviral activities of the essential oils of seven Lebanon species. Chem. Biodivers. 2008, 5, 461–470. [Google Scholar] [CrossRef]
- Chang, F.R.; Yen, C.T.; El-Shazly, M.; Lin, W.H.; Yen, M.H.; Lin, K.H.; Wu, Y.C. Anti-human coronavirus (anti-HCoV) triterpenoids from the leaves of Euphorbia neriifolia. Nat. Prod. Commun. 2012, 7, 1415–1417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cinatl, J.; Morgenstern, B.; Bauer, G.; Chandra, P.; Rabenau, H.; Doerr, H. Glycyrrhizin, an active component of liquorice roots, and replication of SARS-associated coronavirus. Lancet 2003, 361, 2045–2046. [Google Scholar] [CrossRef] [Green Version]
- Ito, M.; Nakashima, H.; Baba, M.; Pauwels, R.; De Clercq, E.; Shigeta, S.; Yamamoto, N. Inhibitory effect of glycyrrhizin on the in vitro infectivity and cytopathic activity of the human immunodeficiency virus [HIV (HTLV-III/LAV)]. Antivir. Res. 1987, 7, 127–137. [Google Scholar] [CrossRef]
- Amoros, M.; Fauconnier, B.; Girre, R. In vitro antiviral activity of a saponin from Anagallis arvensis, Primulaceae, against herpes simplex virus and poliovirus. Antivir. Res. 1987, 8, 13–25. [Google Scholar] [CrossRef]
- Baba, M.; Shigeta, S. Antiviral activity of glycyrrhizin against varicella-zoster virus in vitro. Antivir. Res. 1987, 7, 99–107. [Google Scholar] [CrossRef]
- Ushio, Y.; Abe, H. Inactivation of measles virus and herpes simplex virus by saikosaponin d. Planta Med. 1992, 58, 171–173. [Google Scholar] [CrossRef]
- Schwarz, S.; Wang, K.; Yu, W.; Sun, B.; Schwarz, W. Emodin inhibits current through SARS-associated coronavirus 3a protein. Antivir. Res. 2011, 90, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Xie, S.; Sun, B. Viral proteins function as ion channels. BBA Biomembr. 2011, 1808, 510–515. [Google Scholar] [CrossRef]
- Lin, C.W.; Tsai, F.J.; Tsai, C.H.; Lai, C.C.; Wan, L.; Ho, T.Y.; Hsieh, C.C.; Chao, P.D.L. Anti-SARS coronavirus 3C-like protease effects of Isatis indigotica root and plant-derived phenolic compounds. Antivir. Res. 2005, 68, 36–42. [Google Scholar] [CrossRef]
- Chen, F.; Chan, K.H.; Jiang, Y.; Kao, R.Y.T.; Lu, H.T.; Fan, K.W.; Cheng, V.C.C.; Tsui, W.H.W.; Huang, I.F.N.; Lee, T.S.W. In vitro susceptibility of 10 clinical isolates of SARS coronavirus to selected antiviral compounds. J. Clin. Virol. 2004, 31, 69–75. [Google Scholar] [CrossRef]
- Wang, W.; Ma, X.; Han, J.; Zhou, M.; Ren, H.; Pan, Q.; Zheng, C.; Zheng, Q. Neuroprotective effect of scutellarin on ischemic cerebral injury by down-regulating the expression of angiotensin-converting enzyme and AT1 receptor. PLoS ONE 2016, 11. [Google Scholar] [CrossRef]
- Ghosh, A.K.; Xi, K.; Johnson, M.E.; Baker, S.C.; Mesecar, A.D. Progress in anti-SARS coronavirus chemistry, biology and chemotherapy. Annu. Rep. Med. Chem. 2006, 41, 183–196. [Google Scholar] [CrossRef]
