Improved Morphine-Loaded Hydrogels for Wound-Related Pain Relief
Abstract
:1. Introduction
2. Material and Methods
2.1. Materials
2.2. Methods
2.2.1. Identification of QTPP and CQAs
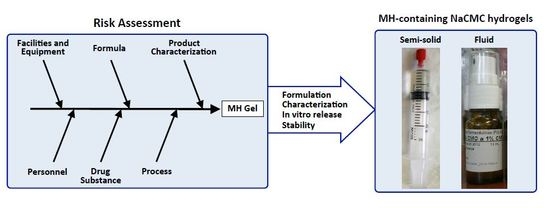
2.2.2. Risk Analysis of CQAs
2.2.3. Hydrogels’ Preparation
2.2.4. Physicochemical Characterisation
2.2.5. Morphine Quantification
2.2.6. Sterility Testing
2.2.7. Efficacy of Antimicrobial Preservation
2.2.8. In Vitro Release Studies
- 1)
- Zero order kineticsWhere, K0 is the zero order release constant
- 2)
- First order kineticsWhere, K1 is the first order release constant.
- 3)
- Higuchi modelWhere, KH is the Higuchi release constant.
- 4)
- Korsmeyer-Peppas modelWhere, KKP is the release constant incorporating the structural and geometric characteristics of the drug-dosage form, and n is the diffusional exponent indicating the drug-release mechanism.
2.2.9. Stability Studies
2.2.10. Statistical analysis
3. Results and discussion
3.1. Risk Assessment
3.2. Characterisation
3.3. In Vitro Release
3.4. Stability
4. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Maida, V. Wound management in patients with advanced illness. Curr. Opin. Support Palliat. Care 2013, 7, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Zeppetella, G.; Paul, J.; Ribeiro, M.D. Analgesic efficacy of morphine applied topically to painful ulcers. J. Pain Symptom. Manage. 2003, 25, 555–558. [Google Scholar] [CrossRef]
- Argoff, C.E. Topical analgesics in the management of acute and chronic pain. Mayo. Clin. Proc. 2013, 88, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Langemo, D.; Haesler, E.; Naylor, W.; Tippett, A.; Young, T. Evidence-based guidelines for pressure ulcer management at the end of life. Int. J. Palliat. Nurs. 2015, 21, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Peppin, J.F.; Albrecht, P.J.; Argoff, C.; Gustorff, B.; Pappagallo, M.; Rice, F.L.; Wallace, M.S. Skin matters: A review of topical treatments for chronic pain. Part one: Skin physiology and delivery systems. Pain Ther. 2015, 4, 17–32. [Google Scholar] [CrossRef] [PubMed]
- Zur, E. Topical treatment of neuropathic pain using compounded medications. Clin. J. Pain 2014, 30, 73–91. [Google Scholar] [CrossRef] [PubMed]
- DiScala, S.; Basri, D.; Vartan, C.M.; Silverman, M.A. Use of topical morphine to relieve painful pressure ulcers. Consult. Pharm. 2018, 33, 215–221. [Google Scholar] [CrossRef]
- Miyazaki, T.; Satou, S.; Ohno, T.; Yoshida, A.; Nishimura, K. Topical morphine gel for pain management in head and neck cancer patients. Auris. Nasus. Larynx. 2014, 41, 496–498. [Google Scholar] [CrossRef]
- Twillman, R.K.; Long, T.D.; Cathers, T.A.; Mueller, D.W. Treatment of painful skin ulcers with topical opioids. J. Pain Symptom. Manage. 1999, 17, 288–292. [Google Scholar] [CrossRef]
- LeBon, B.; Zeppetella, G.; Higginson, I.J. Effectiveness of topical administration of opioids in palliative care: A systematic review. J. Pain Symptom. Manage. 2009, 37, 913–917. [Google Scholar] [CrossRef]
- Bigliardi, P.L.; Tobin, D.J.; Gaveriaux-Ruff, C.; Bigliardi-Qi, M. Opioids and the skin—where do we stand? Exp. Dermatol. 2009, 18, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Farley, P. Should topical opioid analgesics be regarded as effective and safe when applied to chronic cutaneous lesions? J. Pharm. Pharmacol. 2011, 63, 747–756. [Google Scholar] [CrossRef]
