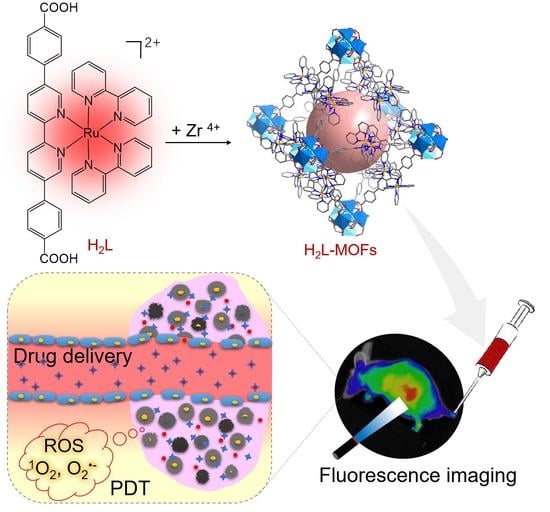
Single Nano-Sized Metal–Organic Framework for Bio-Nanoarchitectonics with In Vivo Fluorescence Imaging and Chemo-Photodynamic Therapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Characterized Techniques
2.3. Cell Lines Culture and Animal Experiments
2.4. Preparation of H2L-MOFs
2.5. DOX Uptake Experiment
2.6. DOX Release Experiment
2.7. In Vitro Singlet Oxygen Generation
2.8. Cytotoxicity and In Vitro Chemotherapy, Photodynamic Therapy, and Chemo-Photodynamic Therapy of H2L-MOFs
2.9. In Vivo Fluorescence Imaging
3. Results
3.1. Synthesis and Characterization of H2L-MOFs
3.2. Optical Properties of H2L-MOFs
3.3. Drug Loading and Releasing of H2L-MOFs
3.4. Biocompatibility of H2L-MOFs
3.5. In Vitro Treatment of H2L-MOFs
3.6. In Vivo Fluorescence Imaging of H2L-MOFs
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shah, S.C.; Kayamba, V.; Peek, R.M., Jr.; Heimburger, D. Cancer control in low-and middle-income countries: Is it time to consider screening? J. Glob. Oncol. 2019, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hauer-Jensen, M.; Denham, J.W.; Andreyev, H.J.N. Radiation enteropathy—Pathogenesis, treatment and prevention. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 470–479. [Google Scholar] [CrossRef] [PubMed]
- Szczesniak, M.M.; Maclean, J.; Zhang, T.; Graham, P.H.; Cook, I.J. Persistent dysphagia after head and neck radiotherapy: A common and under-reported complication with significant effect on non-cancer-related mortality. Clin. Oncol. 2014, 26, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Wang, Y.M.; Li, Y.H.; Cai, S.J.; Yin, X.B.; He, X.W.; Zhang, Y.K. Fluorescent Imaging-Guided Chemotherapy-and-Photodynamic Dual Therapy with Nanoscale Porphyrin Metal-Organic Framework. Small 2017, 13, 1603459. [Google Scholar] [CrossRef]
- Zheng, X.; Wu, W.; Zheng, Y.; Ding, Y.; Xiang, Y.; Liu, B.; Tong, A. Organic Nanoparticles with Persistent Luminescence for In Vivo Afterglow Imaging-Guided Photodynamic Therapy. Chemistry 2021, 27, 6911–6916. [Google Scholar] [CrossRef]
- Wei, Q.; Chen, Y.; Ma, X.; Ji, J.; Qiao, Y.; Zhou, B.; Ma, F.; Ling, D.; Zhang, H.; Tian, M.; et al. High-Efficient Clearable Nanoparticles for Multi-Modal Imaging and Image-Guided Cancer Therapy. Adv. Funct. Mater. 2018, 28, 1704634. [Google Scholar] [CrossRef]
- Yu, W.; Yu, N.; Wang, Z.; Li, X.; Song, C.; Jiang, R.; Geng, P.; Li, M.; Yin, S.; Chen, Z. Chitosan-mediated green synthesis and folic-acid modification of CuS quantum dots for photoacoustic imaging guided photothermal therapy of tumor. J. Colloid Interface Sci. 2019, 555, 480–488. [Google Scholar] [CrossRef]
- William, J.; Rieter, K.M.L.T.; Lin, W. Surface Modification and Functionalization of Nanoscale Metal-Organic Frameworks for Controlled Release and Luminescence Sensing. J. Am. Chem. Soc. 2007, 129, 9852–9853. [Google Scholar]
- Yin, H.-Q.; Cao, P.-P.; Wang, X.-Y.; Li, Y.-H.; Yin, X.-B. Computed Tomography Imaging-Guided Tandem Catalysis-Enhanced Photodynamic Therapy with Gold Nanoparticle Functional Covalent Organic Polymers. ACS Appl. Bio Mater. 2020, 3, 2534–2542. [Google Scholar] [CrossRef]
