1. Introduction
Including more than 100 different diseases, cancer is characterized by disordered cells growth with the ability to invade tissues and organs; some types of tumor cells can also spread to other body parts in a process called metastasis [
1]. According to the International for Union Against Cancer (UICC), in 2020, an estimate of 15 million new cases of cancer will occur and this disease will be responsible for 12% of deaths worldwide, considering the non-infectious causes of death.
Multidrug resistance (MDR) is one of the main obstacles of anticancer treatment and believed to cause treatment failure in over 90% of patients with metastatic cancer [
2]. Although most patients initially respond to chemotherapy, a significant percentage of them relapse, developing resistance to a broad spectrum of structurally unrelated drugs that do not share a common target [
3].
One of the major causes of multidrug resistance is the enhanced efflux of drugs by membrane ABC (ATP-binding cassete) transporters. Targeting ABC transporters projects a promising approach to eliminating or suppressing drug resistance in cancer treatment [
4]. Among these members, P-glycoprotein (P-gp, also referred to as multidrug resistance protein 1, MDR1, or ABCB1) is the best characterized efflux pump that mediates cancer MDR [
5].
Structurally, P-gp is formed by four-domain architecture consisting of two cytoplasmic nucleotide-binding domains (NBDs) that bind and hydrolyse ATP and two transmembrane domains (TMDs) that recognize and transport substrates [
6]. Abundant in gastrointestinal and hepatic systems, P-gp acts as a drug efflux pump capturing drug molecules in cytoplasma and returning them to the cell interstice [
7]. Among general strategy to overcome multidrug resistance is the coadministration of P-gp chemical inhibitors with anticancer drugs [
8].
Apiole is a phenylpropanoid found in the roots, seeds and leaves of parsley (Apiaceae), but also in Lauraceae and Piperaceae species [
9]. This compound is popularly known as an abortifacient. Medicinal properties such as antioxidant, antibacterial, antihyperlipidemic, antihypercholesterolemic, antimycobacterial, chemopreventive, antidiabetic and anti-inflammatory have been described. Beneficial uses reported for apiole include the treatment of uterus diseases and cervical ectropio [
10]. There are few studies in the scientific field showing that apiole can suppress colorectal cancer cell growth [
11,
12,
13], in addition to being a potent calcium channel inhibitor [
14,
15].
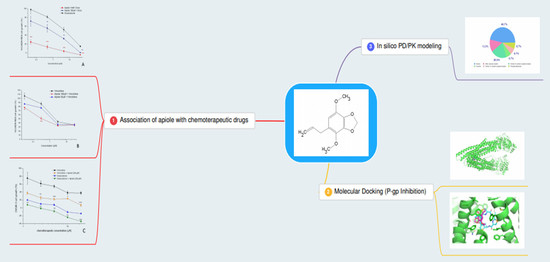
Considering that calcium channel blockers have been shown to be substrates for P-gp and potent MDR reversers [
16], this study aimed to evaluate the action of apiole in adjuvant treatment with well-established chemotherapy drugs used in the clinic, such as doxorubicin and vincristine, on ovarian tumor cell lines.
3. Discussion
The development of MDR is one of the main obstacles in chemotherapy treatment against tumors [
23]. This resistance is multifactorial, and may result, among other factors, from the activation or overexpression of proteins from ABC transporter family (ATP Binding Cassette). Resistance to chemotherapeutic drugs promoted by P-gp, a well characterized ABC-transporter, is the most studied form of resistance in vitro, in vivo and in the clinic and, consequently, a large number of compounds are investigated for their abilities to affect the phenomenon [
24].
Many drugs, including calcium channel blockers, prevent P-gp phosphorylation, which is necessary for the protein’s pumping function. By blocking this resistance mechanism, the chemotherapeutic agent is able to produce antiproliferative effect repeatedly [
25]. As a calcium channel blocker [
11], initially it was hypothesized that apiole’s mechanism of action was the same as first, second and third-generation modulators, binding to the P-gp present in the ovarian tumor cells membrane, inhibiting the extrusion mechanism of chemotherapeutic agents, and consequently, potentiating the substance’s antiproliferative activity. Molecular docking analysis gave insights that apiole has an affinity to the active site of the P-glycoprotein, evidenced by the efficient binding force to this protein. Such results suggest that this compound may inhibit P-gp.
The potential use of calcium channel blocking drugs in cancer therapy to revert MDR [
26] and the affinity to P-gp observed for apiole by molecular docking prompted the antiproliferative study associating apiole and two chemotherapeutic drugs frequently used in the clinic (doxorubicin and vincristine) in two ovarian cancer cell lines (NCI/ADR-RES, which expresses the phenotype of resistance to multiple drugs, characterized by the high expression of P-gp [
27]; and OVCAR-3).