- Boateng, J.; Cantazano, O. Advanced therapeutic dressings for effective wound healing—a review. J. Pharm. Sci. 2015, 104, 3653–3680. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, M.D.; Joel, S.P.; Zeppetella, G. The bioavailability of morphine applied topically to cutaneous ulcers. J. Pain Symptom. Manage. 2004, 27, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Zeppetella, G.; Ribeiro, M.D. Morphine in intrasite gel applied topically to painful ulcers. J. Pain. Symptom. Manage. 2005, 29, 118–119. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.W.; Ramli, N.A. Carboxymethylcellulose film for bacterial wound infection control and healing. Carbohydr. Polym. 2014, 112, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Zeppetella, G.; Joel, S.P.; Ribeiro, M.D. Stability of morphine sulphate and diamorphine hydrochloride in intrasite gel. Palliat. Med. 2005, 19, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Jansen, M.M.P.M.; Verzijl, J.M.; Burger, D.M.; Hekster, Y.A. Controlled release of morphine from a poloxamer 407 gel. Int. J. Pharm. 2013, 452, 266–269. [Google Scholar] [CrossRef]
- Jeng, J.; Gibran, N.; Peck, M. Burn care in disaster and other austere settings. Surg. Clin. North Am. 2014, 94, 893–907. [Google Scholar] [CrossRef]
- ICH Q8(R2). Pharmaceutical Development. ICH Harmonized Tripartite Guideline. 2009. Available online: https://www.ich.org/products/guidelines/quality/quality-single/article/pharmaceutical-development.html (accessed on 26 November 2018).
- ICH Q1A(R2). Stability testing of new Drugs and Products. ICH Harmonized Tripartite Guideline. 2003. Available online: https://www.ich.org/products/guidelines/quality/quality-single/article/stability-testing-of-new-drug-substances-and-products.html (accessed on 26 November 2018).
- Gethin, G. The significance of surface pH in chronic wounds. Wounds UK 2007, 3, 52–56. [Google Scholar]
- The United States Pharmacopeial Convention. The United States Pharmacopeia (USP 41-NF36); The United States Pharmacopeial Convention: Rockville, MD, USA, 2017. [Google Scholar]
- European Directorate for the Quality of Medicines. European Pharmacopoeia (Ph. Eur.). 9th Ed. European Directorate for the Quality of Medicines; Council of Europe: Strasbourg, France, 2016. [Google Scholar]
- ICH Q9. Quality Risk Management. ICH Harmonized Tripartite Guideline. 2005. Available online: https://www.ich.org/products/guidelines/quality/quality-single/article/quality-risk-management.html (accessed on 26 November 2018).
- Santos, A.M.C.; Doria, M.S.; Meirinhos-Soares, L.; Almeida, A.J.; Menezes, J.C. A QRM discussion of microbial contamination of non-sterile drug products, using FDA’s and EMA’s warning-letters between 2008 and 2016. PDA J. Pharm. Sci. Technol. 2018, 72, 62–72. [Google Scholar] [CrossRef]
- PIC/S. Guide to good practices for the preparation of medicinal products in healthcare establishments. Pharmaceutical Inspection Convention—Pharmaceutical Inspection Co-operation Scheme. 2014. Available online: https://www.gmp-compliance.org/guidelines/gmp-guideline/pic-s-guide-to-good-manufacturing-practices-of-preparation-of-medicinal-products-in-healthcare-establishments-pic-s-pe-010-4 (accessed on 18 December 2018).