- Zhang, D.; Gao, A.; Xu, Y.; Yin, X.B.; He, X.W.; Zhang, Y.K. Gd-Al co-doped mesoporous silica nanoparticles loaded with Ru(bpy)(3)(2)(+) as a dual-modality probe for fluorescence and magnetic resonance imaging. Analyst 2014, 139, 4613–4619. [Google Scholar] [CrossRef]
- Wang, J.; Gao, Y.; Liu, P.; Xu, S.; Luo, X. Core-Shell Multifunctional Nanomaterial-Based All-in-One Nanoplatform for Simultaneous Multilayer Imaging of Dual Types of Tumor Biomarkers and Photothermal Therapy. Anal. Chem. 2020, 92, 15169–15178. [Google Scholar] [CrossRef]
- Minati, L.; Antonini, V.; Dalla Serra, M.; Speranza, G.; Enrichi, F.; Riello, P. pH-activated doxorubicin release from polyelectrolyte complex layer coated mesoporous silica nanoparticles. Microporous Mesoporous Mater. 2013, 180, 86–91. [Google Scholar] [CrossRef]
- Chen, W.; Zeng, K.; Liu, H.; Ouyang, J.; Wang, L.; Liu, Y.; Wang, H.; Deng, L.; Liu, Y.N. Cell membrane camouflaged hollow prussian blue nanoparticles for synergistic photothermal-/chemotherapy of cancer. Adv. Funct. 2017, 27, 1605795. [Google Scholar] [CrossRef]
- Lin, X.; Fang, Y.; Tao, Z.; Gao, X.; Wang, T.; Zhao, M.; Wang, S.; Liu, Y. Tumor-Microenvironment-Induced All-in-One Nanoplatform for Multimodal Imaging-Guided Chemical and Photothermal Therapy of Cancer. ACS Appl. Mater. Interfaces 2019, 11, 25043–25053. [Google Scholar] [CrossRef]
- Furukawa, H.; Cordova, K.E.; O’Keeffe, M.; Yaghi, O.M. The Chemistry and Applications of Metal-Organic Frameworks. Science 2013, 341, 1230444. [Google Scholar] [CrossRef] [Green Version]
- Kirchon, A.; Feng, L.; Drake, H.F.; Joseph, E.A.; Zhou, H.C. From fundamentals to applications: A toolbox for robust and multifunctional MOF materials. Chem. Soc. Rev. 2018, 47, 8611–8638. [Google Scholar] [CrossRef]
- Zhou, H.-C.; Kitagaw, S. Metal–Organic Frameworks (MOFs). Chem. Soc. Rev. 2014, 43, 5415. [Google Scholar] [CrossRef] [Green Version]
- Jiang, Z.; Xu, X.; Ma, Y.; Cho, H.S.; Ding, D.; Wang, C.; Wu, J.; Oleynikov, P.; Jia, M.; Cheng, J.; et al. Filling metal-organic framework mesopores with TiO2 for CO2 photoreduction. Nature 2020, 586, 549–554. [Google Scholar] [CrossRef]
- Wang, Q.; Astruc, D. State of the art and prospects in metal–organic framework (MOF)-based and MOF-derived nanocatalysis. Chem. Rev. 2019, 120, 1438–1511. [Google Scholar] [CrossRef]
- Mohamed Eddaoudi, J.K.; Rosi, N.; Vodak, D.; Wachter, J.; O’Keeffe, M.; Omar, M.; Yaghi, O.M. Systematic Design of Pore Size and Functionality in Isoreticular MOFs and Their Application in Methane Storage. Science 2002, 295, 469. [Google Scholar] [CrossRef] [Green Version]
- Cao, Y.; Wang, L.; Shen, C.; Wang, C.; Hu, X.; Wang, G. An electrochemical sensor on the hierarchically porous Cu-BTC MOF platform for glyphosate determination. Sens. Actuators B 2019, 283, 487–494. [Google Scholar] [CrossRef]
- Wang, Y.M.; Xu, Y.; Yang, Z.R.; Zhang, X.; Hu, Y.; Yang, R. Multi-functional lanthanide coordination polymers for multi-modal detection of nitroaromatics and trace water in organic solvents. J. Colloid Interface Sci. 2021, 598, 474–482. [Google Scholar] [CrossRef]