- Yu, M.S.; Lee, J.; Lee, J.M.; Kim, Y.; Chin, Y.W.; Jee, J.G.; Keum, Y.S.; Jeong, Y.J. Identification of myricetin and scutellarein as novel chemical inhibitors of the SARS coronavirus helicase, nsP13. Bioorg. Med. Chem. Lett. 2012, 22, 4049–4054. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Bellavite, P.; Donzelli, A. Hesperidin and SARS-CoV-2: New light on the healthy function of citrus fruits. Antioxidants 2020, 9, 742. [Google Scholar] [CrossRef] [PubMed]
- Clementi, N.; Scagnolari, C.; D’Amore, A.; Palombi, F.; Criscuolo, E.; Frasca, F.; Pierangeli, A.; Mancini, N.; Antonelli, G.; Clementi, M.; et al. Naringenin is a powerful inhibitor of SARS-CoV-2 infection in vitro. Pharmacol. Res. 2020, 163, 105255. [Google Scholar] [CrossRef]
- Wu, C.; Liu, Y.; Yang, Y.; Zhang, P.; Zhong, W.; Wang, Y.; Wang, Q.; Xu, Y.; Li, M.; Li, X.; et al. Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods. Acta Pharm. Sin. B 2020, 10, 766–788. [Google Scholar] [CrossRef]
- Muchtaridi, M.; Fauzi, M.; Khairul Ikram, N.K.; Mohd Gazzali, A.; Wahab, H.A. Natural flavonoids as potential angiotensin-converting enzyme 2 inhibitors for anti-SARS-CoV-2. Molecules 2020, 25, 3980. [Google Scholar] [CrossRef]
- Jo, S.; Kim, S.; Shin, D.H.; Kim, M.S. Inhibition of SARS-CoV 3CL protease by flavonoids. J. Enzyme Inhib. Med. Chem. 2020, 35, 145–151. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.; Li, J.; Luo, C.; Liu, H.; Xu, W.; Chen, G.; Liew, O.W.; Zhu, W.; Puah, C.M.; Shen, X.; et al. Binding interaction of quercetin-3-β-galactoside and its synthetic derivatives with SARS-CoV 3CLpro: Structure–activity relationship studies reveal salient pharmacophore features. Bioorg. Med. Chem. 2006, 14, 8295–8306. [Google Scholar] [CrossRef]
- Schwarz, S.; Sauter, D.; Wang, K.; Zhang, R.; Sun, B.; Karioti, A.; Bilia, A.R.; Efferth, T.; Schwarz, W. Kaempferol derivatives as antiviral drugs against the 3a channel protein of coronavirus. Planta Med. 2014, 80, 177–182. [Google Scholar] [CrossRef] [Green Version]
- Yi, L.; Li, Z.; Yuan, K.; Qu, X.; Chen, J.; Wang, G.; Zhang, H.; Luo, H.; Zhu, L.; Jiang, P.; et al. Small molecules blocking the entry of severe acute respiratory syndrome coronavirus into host cells. J. Virol. 2004, 78, 11334–11339. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.N.; Lin, C.P.; Huang, K.K.; Chen, W.C.; Hsieh, H.P.; Liang, P.H.; Hsu, J.T.A. Inhibition of SARS-CoV 3C-like protease activity by theaflavin-3, 3’-digallate (TF3). Evid. Based Complement. Alternat. Med. 2005, 2, 209–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumoto, Y.; Matsuura, T.; Aoyagi, H.; Matsuda, M.; Hmwe, S.S.; Date, T.; Watanabe, N.; Watashi, K.; Suzuki, R.; Ichinose, S.; et al. Antiviral activity of glycyrrhizin against hepatitis C virus in vitro. PLoS ONE 2013, 8, e68992. [Google Scholar] [CrossRef] [Green Version]
