The Interest of a Systematic Toxicological Analysis Combined with Forensic Advice to Improve the Judicial Investigation and Final Judgment in Drug Facilitated Sexual Assault Cases
Abstract
:1. Introduction
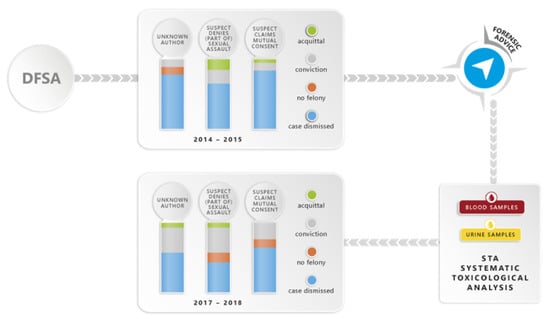
2. Results
2.1. Study Population
2.2. STA Results
2.3. FA Interpretation
3. Discussion
4. Materials and Methods
4.1. Case Selection
4.2. STA
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- United Nations Office on Drugs and Crime. Guidelines for the Forensic Analysis of Drugs Facilitating Sexual Assault and Other Criminal Acts. United Nations, New York. 2011. Available online: https://www.unodc.org/documents/scientific/forensic_analys_of_drugs_facilitating_sexual_assault_and_other_criminal_acts.pdf (accessed on 19 March 2021).
- Anderson, L.J.; Flynn, A.; Pilgrim, J.L. A global epidemiological perspective on the toxicology of drug-facilitated sexual assault: A systematic review. J. Forensic. Leg. Med. 2017, 47, 46–54. [Google Scholar] [CrossRef]
- Kilpatrick, D.G.; Resnick, H.S.; Ruggiero, K.J.; Cognoscenti, L.M.; McCauley, J. Drug-Facilitated, Incapacitated, and Forcible Rape: National Study; Final Report Submitted to the National Institute of Justice (Document No. NCJ 219181). 2007. Available online: http://www.ncjrs.gov/pdffiles1/nij/grants/219181.pdf (accessed on 19 March 2021).
- LeBeau, M.A.; Montgomery, M.A. The frequency of drug-facilitated sexual assault investigations. Forensic Sci. Rev. 2010, 22, 7–14. [Google Scholar] [PubMed]
- Adamowicz, P.; Kala, M. Date-rape drugs scene in Poland. Przegl. Lek. 2005, 62, 572–575. [Google Scholar] [PubMed]
- Hurley, M.; Parker, H.; Wells, D.L. The epidemiology of drug facilitated sexual assault. J. Clin. Forensic Med. 2006, 13, 181–185. [Google Scholar] [CrossRef] [PubMed]
- McGregor, M.J.; Lipowska, M.; Shah, S.; Du, M.J.; De Siato, C. An exploratory analysis of suspected drug-facilitated sexual assault seen in a hospital emergency department. Women Health 2003, 37, 71–80. [Google Scholar] [CrossRef]
- Questel, F.; Sec, I.; Sicot, R.; Pourriat, J.-L. Drug-facilitated crimes: Prospective data collection in a forensic unit in Paris. Presse Med. 2009, 38, 1049–1055. [Google Scholar] [CrossRef] [PubMed]
- Scott-Ham, M.; Burton, F.C. Toxicological findings in cases of alleged drug-facilitated sexual assault in the United Kingdom over a 3-year period. J. Clin. Forensic Med. 2005, 12, 175–186. [Google Scholar] [CrossRef]
- Federale Politie (DGR/DRI/BiPol). Politiële criminaliteitsstatistieken België 2000-1e Semester. 2018. Available online: https://www.pzgrens.be/sites/default/files/Criminaliteitsstatistieken%20PZ%20Grens%20tot%202020%201ste%20semester.pdf (accessed on 19 March 2021).
- LeBeau, M.A. Guidance for improved detection of drugs used to facilitate crimes. Ther. Drug Monit. 2008, 30, 229–233. [Google Scholar] [CrossRef]
- UN report Preventing Sexual Exploitation and Abuse. Available online: https://www.un.org/preventing-sexual-exploitation-and-abuse/content/secretary-generals-reports. (accessed on 9 March 2021).