- Muhtadi, F.J. Analytical profile of morphine. In Analytical Profiles of Drug Substances; Florey, K., Ed.; Academic Press: San Diego, CA, USA, 1988; Volume 17, pp. 259–366. [Google Scholar]
- ICH Q2(R1). Validation of analytical procedures. ICH Harmonized Tripartite Guideline. 2005. Available online: https://www.ich.org/products/guidelines/quality/quality-single/article/analytical-procedure-development-and-revision-of-q2r1-analytical-validation-copy-1.html (accessed on 26 November 2018).
- Zhang, Y.; Huo, M.; Zhou, J.; Zou, A.; Li, A.; Yao, C.; Xie, S. DDSolver: An add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 2010, 12, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Costa, P.; Sousa Lobo, J.M. Modeling and comparison of dissolution profiles. Eur. J. Pharm. Sci. 2001, 13, 123–133. [Google Scholar] [CrossRef]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Khan, K.A. The concept of dissolution efficiency. J. Pharm. Pharmacol. 1975, 27, 48–49. [Google Scholar] [CrossRef] [PubMed]
- Agren, M.S. An amorphous hydrogel enhances epithelialisation of wounds. Acta Derm. Venereol. 1998, 78, 119–122. [Google Scholar]
- Ramli, N.A.; Wong, T.W. Sodium carboxymethylcellulose scaffolds and their physicochemical effects on partial thickness wound healing. Int. J. Pharm. 2011, 403, 73–82. [Google Scholar] [CrossRef]
- Hooton, J.C. Carboxymethylcellulose sodium. Pharmaceutical Excipients. Medicines Complete. 2018. Available online: https://www.medicinescomplete.com/#/content/excipients/1001935347 (accessed on 18 December 2018).
- Jones, E.M.; Cochrane, C.A.; Percival, S.L. The effect of pH on the extracellular matrix and biofilms. Adv. Wound Care (New Rochelle) 2015, 4, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Lönnqvist, S.; Emanuelsson, P.; Kratz, G. Influence of acidic pH on keratinocyte function and re-epithelialisation of human in vitro wounds. J. Plast. Surg. Hand Surg. 2015, 49, 346–352. [Google Scholar] [CrossRef]
- Salgado, A.C.; Rosa, M.L.; Duarte, M.A.; Almeida, A.J. Stability of spironolactone in an extemporaneously prepared aqueous suspension: Importance of microbiological quality of compounded paediatric formulations. Eur. J. Hosp. Pharm. Sci. 2005, 11, 68–73. [Google Scholar]
- Vermeire, A.; Remon, J.P. Stability and compatibility of morphine. Int J Pharm 1999, 187, 17–51. [Google Scholar] [CrossRef]
- Raghavan, S.L.; Trividic, A.; Davis, A.F.; Hadgraft, J. Effect of cellulose polymers on supersaturation and in vitro membrane transport of hydrocortisone acetate. Int. J. Pharm. 2000, 193, 231–237. [Google Scholar] [CrossRef]
- Salgado, A.; Raposo, S.; Marto, J.; Silva, A.N.; Simões, S.; Ribeiro, H.M. Mometasone furoate hydrogel for scalp use: In vitro and in vivo evaluation. Pharm. Dev. Technol. 2014, 19, 618–622. [Google Scholar] [CrossRef]