- Ni, K.; Lan, G.; Veroneau, S.S.; Duan, X.; Song, Y.; Lin, W. Nanoscale metal-organic frameworks for mitochondria-targeted radiotherapy-radiodynamic therapy. Nat. Commun. 2018, 9, 4321. [Google Scholar] [CrossRef]
- Lu, K.; Aung, T.; Guo, N.; Weichselbaum, R.; Lin, W. Nanoscale Metal-Organic Frameworks for Therapeutic, Imaging, and Sensing Applications. Adv. Mater. 2018, 30, 1707634. [Google Scholar] [CrossRef]
- Wang, Y.-M.; Liu, W.; Yin, X.-B. Self-Limiting Growth Nanoscale Coordination Polymers for Fluorescence and Magnetic Resonance Dual-Modality Imaging. Adv. Funct. Mater. 2016, 26, 8463–8470. [Google Scholar] [CrossRef]
- He, C.; Lu, K.; Liu, D.; Lin, W. Nanoscale Metal–Organic Frameworks for the Co-Delivery of Cisplatin and Pooled siRNAs to Enhance Therapeutic Efficacy in Drug-Resistant Ovarian Cancer Cells. J. Am. Chem. Soc. 2014, 136, 5181–5184. [Google Scholar] [CrossRef]
- Horcajada, P.; Chalati, T.; Serre, C.; Gillet, B.; Sebrie, C.; Baati, T.; Eubank, J.F.; Heurtaux, D.; Clayette, P.; Kreuz, C.; et al. Porous metal–organic-framework nanoscale carriers as a potential platform for drug delivery and imaging. Nat. Mater. 2009, 9, 172–178. [Google Scholar] [CrossRef]
- Lawson, H.D.; Walton, S.P.; Chan, C. Metal–Organic Frameworks for Drug Delivery: A Design Perspective. ACS Appl. Mater. Interfaces 2021, 13, 7004–7020. [Google Scholar] [CrossRef]
- Chen, R.; Zhang, J.; Chelora, J.; Xiong, Y.; Kershaw, S.V.; Li, K.F.; Lo, P.K.; Cheah, K.W.; Rogach, A.L.; Zapien, J.A.; et al. Ruthenium (II) complex incorporated UiO-67 metal–organic framework nanoparticles for enhanced two-photon fluorescence imaging and photodynamic cancer therapy. ACS Appl. Mater. Interfaces 2017, 9, 5699–5708. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.M.; Liu, W.; Yin, X.B. Multifunctional mixed-metal nanoscale coordination polymers for triple-modality imaging-guided photodynamic therapy. Chem. Sci. 2017, 8, 3891–3897. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.; Yu, B.; Zhang, P.; Huang, J.; Chen, Y.; Gasser, G.; Ji, L.; Chao, H. Highly Charged Ruthenium(II) Polypyridyl Complexes as Lysosome-Localized Photosensitizers for Two-Photon Photodynamic Therapy. Angew. Chem. Int. Ed. 2015, 54, 14049–14052. [Google Scholar] [CrossRef]
- Kong, X.J.; Lin, Z.; Zhang, Z.M.; Zhang, T.; Lin, W. Hierarchical Integration of Photosensitizing Metal-Organic Frameworks and Nickel-Containing Polyoxometalates for Efficient Visible-Light-Driven Hydrogen Evolution. Angew. Chem. Int. Ed. 2016, 55, 6411–6416. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; deKrafft, K.E.; Lin, W. Pt nanoparticles@photoactive metal-organic frameworks: Efficient hydrogen evolution via synergistic photoexcitation and electron injection. J. Am. Chem. Soc. 2012, 134, 7211–7214. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Chen, L.; Bai, Z.; Zhang, D.; Guan, J.; Zhang, Y.; Shi, C.; Diwu, J. In Vivo Uranium Sequestration using a Nanoscale Metal–Organic Framework. Angew. Chem. 2021, 133, 1670–1674. [Google Scholar] [CrossRef]