- Bitzer, S.; Heudt, L.; Barret, A.; George, L.; Van Dijck, K.; Gason, F.; Renard, B. The introduction of forensic advisors in Belgium and their role in the criminal justice system. Sci. Justice 2018, 58, 177–184. [Google Scholar] [CrossRef]
- LeBeau, M.A.; Montgomery, M.A. Challenges of drug-facilitated sexual assault. Forensic Sci. Rev. 2010, 22, 1–6. [Google Scholar]
- LeBeau, M.A. Laboratory management of drug-facilitated sexual assault cases. Forensic Sci. Rev. 2010, 22, 113–119. [Google Scholar]
- Juhascik, M.P.; Negrusz, A.; Faugno, D.; Ledray, L.; Greene, P.; Lindner, A.; Haner, B.; Gaensslen, R.E. An estimate of the proportion of drug-facilitation of sexual assault in four U.S. localities. J. Forensic Sci. 2007, 52, 1396–1400. [Google Scholar] [CrossRef] [PubMed]
- Kerrigan, S. The use of alcohol to facilitate sexual assault. Forensic Sci. Rev. 2010, 22, 15–32. [Google Scholar]
- Couper, F.J.; Saady, J.J. The use of miscellaneous prescription medicatins to facilitate sexual assault. Forensic Sci. Rev. 2010, 22, 83–112. [Google Scholar] [PubMed]
- Kummer, N.; Lambert, W.E.; Samyn, N.; Stove, C.P. Alternative sampling strategies fort the assessment of alcohol intake of living persons. Clin. Biochem. 2016, 49, 1078–1091. [Google Scholar] [CrossRef] [PubMed]
- Wille, S.M.R.; Richeval, C.; Nachon-Phanithavong, M.; Gaulier, J.M.; Di Fazio, V.; Humbert, L.; Samyn, N.; Allorge, D. Prevalence of new psychoactive substances and prescription drugs in the Belgian driving under the influence of drugs population. Drug Test Anal. 2018, 10, 539–547. [Google Scholar]
- Stockham, T.; Rohrig, T.P. The use of ‘Z-drugs’ to facilitate sexual assault. Forensic Sci. Rev. 2010, 22, 61. [Google Scholar]
- Montgomery, M.A. The use of benzodiazepines to facilitate sexual assault. Forensic Sci. Rev. 2010, 22, 33–40. [Google Scholar]
- Forensic Toxicology screening Application Solution, Waters. Available online: https://www.waters.com/waters/high-resolution-ms-non-targeted-screening/nav.htm?&cid=134779723&&locale=en_BE (accessed on 23 March 2020).
- Elliott, S.P. Gamma hydroxybutyric acid (GHB) concentrations in humans and factors affecting endogenous production. Forensi Sci. Int. 2003, 133, 9–16. [Google Scholar] [CrossRef]
- Laloup, M.; Ramirez-Fernandez, M.; De Boeck, G.; Wood, M.; Maes, V.; Samyn, N. Validation of a liquid chromatography-tandem mass spectrometry method for the simultaneous determination of 26 benzodiazepines and metabolites, zolpidem and zopiclone in blood, urine, and hair. J. Anal. Toxicol. 2006, 29, 616–626. [Google Scholar] [CrossRef] [Green Version]
- Ramirez Fernandez, M.; Wille, S.M.R.; Samyn, N. Quantitative method validation for the analysis of 27 antidepressants and metabolites in plasma with ultra performance liquid chromatography tandem mass spectrometry. Ther. Drug Monit. 2012, 34, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Ramirez Fernandez, M.; Samyn, N. Ultra-performance liquid chromatography-tandem mass spectrometry method for the analysis of amphetamines in plasma. J. Anal. Toxicol. 2011, 35, 577–582. [Google Scholar]