The results herein presented revealed a synergistic effect when apiole was associated with doxorubicin and vincristine, in a concentration-dependent manner, in both ovarian tumor lines, being more effective in the resistant cell line NCI/ADR-RES, which reinforced the involvement of apiole with P-gp.
Considering the potential use clinical use of apiol in association with chemotherapeutic drugs, we evaluated in silico some parameters for druglikeness according Lipinski’s criteria. These evaluations demonstrated that apiole presented high water solubility suggesting compatibility with biologic fluids associated with adequated balance between and the hydrogen-bond acceptors and donors are adequate for water and target interactions [
28]. The calculated logP for apiol (2.85) suggested a good ability to cross plasmatic membranes which might reflect its high gastrointestinal absorption. This parameter reflects the possibility of one substance to reach the molecular target at effective concentration after oral administration [
29]. Besides, the in silico evaluation has shown that apiole has no ability to inhibit the main hepatic enzymes (P450 complex) suggesting a lower risk of drug interaction mediated by interference drug metabolism.
The low toxicity predicted for apiole was confirmed by previous studies. In mice tumor models [
12,
13], apiole promoted antitumor effects without clinical signs of toxicity up to 30 mg/kg, three times per week, by intraperitoneal route. In comparison to other allylbenzenes derivatives, apiole was found as the less potent genotoxic agent [
30,
31]. A careful toxicological study should be considered for apiole, once this molecule is popularly known by its abortive and toxic effects.
Despite considerable in vitro success, there are no compounds currently available to block P-gp–mediated resistance in the clinic. The failure may be attributed to toxicity, adverse drug interaction, and numerous pharmacokinetic issues [
32].
The most important first generation calcium channel blocker, verapamil, failed in clinical trials because the plasmatic concentration required to reverse MDR (6–10 µM) was higher than that required to promote effects on the cardiovascular system (1 to 2 µM) [
33]. These significant cardiovascular adverse effects still limit in the clinic use of verapamil [
34]. Despite showing better pharmacological ant toxic profiles, the second-generation of P-gp modulators, represented by valspodar and biricodar, also failed in clinical trails mainly because they are substrates for cytochrome P450 superfamily, especialy CYP3A4. Considering the key role of CYP3A4 in the metabolism and excretion of cytotoxic agents, the coadministration of a potential modulator of both P-gp and CYP3A4 might promote unwanted changes on pharmacokinetic parameters of the chemotherapeutic agent leading to toxic drug-drug interactions. A third generation of P-gp inhibitors is represented by tariquidar, which has high affinity to P-gp at nanomolar concentrations. This generation of P-gp inhibitors has been examined in preclinical and clinical studies; however, the trials have largely failed to demonstrate an improvement in therapeutic efficacy [
19,
32,
33,
34]. Therefore, the search for resistance reversal modulators that do not present adverse effects to be introduced in the clinic has been incessant. New strategies to find forth generation of P-gp inhibitors have been used by investigators, such as the “return” to natural products [
19].
In this context, our in silico and in vitro results together with the in vitro and in vivo data available in literature pointed out that apiole could be a promisor alternative to reverse MDR in cancer chemotherapy with low potential to elicit unwanted drug-drug interactions. Further non-clinical studies should be done to complement both pharmacological (adjuvant calcium channel blocker in cancer therapy) and toxicological evaluation of apiole. To the best of our knowledge, this is the first article to report the chemoreversion property of apiole.
4. Material and Methods
4.1. Isolation of Apiole Obtained from Piper Regnellii (Miq.) C. DC. var. Regnellii Leaves
Apiole was isolated from Piper regnellii (Miq.) C. DC. var. regnellii leaves. Briefly, Piper regnellii (Miq.) C. DC. var. regnellii leaves (voucher number CPMA 221) were collected at Centro Pluridisciplinar de Pesquisas Químicas, Biológicas e Agrícolas (CPQBA, Universidade Estadual de Campinas, São Paulo, Brazil). From the dry milled leaves (218 g) the dichloromethane crude extract was obtained (DCE, 6% yield) and fractionated by column chromatography using silica gel with an increasing gradient of hexane, dichloromethane, and methanol, providing 48 fractions (50 mL each one). The resulting fractions were grouped (FRA-FRG) according to thin-layer chromatography (TLC) profile. FRD was submitted to successive column chromatography with silica gel eluted with hexane and ethyl acetate (90:10), providing apiole (345 mg,
Figure 1). The identification of apiole was accomplished by comparison of nuclear magnetic resonance (NMR 1H and 13C NMR), mass spectrometry (MS) data, and melting point with the literature [
17].
4.2. Cell Culture
Human tumor cell lines [U251 (central nervous system, glioblastoma), MCF7 (breast, adenocarcinoma), NCI/ADR-RES (multidrug resistant ovarian adenocarcinoma), 786-0 (renal adenocarcinoma), NCI-H460 (lung, large cell carcinoma), PC-3 (prostate, adenocarcinoma), OVCAR-3 (ovarian adenocarcinoma) and HT29 (colon, adenocarcinoma)] were kindly donated by the National Cancer Institute at Frederick MA-USA. Stock cultures were grown in complete medium [RPMI 1640 medium supplemented with 5% fetal bovine serum and 1% penicillin:streptomycin mixture (1000 U∙mL−1:1000 µg·mL−1)] at 37 °C with 5% CO2.