- Tan, Y.; Sun, D.; Yu, H.; Yang, B.; Gong, Y.; Yan, S.; Chen, Z.; Cai, Q.; Wu, Z. Crystallization mechanism analysis of noncrystalline Ni–P nanoparticles through XRD, HRTEM and XAFS. CrystEngComm 2014, 16, 9657. [Google Scholar] [CrossRef]
- Liu, J.; Bu, J.; Bu, W.; Zhang, S.; Pan, L.; Fan, W.; Chen, F.; Zhou, L.; Peng, W.; Zhao, K. Real-time in vivo quantitative monitoring of drug release by dual-mode magnetic resonance and upconverted luminescence imaging. Angew. Chem. 2014, 126, 4639–4643. [Google Scholar] [CrossRef]
- Yuan, Y.; Zhang, C.J.; Xu, S.; Liu, B. A self-reporting AIE probe with a built-in singlet oxygen sensor for targeted photodynamic ablation of cancer cells. Chem. Sci. 2016, 7, 1862–1866. [Google Scholar] [CrossRef] [Green Version]
- Fateminia, S.A.; Kacenauskaite, L.; Zhang, C.J.; Ma, S.; Manghnani, P.N.; Chen, J.; Xu, S.; Hu, F.; Xu, B.; Lauren, B.W.; et al. Simultaneous increase in brightness and singlet oxygen generation of an organic photosensitizer by nanocrystallization. Small 2018, 14, 1803325. [Google Scholar] [CrossRef]
- Huang, P.; Wang, W.; Zhou, J.; Zhao, F.; Zhang, Y.; Liu, J.; Liu, J.; Dong, A.; Kong, D.; Zhang, J. Amphiphilic polyelectrolyte/prodrug nanoparticles constructed by synergetic electrostatic and hydrophobic interactions with cooperative pH-sensitivity for controlled doxorubicin delivery. ACS Appl. Mater. Interfaces 2015, 7, 6340–6350. [Google Scholar] [CrossRef]
- Podila, R.; Brown, J.M. Toxicity of engineered nanomaterials: A physicochemical perspective. J. Biochem. Mol. Toxicol. 2013, 27, 50–55. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Sun, D.; Fan, Q.; Ma, Q.; Dong, Z.; Tao, W.; Tao, H.; Liu, Z.; Wang, C. The enhanced permeability and retention effect based nanomedicine at the site of injury. Nano Res. 2020, 13, 564–569. [Google Scholar] [CrossRef]
- Marsh, S.R.; Pridham, K.J.; Jourdan, J.; Gourdie, R.G. Novel Protocols for Scalable Production of High Quality Purified Small Extracellular Vesicles from Bovine Milk. Nanotheranostics 2021, 5, 488–498. [Google Scholar] [CrossRef] [PubMed]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.-M.; Xu, Y.; Zhang, X.; Cui, Y.; Liang, Q.; Liu, C.; Wang, X.; Wu, S.; Yang, R. Single Nano-Sized Metal–Organic Framework for Bio-Nanoarchitectonics with In Vivo Fluorescence Imaging and Chemo-Photodynamic Therapy. Nanomaterials 2022, 12, 287. https://0-doi-org.brum.beds.ac.uk/10.3390/nano12020287
Wang Y-M, Xu Y, Zhang X, Cui Y, Liang Q, Liu C, Wang X, Wu S, Yang R. Single Nano-Sized Metal–Organic Framework for Bio-Nanoarchitectonics with In Vivo Fluorescence Imaging and Chemo-Photodynamic Therapy. Nanomaterials. 2022; 12(2):287. https://0-doi-org.brum.beds.ac.uk/10.3390/nano12020287
Chicago/Turabian StyleWang, Yong-Mei, Ying Xu, Xinxin Zhang, Yifan Cui, Qingquan Liang, Cunshun Liu, Xinan Wang, Shuqi Wu, and Rusen Yang. 2022. "Single Nano-Sized Metal–Organic Framework for Bio-Nanoarchitectonics with In Vivo Fluorescence Imaging and Chemo-Photodynamic Therapy" Nanomaterials 12, no. 2: 287. https://0-doi-org.brum.beds.ac.uk/10.3390/nano12020287