- Ramirez Fernandez, M.; De Boeck, G.; Wood, M.; Lopez-Rivadulla, M.; Samyn, N. Simultaneous analysis of THC and its metabolites in blood using liquid chromatography-tandem mass spectrometry. J. Chromatogr. B 2008, 875, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Ramirez Fernandez, M.; Laloup, M.; Wood, M.; De Boeck, G.; Lopez-Rivadulla, M.; Wallemacq, P.; Samyn, N. Liquid chromatography-tandem mass spectrometry method for the simultaneous analysis of multiple hallucinogens, chlorpheniramine, ketamine, ritalinic acid, and metabolites in urine. J. Anal. Toxicol. 2007, 31, 497–504. [Google Scholar] [CrossRef] [Green Version]
- Ramirez Fernandez, M.; Wille, S.M.R.; Di Fazio, V.; Gosselin, M.; Samyn, N. Analysis of amphetamines and metabolites in urine with ultra performance liquid chromatography tandem mass spectrometry. J. Chromatogr. B 2010, 878, 1616–1622. [Google Scholar] [CrossRef]
- Ramirez Fernandez, M.; Van Durme, F.; Wille, S.M.; Di Fazio, V.; Kummer, N.; Samyn, N. Validation of an Automated Solid Phase Extraction Method for the Analysis of 23 Opioids, Cocaine and Metabolites in Urine with Ultra Performance Liquid Chromatography-Tandem Mass Spectrometry. J. Anal. Toxicol. 2014, 38, 280–288. [Google Scholar] [CrossRef] [Green Version]
- Ramirez Fernandez, M.; Wille, S.M.; Kummer, N.; di Fazio, V.; Samyn, N. Quantitative Analysis of 26 Opioids, Cocaine, and their Metabolites in Human Blood by Ultra Performance Liquid Chromatography-Tandem Mass Spectrometry. Ther. Drug Monit. 2013, 4, 510–521. [Google Scholar] [CrossRef]
- Wille, S.M.R.; Peters, P.T.; Di Fazio, V.; Samyn, N. Practical aspects concerning validation and quality control for forensic and clinical bioanalytical quantitative methods. Accred Qual. Assur. 2011, 16, 279–292. [Google Scholar]
- Wille, S.M.R.; Coucke, W.; De Baere, T.; Peters, P.T. Update of Standard Practices for New Method Validation in Forensic Toxicology. Curr. Pharma. Des. 2017, 23, 5442–5454. [Google Scholar] [CrossRef]




| Case N° | Age (Years) | Gender | Information According to Victim | Time between Sexual Assault and Sampling | STA Blood | STA Urine | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Suspicion of Being Drugged | Voluntary Intake | Detected | Back Calculation | |||||||
| Drugs | Medication in the Week before the Assault | Alcohol | ||||||||
| 1 | >14–16 | F | ■ | 07h40 | 8.9 ng/mL THC-COOH | THC-COOH | ||||
| 2 | >14–16 | F | ■ | 08h50 | 5.1 ng/mL THC-COOH | Cetirizine, THC-COOH | ||||
| 3 | >18 | F | ■ | 01h44 | Negative | Negative | ||||
| 4 | >16–18 | M | ■ | 05h10 | 88.2 ng/mL Fluoxetine, 264 ng/mL Norfluoxetine, 21.5 ng/mLMethylphenidate, >300 ng/mL Rilatinic acid, 34.3 ng/mL Aripiprazol | Fluoxetine, DMF, Methylphenidate, Rilatinic acid, Aripiprazol | ||||