- Mazák, K.; Hosztafi, S.; Rácz, Á.; Noszál, B. Structural and physicochemical profiling of morphine and related compounds of therapeutic interest. Mini. Rev. Med. Chem. 2009, 9, 984–995. [Google Scholar] [CrossRef] [PubMed]
- Strong, M.L.; Schaaf, L.J.; Pankaskie, M.C.; Robinson, D.H. Shelf-lives and factors affecting the stability of morphine sulphate and meperidine (pethidine) hydrochloride in plastic syringes for use in patient-controlled analgesic devices. J. Clin. Pharm. Ther. 1994, 19, 361–369. [Google Scholar] [CrossRef] [PubMed]






| QTPP Element | Target | Reference |
|---|---|---|
| Route of Administration | Topical in wounds | [9] |
| Strength | Semi-solid gel: 0.125% MH; Fluid gel: 1.0% MH | According to the characteristics of the dose metering device |
| Dosage Form | Hydrogel | [2] |
| Drug Product Critical Quality Attributes [19] | Aspect: colourless to yellowish transparent, homogeneous gel pH: slightly acidic: 5.5–6.5 Viscosity: Semi-solid gel: 50 ± 20 × 103 Pa·s; Fluid gel: 25 ± 10 Pa·s Assay: 90–110% Antimicrobial preservation Sterility | [22] ≤ viscosity of commercial hydrogels (IntraSite® Gel Varihesive® Hydrogel) USP<795> [23] Ph. Eur. 5.1.3 [24] Ph. Eur. 2.6.1; USP<797> [23,24] |
| Stability | Beyond-use date ≥28 days at 5 ± 3 °C | [21] |
| Excipients | Concentration (% w/w) | Quality Standard | Pharmaceutical Function | |
|---|---|---|---|---|
| F1 | F2 | |||
| NaCMC | 3.0* | 0.5 * | Ph. Eur. | Polymer |
| Glycerol | 5.0 | 5.0 | Ph. Eur. | Humectant |
| Metylparaben | 0.10 | 0.10 | Ph. Eur. | Preservative |
| Propylparaben | 0.010 | 0.010 | Ph. Eur. | Preservative |
| Water for injections | qs to 100 | qs to 100 | Ph. Eur. | Solvent |
| Parameter | NaCMC Hydrogels | Formulations | ||
|---|---|---|---|---|
| F1 | F2 | F1-MH | F2-MH | |
| Aspect | Colourless, transparent and homogeneous | Colourless, transparent and homogeneous | Yellowish, transparent and homogeneous | Slightly yellowish, transparent and homogeneous |
| MH (%) | - | - | 0.125 | 1.0 |
| pH | 6.36 ± 0.02 | 6.22 ± 0.04 | 6.37 ± 0.05 | 5.64 ± 0.05 |
| Viscosity (Pa s−1) | 61.3 × 103 ± 1.90 × 103 | 113.3 ± 2.3 | 50.1 × 103 ± 3.9 × 103 | 20.6 ± 8.1 |
| Formulation | Model | K | R2adjusted | AIC |
|---|---|---|---|---|
| F1-MH | Zero order | 3.71 ± 0.36 | 0.619 ± 0.095 | 28.19 ± 1.77 |
| First order | 0.04 ± 0.00 | 0.682 ± 0.084 | 27.07 ± 1.79 | |
| Higuchi | 7.84 ± 0.78 | 0.946 ± 0.023 | 15.78 ± 3.06 | |
| Korsmeyer-Peppas | 8.65 ± 1.06 | 0.939 ± 0.041 | 16.13 ± 4.39 | |
| n - 0.428 ± 0.08 | ||||
| F2-MH | Zero order | 7.35 ± 0.24 | 0.878 ± 0.076 | 30.39 ± 2.89 |
| First order | 0.09 ± 0.00 | 0.908 ± 0.063 | 28.78 ± 2.78 | |
| Higuchi | 14.33 ± 0.84 | 0.923 ± 0.039 | 27.39 ± 3.22 | |