- Hoever, G.; Baltina, L.; Michaelis, M.; Kondratenko, R.; Baltina, L.; Tolstikov, G.A.; Doerr, H.W.; Cinatl Jr, J. Antiviral activity of glycyrrhizic acid derivatives against SARS−Coronavirus. J. Med. Chem. 2005, 48, 1256–1259. [Google Scholar] [CrossRef]
- Cheng, P.W.; Ng, L.T.; Chiang, L.C.; Lin, C.C. Antiviral effects of saikosaponins on human coronavirus 229E in vitro. Clin. Exp. Pharmacol. Physiol. 2006, 33, 612–616. [Google Scholar] [CrossRef]
- Mani, R.J.; Sehgal, N.; Dogra, N.; Saxena, S.; Katare, D.P. Deciphering underlying mechanism of Sars-CoV-2 infection in humans and revealing the therapeutic potential of bioactive constituents from Nigella sativa to combat COVID19: In-silico study. J. Biomol. Struct. Dyn. 2020, 1–13. [Google Scholar] [CrossRef]




















| Plant Name | Family | Part Used | Ref. |
|---|---|---|---|
| Toona sinensis Reom. | Meliaceae | Leaves | [18] |
| Cimicifuga racemosa (L.) Nutt. | Ranunculaceae | Rhizome | [19] |
| Melia azedarach L. | Meliaceae | Barks | |
| Coptis chinensis Franch. | Ranunculaceae | Rhizomes | |
| Phellodendron amurense Rupr. | Rutaceae | Barks | |
| Sophora subprostrata Chun & T.Chen. | Fabaceae | Seeds | |
| Paeonia suffruticosa Andrews | Paeoniaceae | Whole plant | |
| Houttuynia cordata Thunb. | Saururaceae | Aerial parts | [20] |
| Lycoris radiata Herb. | Amaryllidaceae | Stem cortex | [23] |
| Artemisia annua L. | Asteraceae | Whole plant | |
| Pyrrosia lingua (Thunb.) Farw. | Ploypodiaceae | Leaves | |
| Lindera aggregata (Sims) Kostem | Lauraceae | Roots | |
| Echinacea purpurea (L.) Moench | Asteraceae | Aerial parts | [24] |
| Anthemis hyalina DC. | Asteraceae | Flowers | [26] |
| Nigella sativa L. | Ranunculaceae | Seeds | |
| Citrus sinensis L. Osbeck | Rutaceae | Peels | |
| Astragalus mongholicus Bunge | Fabaceae | Leaves | [29] |
| Atractylodis macrocephalae Koidz. | Asteraceae | Rhizome | |
| Atractylodes lancea (Thunb.) DC. | Asteraceae | Rhizome | |
| Glycyrrhizae uralensis Fisch. Ex DC. | Fabaceae | Roots | |
| Saposhnikovia divaricata (Turcz. Ex Ledeb.) Schischk. | Apiaceae | Flowers | |
| Lonicerae japonica Thunb. | Capripoliaceae | Fruits | |
| Forsythia suspensa (Thunb.) Vahl | Oleaceae | Leaves | |
| Platycodon grandifiorus (Jacq.) A.DC. | Campanulaceae | Roots | |
| Agastache rugosa (Fich. & C.A.Mey.) Kuntze | Lamiaceae | Aerial parts | |
| Cyrtomium fortunei J. Sm. | Dryopteridaceae | Leaves | |
| Allium sativum L. fam. | Alliaceae | Bulbs | [28] |
| Camellia sinensis (L.) Kuntze | Theaceae | Leaves | |
| Zingiber officinalis | Zingiberaceae | Roots | |
| Hypericum perforatum L. | Hypericaceae | Aerial parts | |