| 5 | >18 | F | ■ | 09h30 | 1.56 g/L Ethanol, Paracetamol, Bromazepam | 3.09 g/L Ethanol | 2.43 g/L Ethanol, Paracetamol, Bromazepam | |||
| 6 | >18 | F | ■ | 13h30 | Negative | N/A | ||||
| 7 | >18 | F | 24h00 | Negative | Paracetamol | |||||
| 8 | >18 | F | 44h30 | Negative | Negative | |||||
| 9 | >18 | F | ■ | ■ | 11h10 | Negative | Aspirin, Metipranol | |||
| 10 | >16–18 | F | 06h30 | Azithromycin | Azithromycin | |||||
| 11 | >16–18 | F | ■ | 14h08 | 86.5 ng/mL Aripiprazol | Aripiprazol | ||||
| 12 | >18 | F | 12h00 | N/A | 3.11 g/L Ethanol, Trazodone, m-Cpp, Cocaine, BZE, EME, CE, Levamisole, Paracetamol, Doxylamine | |||||
| 13 | >18 | M | ■ | ■ | ■ | 68h22 | 138 ng/mL Nordiazepam, 3.0 ng/mL Oxazepam | Nordiazepam, Oxazepam, BZE, THC-COOH | ||
| 14 | >18 | F | ■ | ■ | 32h45 | Negative | Negative | |||
| 15 | >18 | F | ■ | 17h00 | Paracetamol | Paracetamol, Piracetam, BZE | ||||
| 16 | >14–16 | F | 11h45 | Negative | Negative | |||||
| 17 | >18 | F | 04h20 | Negative | Negative | |||||
| 18 | >18 | M | 05h00 | 1.81 g/L Ethanol | 2.56 g/L Ethanol | 2.45 g/L Ethanol, THC-COOH | ||||
| 19 | >18 | F | ■ | 14h30 | Valsartan | Valsartan, Nevibolol | ||||
| 20 | >10–14 | F | 30h40 | Negative | Aspirin | |||||
| 21 | >18 | F | 09h20 | Negative | Negative | |||||
| 22 | >18 | F | ■ | 24h00 | Negative | Negative | ||||
| 23 | >18 | F | ■ | ■ | ■ | 14h30 | 0.47 g/L Ethanol | 0.40 g/L Ethanol, Aspirin | ||
| 24 | >18 | F | 03h00 | 235 ng/mL Bromazepam, 2807 ng/mL Amphetamine, 5.8 ng/mL THC-COOH | 0.16 g/L Ethanol, Bromazepam, Temazepam, Amphetamine, Methamphetamine, GHB (336.2 µL/mL), THC-COOH, BZE, Paracetamol | |||||
| 25 | >16–18 | F | ■ | ■ | 06h00 | 37.8 ng/mL Diazepam, 4.7 ng/mL THC-COOH | 0.44 g/L Ethanol, Diazepam, Nordiazepam, Temazepam, THC-COOH | |||
| 26 | >18 | F | ■ | ■ | 24h00 | 1.09 g/L Ethanol, 19.6 ng/mL Citalopram, 5.4 DMC | 0.46 g/L Ethanol, Citalopram, DMC | |||
| 27 | >18 | F | 04h00 | 0.38 g/L Ethanol, Naproxen, Ibuprofen | 0.98 g/L Ethanol | 0.72 g/L Ethanol, Naproxen, Ibuprofen, THC-COOH | ||||
| 28 | >16–18 | F | 02h00 | Salbutamol | Salbutamol, BZE, EME | |||||
| 29 | >18 | F | 04h40 | N/A | Negative | |||||
| 30 | >18 | F | 03h50 | 24.5 ng/mL Trazodone, 9 ng/mL Dosulepin, 0.8 ng/mL Zolpidem, 6.1 ng/mL Alprazolam, 31.0 ng/mL Amisulpride | Trazodone, Dosulepin, Duloxetine, Zolpidem, Alprazolam, OH-Alprazolam, Amisulpride, Gliclazide, Bisoprolol, BZE | |||||
| 31 | >18 | F | 19h10 | Negatieve | Diclophenac | |||||
| 32 | >18 | F | 06h20 | Negative | Negative | |||||
| 33 | >18 | F | ■ | 34h00 | Negative | Negative | ||||
| 34 | >18 | F | ■ | ■ | 16h00 | 7.5 ng/mL BZE, 166 MDMA, 17.0 MDA | 0.22 g/L Ethanol, BZE, EME, Cocaine, MDMA, MDA | |||