4.3. Sample Preparation
(Doxorubicin Hydrochloride
®—Europharma) and vincristine (Tecnocris Sulfato de Vincristina
®—Zodiac) were prepared aseptically in DMSO (100 mg/mL) and diluted in in complete medium to afford the final concentration. The final DMSO concentration (≤0.25%) in the experiments did not affect cell viability [
35].
4.4. Antiproliferative Activity Evaluation
Briefly, the tumor cells were seeded in 96-well plates (T1 plates, between 3 to 6 × 10
4 cells/mL, 100 µL/well), incubated for 24 h, treated with apiole (1, 10, 100 µM and 1 mM, 100 µL/well), doxorubicin (0.046, 0.46, 4.6 and 46 µM, 100 µL/well) and vincristine (0.03, 0.3, 3 and 30 µM, 100 µL/well), in triplicate, and then incubated for 48 h at 37 °C in 5% CO
2. A second plate, denominated T0, was prepared to infer the absorbance value of untreated cells at the moment of sample addition. Untreated (T0 and T1 plates) and treated (T1 plates) cells were fixed with 50% trichloroacetic acid and stained with sulforhodamine dye (0.4% in acetic acid 1%). Absorbance was recorded at 540 nm using a microplate reader (Molecular Devices
®, VersaMax model). Using the absorbance values, the cell growth (%) for each cell line, at each sample concentration, was calculated considering at 100% of cell growth the difference between the absorbances of untreated cells after 48 h incubation (T1) and at the sample addition moment (T0). The curve cell growth vs. sample concentration was plotted and GI
50 (concentration required for 50% growth inhibition) was calculated by sigmoidal regression using the Origin 8.0 software (OriginLab Corporation, Northampton, MA, USA) [
36].
4.5. Influence of Apiole on the Antiproliferative Activity of Doxorubicin and Vincristine in Human Ovarian Tumor Lines (NCI/ADR-RES and OVCAR-3)
Following the protocol already described for the antiproliferative activity evaluation, NCI/ADR-RES and OVCAR-3 cells were seeded in 96-well plates (T1 plates, 4 and 5 × 104 cells/mL, respectively, 100 µL/well). After 24 h of incubation, NCI/ADR-RES cell was treated doxorubicin (0.045, 0.45, 4.5 and 45 µM) associated with apiole at 10, 100 µM and 1 mM assay or vincristine (0.03, 0.3, 3 and 30 µM) associated with apiole at 25, 50 and 100 µM. For treatment of OVCAR-3 cells, both doxorubicin (0.045, 0.45, 4.5 and 45 µM) and vincristine (0.03, 0.3, 3 and 30 µM) were associated with apiole at 100 µM. A T0 plate was prepared for each experiment. After 48h-exposure, cell proliferation was determined as described for the antiproliferative activity evaluation.
For the analysis of the combinatorial effect, the concentration reduction index (CRI) was calculated as CRI = GI
50 cytotoxic drug alone/GI
50 cytotoxic drug alone+apiol. CRI values higher than 1 indicated synergistic combination [
37].
4.6. Molecular Docking
The target (P-gp) for molecular docking was selected in the RCSB PDB (Protein Data Bank)—accession code 3G60, chain A, with 4.40 Å resolution. OpenBabel Cheminformatics tools of ChemInfo [
38] was used to optimize the energy of the ligand (apiole), which was drawn and converted to mol.2 format, with 3D parameters and pH 7. The protein was prepared with Maestro 11.7 (Shrodinger
® 2018; small-molecule drug discovery suite) using Protein Preparation Wizard (Epik pH: 7.4 ± 0.5 and OPLS3e force field). The grid was defined by 20 Å × 20 Å × 20 Å box centred in the central ligand QZ59 position (co-crystal template for comparison). The ligand docking was carried out by replacing the QZ59 with Apiole, using all atoms for docking and hydrogen atoms added, considering pH 7.
4.7. In Silico Pharmacodynamics
The apiole structure was also submitted to ADME analysis, in order to verify the compound’s physico-chemical properties, solubility, lipophilicity, pharmacokinetics parameters (gastrointestinal and brain-blood barrier absorption and hepatic enzymes inhibition) and druglikeness, following the medicinal chemistry alert [
39].
4.8. Statistical Analysis
Statistical analysis was performed using GraphPad Prism®. Comparisons among groups (three or more), considering only one independent variable/factor, were performed using One-way ANOVA followed by Tukey post-hoc tests. The results were expressed as the mean ± SD and the level of significance was 5 %.