| Scutellaria baicalensis Georgi. | Lamiaceae | Aerial parts | [27] |
| Bupleurum chinense DC. | Apiaceae | Aerial parts | |
| Gardenia jasminoides J. Ellis. | Rubiaceae | Leaves | |
| Stephania tetrandra S. Moore | Menispermaceae | Leaves | [30] |
| Rauwolfia spp. | Apocynaceae | - | [31] |
| Aesculus hippocastanum L. | Sapindaceae | Seeds | |
| Rheum officinale Baill. | Polygonaceae | Roots | [32] |
| Polygonum multiflorum Thunb. | Polygonaceae | Roots | |
| Scutellaria spp. | Lamiaceae | Aerial parts | [33] |
| Paulownia tomentosa (Thunb.) Steud. | Paulowniaceae | Fruits | [34] |
| Torreya nucifera L. Siebold & Zucc. | Lamiaceae | Leaves | [35] |
| Chamaecyparis obtusa var. formosana | Cupressaceae | Heartwood | [36] |
| Juniperus formosana Hayata. | Cupressaceae | Heartwood | |
| Cryptomeria japonica (L.f.) D.Don | Cupressaceae | Heartwood | |
| Rhus Chinensis Mill. | Anacardiaceae | Fruits | [37] |
| Laurus nobilis L. | Lauraceae | Berry | [38] |
| Thuja orientalis L. | Cupressaceae | Fruits | |
| Juniperus oxycedrus ssp. oxycedrus | Cupressaceae | Berry | |
| Euphorbia neriifolia L. | Euphorbiaceae | Leaves | [39] |
| Glycyrrhiza glabra L. | Fabaceae | Roots | [40] |
| Bupleurum spp. | Apiaceae | Aerial parts | [41,42,43,44] |
| Heteromorpha spp. | Apiaceae | Aerial parts | |
| Scrophularia scorodonia L. | Scrophulariaceae | Aerial parts |
| No. | Mode of Action | IC50 (μM) | CC50 (μM) | EC50 (μM) | SI | Concentration (μM) | Positive Control | Ref. |
|---|---|---|---|---|---|---|---|---|
| Alkaloids | ||||||||
| 7 | Inhibition of SARS-CoV (BJ-001 strain) | - | 14,980.0 ± 912.0 a | 15.7 ± 1.2 a | 954 | - | Interferon alpha, CC50 > 100,000 ± 710.1 μM, EC50 = 660.3 ± 119.1 μM, SI > 151 | [23] |
| 8 | Inhibition of HCoV-OC43 infected MRC-5 human lung cells | 0.33 ± 0.03 | 13.41 ± 0.36 | - | 40.19 | 2–20 | - | [30] |
| 9 | 1.01 ± 0.07 | 11.54 ± 0.46 | - | 11.46 | ||||
| 10 | 0.83 ± 0.07 | 11.26 ± 0.69 | - | 13.63 | ||||
| 11 | Inhibition of SARS-CoV replication | - | 25 | 3.4 | 7.3 | - | - | [31] |
| Anthraquinones | ||||||||
| 18 | Blocks the interaction of SARS spike protein to ACE-2 | 200 | - | - | - | 0.1–400 | Promazine | [32] |
| Flavonoids and flavonoid glycosides | ||||||||
| 19 | Inhibition of SARS-CoV 3CL Protease | 8.3 (2.5 ± 0.8 μg/mL) | 2718 (820 ± 15 μg/mL) | - | - | - | - | [47] |
| 22 | Inhibition of wild-type SARS-CoV infection | - | 155 | 10.6 (9.2–12.2) | 14.62 | 0.1–10,000 | Glycyrrhizin (111), EC50 > 607.6 μM; Ribavirin, not effect | [44,50] |
| 23 | Inhibition of entry of HIV-luc/SARS pseudotypeed virus into Vero E6 cells | - | 3320 | 83.4 | 39.81 | 0.1–10,000 | - | [60] |
| 24 | Inhibition of SARS-CoV helicase, nsP13 | 2.71 ± 0.19 | - | - | - | 0.01–10 | [51] | |
| 25 | 0.86 ± 0.48 | - | - | - | ||||