| 35 | >16–18 | F | ■ | 04h20 | 7.9 ng/mL Mirtazapine, 0.9 ng/mL Quetiapine, 4.7 ng/mL OH-Respiridone, 4.8 ng/mL Sulpiride | Mirtazapine, Quetiapine, OH-Respiridone, Sulpride, Metformine, Paracetamol | ||||
| 36 | >18 | F | ■ | ■ | 04h30 | 1.53 g/L Ethanol | 2.21 g/L Ethanol | 2.20 g/L Ethanol | ||
| 37 | >18 | F | ■ | ■ | 16h00 | Negative | Negative | |||
| 38 | >18 | F | ■ | 16h45 | N/A | Tramadol, Aspirin | ||||
| 39 | >18 | F | ■ | ■ | 15h00 | 83.0 ng/mL MDMA, 8.0 ng/mL MDA | MDMA, MDA | |||
| 40 | >18 | F | ■ | 16h50 | Negative | Negative | ||||
| 41 | >14–16 | F | 07h00 | Negative | Prometazine | |||||
| 42 | >14–16 | F | 08h00 | N/A | Negative | |||||
| 43 | >18 | F | 50h10 | 0.75 g/L Ethanol | 0.94 g/L Ethanol, Paracetamol, Piracetam | |||||
| 44 | >16–18 | F | ■ | ■ | 11h00 | 1.04 g/L Ethanol | 2.69 g/L | 1.47 g/L Ethanol | ||
| 45 | >16–18 | F | ■ | ■ | 09h50 | Negative | Negative | |||
| 46 | >18 | F | ■ | ■ | 15h50 | 38.4 ng/mL Sertraline, 156 ng/mL BZE, 10.2 ng/mL EME, 3.4 ng/mL CE | Sertraline, BZE, EME, CE, Cocaine, Xylometazoline | |||
| 47 | >18 | F | ■ | 15h00 | 233.4 ng/mL BZE, 8.5 ng/mL EME, 3.9 ng/mL CE | 0.11 g/L Ethanol, BZE, EME, CE, Cocaine | ||||
| 48 | >16–18 | F | 48h00 | Negative | Negative | |||||
| 49 | >18 | F | ■ | 02h00 | Paracetamol | Paracetamol | ||||
| 50 | >16–18 | F | ■ | 04h00 | 0.80 g/L Ethanol, Paracetamol, Piroxicam | 1.40 g/L Ethanol | 1.17 g/L Ethanol, Piroxicam, Paracetamol | |||
| 51 | >16–18 | M | 03h05 | 5.7 ng/mL Fluoxetine, 2.2 ng/mL Norfluoxetine, 21.0 ng/mL Aripiprazol | Fluoxetine, Norfluoxetine, Aripiprazol, Methylphenidate, Ritalinic acid | |||||
| 52 | >18 | F | ■ | 14h00 | Gliclazide, Metformine | Negative | ||||
| 53 | >16–18 | F | 48h00 | Negative | Negative | |||||
| 54 | >18 | F | 08h40 | Negative | Negative | |||||
| 55 | >18 | F | ■ | ■ | 18h15 | 17.7 ng/mL Trazodone, 10.7 ng/mL mCpp, 31.3 ng/mL Duloxetine | Trazodone, mCpp, Duloxetine | |||
| 56 | >18 | F | ■ | 18h10 | Negative | Negative | ||||
| 57 | >14–16 | F | ■ | 09h00 | Negative | 1.21 g/L Ethanol | ||||
| 58 | >18 | F | ■ | ■ | 48h00 | 21.0 ng/mL Cocaine, 139 ng/mL BZE, 138 ng/mL EME, 2.6 ng/mL CE | N/A | |||
| 59 | >18 | F | 04h30 | 166 ng/mL BZE, 12 ng/mL Cocaine, 10 ng/mL EME, 0.7 ng/mL THC, 0.6 ng/mL OH-THC, 50.6 ng/mL THC-COOH | BZE, Cocaine, EME, THC, OH- THC, THC-COOH, MDMA, MDA | |||||
| 60 | >18 | F | 24h00 | Lidocaine | Ibuprofen, Lidocaine | |||||
| 61 | >18 | F | ■ | 24h00 | 39.9 ng/mL Sertraline, 126 ng/mL Trazodone, 82.0 ng/mL Diazepam, 21.0 ng/mL Nordiazepam, 5.0 ng/mL Temazepam, 11.0 ng/mL Lorazepam | Sertraline, Trazodone, mCpp, Diazepam, Nordiazepam, Temazepam, Oxazepam, Lorazepam, 7-Aminoclonazepam, Pipamperone, Risperidone, Loperamide, DML | ||||
| 62 | >16–18 | F | ■ | ■ | 17h00 | Metronidazole, Azithromycine | Metronidazole, Azithromycine | |||