| Korsmeyer-Peppas | 14.31 ± 1.57 | 0.916 ± 0.039 | 28.81 ± 11.04 | |
| n - 0.48 ± 0.12 |
| Time (days) | F1-MH | F2-MH | ||||
|---|---|---|---|---|---|---|
| Recovery of morphine (%) | pH | Viscosity (× 103 Pa·s) | Recovery of morphine (%) | pH | Viscosity (Pa·s) | |
| Batches stored in the fridge (5 ± 3 °C) | ||||||
| 0 | 100.4 ± 1.3 | 6.37 ± 0.05 | 50.1 ± 3.9 | 102.5 ± 0.1 | 5.64 ± 0.05 | 20.6 ± 8.1 |
| 7 | 101.7 ± 0.3 | 6.38 ± 0.07 | 47.7 ± 3.4 | 101.9 ± 0.1 | 5.59 ± 0.03 | 22.2 ± 9.4 |
| 14 | 104.0 ± 1.2 | 6.28 ± 0.03 | 47.1 ± 3.0 | 100.9 ± 0.9 | 5.64 ± 0.03 | 16.1 ± 3.3 |
| 30 | 104.9 ± 3.2 | 6.38 ± 0.04 | 48.2 ± 3.2 | 102.1 ± 0.2 | 5.67 ± 0.06 | 16.1 ± 4.2 |
| 60 | 104.7 ± 0.1 | 6.59 ± 0.03 | 41.2 ± 1.6 | 102.6 ± 1.6 | 5.61 ± 0.04 | 17.2 ± 2.6 |
| Batches stored at room temperature (22 ± 3 °C) | ||||||
| 0 | 100.4 ± 1.3 | 6.37 ± 0.05 | 50.1 ± 3.9 | 102.5 ± 0.1 | 5.64 ± 0.05 | 20.6 ± 8.1 |
| 7 | 105.0 ± 0.7 | 6.32 ± 0.04 | 46.7 ± 4.7 | 101.6 ± 0.9 | 5.62 ± 0.11 | 25.0 ± 6.6 |
| 14 | 108.7 ± 4.3 | 6.37 ± 0.09 | 45.0 ± 3.7 | 101.0 ± 0.5 | 5.62 ± 0.02 | 16.7 ± 3.5 |
| 30 | 106.4 ± 0.2 | 6.39 ± 0.05 | 46.8 ± 6.7 | 101.3 ± 0.7 | 5.68 ± 0.05 | 17.8 ± 3.6 |
| 60 | 102.6 ± 2.7 | 6.57 ± 0.03 | 33.6 ± 2.0 | 103.6 ± 0.6 | 5.51 ± 0.03 | 17.8 ± 5.7 |
| Batches stored at accelerated conditions (40 ± 2 °C/75% Relative Humidity) | ||||||
| 0 | 100.4 ± 1.3 | 6.37 ± 0.05 | 50.1 ± 3.9 | 102.5 ± 0.1 | 5.64 ± 0.05 | 20.6 ± 8.1 |
| 7 | 104.1 ± 1.9 | 6.30 ± 0.03 | 38.1 ± 2.5 | 101.0 ± 1.1 | 5.54 ± 0.03 | 17.2 ± 4.4 |
| 14 | 101.3 ± 2.0 | 6.29 ± 0.12 | 32.4 ± 1.4 | 102.7 ± 1.3 | 5.55 ± 0.02 | 22.2 ± 5.7 |
| 30 | 102.0 ± 0.8 | 6.34 ± 0.06 | 30.0 ± 1.7 | 104.0 ± 1.9 | 5.50 ± 0.04 | 15.0 ± 4.3 |
| 60 | 101.6 ± 1.3 | 6.39 ± 0.05 | 11.3 ± 0.6 | 105.5 ± 1.5 | 5.33 ± 0.03 | 11.1 ± 2.2 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mateus, D.; Marto, J.; Trindade, P.; Gonçalves, H.; Salgado, A.; Machado, P.; Melo-Gouveia, A.; Ribeiro, H.M.; Almeida, A.J. Improved Morphine-Loaded Hydrogels for Wound-Related Pain Relief. Pharmaceutics 2019, 11, 76. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11020076
Mateus D, Marto J, Trindade P, Gonçalves H, Salgado A, Machado P, Melo-Gouveia A, Ribeiro HM, Almeida AJ. Improved Morphine-Loaded Hydrogels for Wound-Related Pain Relief. Pharmaceutics. 2019; 11(2):76. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11020076
Chicago/Turabian StyleMateus, Dinis, Joana Marto, Patrícia Trindade, Humberto Gonçalves, Ana Salgado, Paula Machado, António Melo-Gouveia, Helena M. Ribeiro, and António J. Almeida. 2019. "Improved Morphine-Loaded Hydrogels for Wound-Related Pain Relief" Pharmaceutics 11, no. 2: 76. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11020076