| 31 | Inhibition of SARS-CoV 3CL Protease | 33.17 | - | - | - | 2–320 | - | [57] |
| 32 | 27.45 | - | - | - | ||||
| 33 | 37.78 | - | - | - | ||||
| 36 | Inhibition of SARS-CoV 3CL Protease | 42.79 ± 4.97 | - | - | - | 9.4–80 | - | [58] |
| 38 | 24.14 ± 4.32 | - | - | - | ||||
| 39 | 31.62 ± 2.43 | - | - | - | ||||
| 40 | 48.85 ± 8.15 | - | - | - | ||||
| 41 | 61.46 ± 9.13 | - | - | - | ||||
| 36 | Inhibition of SARS-CoV 3CL Protease Q189A | 127.89 ± 10.06 | - | - | - | 16.5–200 | ||
| 45 | Inhibition of SARS-CoV papain-like protease | 6.2 ± 0.04 | - | - | - | 0.1–100 | - | [34] |
| 46 | 6.1 ± 0.02 | - | - | - | ||||
| 47 | 11.6 ± 0.13 | - | - | - | ||||
| 48 | 12.5 ± 0.22 | - | - | - | ||||
| 49 | 5.0 ± 0.06 | - | - | - | ||||
| 50 | 9.5 ± 0.10 | - | - | - | ||||
| 51 | 9.2 ± 0.13 | - | - | - | ||||
| 52 | 13.2 ± 0.14 | - | - | - | ||||
| 53 | 12.7 ± 0.19 | - | - | - | ||||
| 54 | 14.4 ± 0.27 | - | - | - | ||||
| 55 | 10.4 ± 0.16 | - | - | - | ||||
| 56 | 13.9 ± 0.18 | - | - | - | ||||
| 64 | Inhibition of SARS-CoV 3CL Protease | 280.8 ± 21.4 | - | - | - | 1–1000 | Luteolin (22), IC50 = 20.0 ± 2.2 μM; Quercetin (23), IC50 = 23.8 ± 1.9 μM | [35] |
| 65 | 8.3 ± 1.2 | - | - | - | ||||
| 66 | 72.3 ± 4.5 | - | - | - | ||||
| 67 | 32.0 ± 1.7 | - | - | - | ||||
| 68 | 34.8 ± 0.2 | - | - | - | ||||
| Lignans and neolignans | ||||||||
| 69 | Inhibition of Vero E6 cell proliferation and SARS-CoV replication | - | >750 | >10 | N.C. b | 0.01–10 | Niclosamide, CC50 = 22.1 μM, EC50 < 0.1 μM, SI > 221; Valinomycin, CC50 = 67.5 μM, EC50 = 1.63 μM, SI = 41.4 | [36] |
| 70 | - | >750 | 1.13 | >667 | ||||
| 72 | - | 88.9 | 6.50 | 13.7 | ||||
| 73 | - | 68.3 | 3.80 | 18.0 | ||||
| 69 | Inhibition of SARS-CoV 3CL Protease | >100 | - | - | - | 8–80 | Niclosamide, IC50 = 40 μM | |
| 70 | 25 | - | - | - | ||||
| Gallic acid derivatives | ||||||||
| 74 | Inhibition of wild-type SARS-CoV infection | - | 1.08 | 4.5 (1.96–5.8) | 240 | 0.1–10,000 | Glycyrrhizin (111), EC50 > 607.6 μM; Ribavirin, not effect | [60] |
| 75 | Inhibition of SARS-CoV 3CL Protease | 3 | - | - | - | 4–20 | N-Ethylmaleimide | [61] |
| 76 | 43 | - | - | - | ||||
| 77 | 9.5 | - | - | - | ||||
| Sesquiterpenoids | ||||||||
| 84 | Inhibition of Vero E6 cell proliferation and SARS-CoV replication | - | >750 | >10 | N.C. b | 0.01–10 | Niclosamide, CC50 = 22.1 μM, EC50 < 0.1 μM, SI > 221; Valinomycin, CC50 = 67.5 μM, EC50 = 1.63 μM, SI = 41.4 | [36] |
| 85 | - | 76.8 | 4.44 | 17.3 | ||||
| Diterpenoids | ||||||||
| 87 | Inhibition of Vero E6 cell proliferation and SARS-CoV replication | - | 80.4 | 1.39 | 58.0 | 0.01–10 | Niclosamide, CC50 = 22.1 μM, EC50 < 0.1 μM, SI > 221; Valinomycin, CC50 = 67.5 μM, EC50 = 1.63 μM, SI = 41.4 | [36] |
| 88 | - | 305.1 | 4.00 | 76.3 | ||||