| 63 | >18 | F | ■ | 13h00 | 0.62 g/L Ethanol, 1.4 ng/mL Morphine, 10.2 ng/mL Codeine, 190 ng/mL Desalkylflurazepam, 39.0 ng/mL Diazepam, 20.0 ng/mL Nordiazepam, 3.8 ng/mL BZE, 2.5 ng/mL EME | 2.42 g/L | 2.18 g/L Ethanol, Morphine, Codeine, Hydrocodone, Flurazepam, Desalkylflurazepam, Diazepam, Nordiazepam, Temazepam, Alprazolam, Zolpidem, Cocaine, BZE, EME, Bisoprolol, Quetiapine, Norquetiapine, Haloperidol, THC-COOH | |||
| 64 | >18 | X | ■ | 02h35 | Piroxicam | Negative | ||||
| 65 | >18 | F | ■ | 01h15 | 0.28 g/L Ethanol | 0.47 g/L Ethanol | 0.91 g/L Ethanol | |||
| 66 | >16–18 | F | ■ | 25h00 | Negative | Trazodone, Aripiprazol, OH-risperidone | ||||
| 67 | >18 | F | ■ | ■ | 32h30 | 1.0 ng/mL Morphine, 1.8 ng/mL Codeine | Morphine, Codeine, Norcodeine | |||
| 68 | >18 | F | ■ | 04h15 | 147 ng/mL Trazodone, 1.1 ng/mL mCpp, 67 ng/mL Venlafaxine, 69 ng/mL DMV, 119 ng/mL Bromazepam, 12.1 Alprazolam, Pregabaline, Bisoprolol, Methformine, Gliclazide | Trazodone, mCpp, Venlafaxine, DMV, Bromazepam, Alprazolam, Pregabaline, Bisoprolol, Metoprolol, Methformine, Gliclazide, Amoxicilin, Loperamide, DML | ||||
| 69 | >18 | F | ■ | ■ | 44h00 | Negative | THC-COOH | |||
| 70 | >16–18 | X | ■ | ■ | 07h05 | >300 ng/mL Ritalinic acid | 0.75 g/L Ethanol, Methylphenidate, Ritalinic acid | |||
| 71 | >18 | F | ■ | 13h00 | Negative | Negative | ||||
| 72 | >14–16 | F | 05h00 | Negative | Negative | |||||
| 73 | >18 | F | ■ | ■ | 17h55 | 3.8 ng/mL BZE | BZE, Cocaine, EME, Levamisole, Bupropion | |||
| 74 | >14–16 | F | ■ | 23h30 | Negative | Negative | ||||
| 75 | >18 | F | ■ | ■ | 60h00 | 8.8 ng/mL Bupropion, 21.6 ng/mL Clonazepam, 15.4 ng/mL, 7-Aminoclonazepam | Bupropion OH-risperidone7-Aminoclonazepam Indapamide | |||
| 76 | >18 | F | ■ | ■ | ■ | 08h00 | 62 ng/mL Citalopram, 26 ng/mL DMC, 61 ng/mL Nortryptilline, 130 ng/mL Diazepam, 257 ng/mL Nordiazepam, 13 ng/mL Temazepam, 17 ng/mL Oxazepam, >300 ng/mL BZE, 48 ng/mL EME | Citalopram, DMC, Nortryptilline, Diazepam, Nordiazepam, Temazepam, Oxazepam, Lormetazepam, Lorazepam, BZE, EME, Cocaine, CE, THC-COOH | ||
| 77 | >18 | F | ■ | ■ | 12h40 | Negative | Negative | |||
| 78 | >18 | F | ■ | 05h00 | 0.61 g/L Ethanol | 1.36 g/L Ethanol | 1.11 g/L Ethanol | |||
| 79 | >18 | F | ■ | ■ | 10h27 | 1.43 g/L Ethanol, 9.2 ng/mL Venlafaxine, 65 ng/mL DMV, 617 ng/mL Trazodone | 1.19 g/L Ethanol, Venlafaxine, DMV, Trazodone, mCpp | |||
| ALCOHOL | |||||
| n | low (g/L) | high (g/L) | median (g/L) | mean (g/L) | |
| Ethanol | 13 | 0.28 | 1.81 | 0.80 | 0.95 |
| DRUGS | |||||
| n | low (ng/mL) | high (ng/mL) | median (ng/mL) | mean (ng/mL) | |
| Cocaine | 8 | ||||
| Cocaine | 2 | 12.0 | 21.0 | 16.5 | 16.5 |
| BZE | 8 | 3.8 | 698.0 | 147.3 | 175.9 |
| EME | 5 | 2.5 | 138.0 | 10.0 | 38.8 |
| CE | 3 | 2.6 | 3.9 | 3.4 | 3.3 |
| Cannabis | 5 | ||||
| THC | 1 | 0.7 | 0.7 | / | / |
| OH-THC | 1 | 0.6 | 0.6 | / | / |
| THC-COOH | 5 | 4.7 | 50.6 | 5.8 | 15.0 |
| Amphetamines | 3 | ||||
| MDMA | 2 | 83.0 | 166.0 | 124.5 | 124.5 |
| MDA | 2 | 8.0 | 17.0 | 12.5 | 12.5 |