| 90 | - | 78.5 | >10 | <7.9 | ||||
| 91 | - | >750 | 1.47 | >510 | ||||
| 92 | - | 127 | 1.15 | 111 | ||||
| 93 | - | 89.7 | 5.55 | 16.2 | ||||
| 94 | - | 303.3 | 1.57 | 193 | ||||
| 95 | - | >750 | 4.71 | >159 | ||||
| 96 | - | 674 | 7.5 | 89.8 | ||||
| 87 | Inhibition of SARS-CoV 3CL Protease | 49.6 ± 1.5 | - | - | - | 0.1–1000 | Abietic acid (104), IC50 = 189.1 ± 15.5 μM | [35] |
| 97 | 220.8 ± 10.4 | - | - | - | ||||
| 98 | 233.4 ± 22.2 | - | - | - | ||||
| 99 | 163.2 ± 13.8 | - | - | - | ||||
| 100 | 128.9 ± 25.2 | - | - | - | ||||
| 101 | 207.0 ± 14.3 | - | - | - | ||||
| 102 | 283.5 ± 18.4 | - | - | - | ||||
| 103 | 137.7 ± 12.5 | - | - | - | ||||
| Triterpenoids | ||||||||
| 105 | Inhibition of Vero E6 cell proliferation and SARS-CoV replication | - | 150 | >10 | <15 | - | Niclosamide, CC50 = 22.1 μM, EC50 < 0.1 μM, SI > 221; Valinomycin, CC50 = 67.5 μM, EC50 = 1.63 μM, SI = 41.4 | [36] |
| 106 | - | 112 | 0.63 | 180 | ||||
| 105 | Inhibition of SARS-CoV 3CL Protease | 10 | - | - | - | 8–80 | Niclosamide, IC50 = 40 μM | |
| 106 | >100 | - | - | - | ||||
| Saponins | ||||||||
| 111 | - | >20,000 * | 300 (51) * | >67 | - | - | [40] | |
| 112 | Inhibition of SARS-CoV replication | - | >3000 | 40 ± 13 | >75 | 0.1–1000 | Glycyrrhizin (111), CC50 > 24,000 μM, EC50 = 365. ± 12 μM, SI > 65 | [63] |
| 113 | - | 1462 ± 50 | 35 ± 7 | 41 | ||||
| 114 | - | 215 ± 18 | 139 ± 20 | 2 | ||||
| 120 | - | 44 ± 6 | 8 ± 2 | 6 | ||||
| 121 | - | 250 ± 19 | 50 ± 10 | 5 | ||||
| 122 | - | 15 ± 3 | 5 ± 3 | 3 | ||||
| 123 | - | 66 ± 8 | 16 ± 1 | 4 | ||||
| 127 | Inhibition of HCoV-OC43 infected MRC-5 human lung cells | - | 228.1 ± 3.8 | 8.6 ± 0.3 | 26.6 | 0.25–25 | Actinomycin D, CC50 = 2.8 ± 0.3 μM, EC50 = 0.02 ± 0.0 μM, SI = 140 | [64] |
| 128 | - | 383.3 ± 0.2 | 1.7 ± 0.1 ** | 221.9 | ||||
| 129 | - | 121.5 ± 0.1 | 19.9 ± 0.1 *† | 19.2 | ||||
| 130 | - | 176.2 ± 0.2 | 13.2 ± 0.3 *†‡ | 13.3 | ||||
| 131 | Inhibition of SARS-CoV replication | - | 15.0 | 6.0 | 2.5 | - | - | [30] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hafez Ghoran, S.; El-Shazly, M.; Sekeroglu, N.; Kijjoa, A. Natural Products from Medicinal Plants with Anti-Human Coronavirus Activities. Molecules 2021, 26, 1754. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules26061754
Hafez Ghoran S, El-Shazly M, Sekeroglu N, Kijjoa A. Natural Products from Medicinal Plants with Anti-Human Coronavirus Activities. Molecules. 2021; 26(6):1754. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules26061754
Chicago/Turabian StyleHafez Ghoran, Salar, Mohamed El-Shazly, Nazim Sekeroglu, and Anake Kijjoa. 2021. "Natural Products from Medicinal Plants with Anti-Human Coronavirus Activities" Molecules 26, no. 6: 1754. https://0-doi-org.brum.beds.ac.uk/10.3390/molecules26061754