| Amphetamine | 1 | 2807 | 2807 | / | / |
| MEDICATION | |||||
| n | low (ng/mL) | high (ng/mL) | median (ng/mL) | mean (ng/mL) | |
| Antidepressants | |||||
| Citalopram (DMC) | 2 | 19.6 (5.4) | 62 (26.0) | 40.8 (15.7) | 40.8 (15.7) |
| Bupropion | 1 | 8.8 | 8.8 | / | / |
| Duloxetine | 1 | 31.3 | 31.3 | / | / |
| Dosulepine | 1 | 9.0 | 9.0 | / | / |
| Fluoxetine (NF) | 2 | 5.7 (2.2) | 88.2 (263.9) | 46.9 (133.1) | 46.9 (133.1) |
| Mirtazapine | 1 | 7.9 | 7.9 | / | / |
| Nortryptyline | 1 | 61.0 | 61.0 | / | / |
| Sertraline | 2 | 38.4 | 39.9 | 39.2 | 39.2 |
| Trazodone (mCpp) | 5 | 9.2 (60.0) | 617.0 (10.7) | 126.4 (5.9) | 186.5 (5.9) |
| Venlafaxine (DMV) | 2 | 9.2 (65.0) | 67.0 (69.0) | 38.1 (67.0) | 38.1 (67.0) |
| Benzodiazepines | |||||
| Alprazolam | 2 | 6.1 | 12.1 | 9.1 | 9.1 |
| Bromazepam | 2 | 119 | 235 | 177 | 177 |
| Clonazepam (7-aminoC) | 1 | 21.6 (15.4) | 21.6 (15.4) | / | / |
| Desalkylflurazepam | 1 | 190.0 | 190.0 | / | / |
| Diazepam | 4 | 37.8 | 130.0 | 60.5 | 72.2 |
| Nordiazepam | 4 | 20.0 | 257.0 | 79.6 | 109.1 |
| Oxazepam | 2 | 3.0 | 17.0 | 10.0 | 10.0 |
| Temazepam | 2 | 5.0 | 13.0 | 9.0 | 9.0 |
| Lorazepam | 1 | 11.0 | 11.0 | / | / |
| Zolpidem | 1 | 0.8 | 0.8 | / | / |
| Neuroleptics | |||||
| Aripiprazol | 3 | 21.0 | 86.5 | 34.3 | 47.3 |
| Amisulpride | 1 | 31.0 | 31.0 | / | / |
| Quetiapine | 1 | 0.9 | 0.9 | / | / |
| OH-Risperidone | 1 | 4.7 | 4.7 | / | / |
| Sulpride | 1 | 4.8 | 4.8 | / | / |
| Opioids | |||||
| Morphine | 2 | 1 | 1.4 | 1.2 | 1.2 |
| Codeine | 2 | 1.8 | 10.2 | 6.0 | 6.0 |
| Others | |||||
| Methylfenidate | 1 | 21.5 | 21.5 | / | / |
| Rilatinic acid | 2 | >300 | >300 | >300 | >300 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wille, S.M.R.; Van Dijck, K.; Van Assche, A.; Di Fazio, V.; Ramiréz-Fernandéz, M.d.M.; Vanvooren, V.; Samyn, N. The Interest of a Systematic Toxicological Analysis Combined with Forensic Advice to Improve the Judicial Investigation and Final Judgment in Drug Facilitated Sexual Assault Cases. Pharmaceuticals 2021, 14, 432. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14050432
Wille SMR, Van Dijck K, Van Assche A, Di Fazio V, Ramiréz-Fernandéz MdM, Vanvooren V, Samyn N. The Interest of a Systematic Toxicological Analysis Combined with Forensic Advice to Improve the Judicial Investigation and Final Judgment in Drug Facilitated Sexual Assault Cases. Pharmaceuticals. 2021; 14(5):432. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14050432
Chicago/Turabian StyleWille, Sarah M. R., Karolien Van Dijck, Antje Van Assche, Vincent Di Fazio, Maria del Mar Ramiréz-Fernandéz, Vanessa Vanvooren, and Nele Samyn. 2021. "The Interest of a Systematic Toxicological Analysis Combined with Forensic Advice to Improve the Judicial Investigation and Final Judgment in Drug Facilitated Sexual Assault Cases" Pharmaceuticals 14, no. 5: 432. https://0-doi-org.brum.beds.ac.uk/10.3390/ph14050432