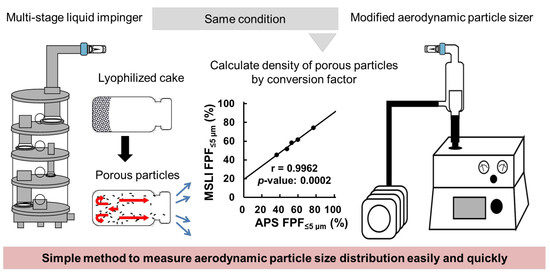
Simple Method to Measure the Aerodynamic Size Distribution of Porous Particles Generated on Lyophilizate for Dry Powder Inhalation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Freeze-Dried Cake
2.3. Particle Size Distribution
2.3.1. Geometric Particle Size Distribution by Laser Diffraction Measurement (LD)
2.3.2. Aerodynamic Particle Size Distribution by Aerodynamic Particle Sizer (APS) Spectrometer
2.3.3. Aerodynamic Particle Size Distribution by MSLI
2.4. Statistical Analysis
3. Results
3.1. Correlation between MSLI and LD Measurement
3.2. Correlation between MSLI and APS Measurement
4. Discussion
4.1. Correlation between MSLI and LD Measurement
4.2. Correlation between MSLI and APS Measurement
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Patton, J.S.; Byron, P.R. Inhaling medicines: Delivering drugs to the body through the lungs. Nat. Rev. Drug Discov. 2007, 6, 67–74. [Google Scholar] [CrossRef]
- Sahane, S.; Nikhar, A.; Bhaskaran, S.; Mundhada, D. Dry powder inhaler: An advance technique for pulmonary drug delivery system. Int. J. Pharm. Chem. Sci. 2012, 1, 1376–1383. [Google Scholar]
- Pilcer, G.; Amighi, K. Formulation strategy and use of excipients in pulmonary drug delivery. Int. J. Pharm. 2010, 392, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Scheuch, G.; Siekmeier, R. Novel approaches to enhance pulmonary delivery of proteins and peptides. J. Physiol. Pharmacol. 2007, 58 (Suppl. 5), 615–625. [Google Scholar]
- De Boer, A.H.; Gjaltema, D.; Hagedoorn, P.; Frijlink, H.W. Characterization of inhalation aerosols: A critical evaluation of cascade impactor analysis and laser diffraction technique. Int. J. Pharm. 2002, 249, 219–231. [Google Scholar] [CrossRef]
- Edwards, D.A. Delivery of biological agents by aerosols. AIChE J. 2002, 48, 2–6. [Google Scholar] [CrossRef]
- Ogienko, A.G.; Bogdanova, E.G.; Trofimov, N.A.; Myz, S.A.; Ogienko, A.A.; Kolesov, B.A.; Yunoshev, A.S.; Zubikov, N.V.; Manakov, A.Y.; Boldyrev, V.V.; et al. Large porous particles for respiratory drug delivery. Glycine-based formulations. Eur. J. Pharm. Sci. 2017, 110, 148–156. [Google Scholar] [CrossRef]
- Pham, D.D.; Fattal, E.; Ghermani, N.E.; Guiblin, N.; Tsapis, N. Formulation of pyrazinamide-loaded large porous particles for the pulmonary route: Avoiding crystal growth using excipients. Int. J. Pharm. 2013, 454, 668–677. [Google Scholar] [CrossRef] [PubMed]
- Edwards, D.A.; Dunbar, C. Bioengineering of therapeutic aerosols. Annu. Rev. Biomed. Eng. 2002, 4, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Kadota, K.; Yanagawa, Y.; Tachikawa, T.; Deki, Y.; Uchiyama, H.; Shirakawa, Y.; Tozuka, Y. Development of porous particles using dextran as an excipient for enhanced deep lung delivery of rifampicin. Int. J. Pharm. 2019, 555, 280–290. [Google Scholar] [CrossRef]
- Chvatal, A.; Ambrus, R.; Party, P.; Katona, G.; Jójárt-Laczkovich, O.; Szabó-Révész, P.; Fattal, E.; Tsapis, N. Formulation and comparison of spray dried non-porous and large porous particles containing meloxicam for pulmonary drug delivery. Int. J. Pharm. 2019, 559, 68–75. [Google Scholar] [CrossRef] [Green Version]
- Alsmadi, M.M.; Obaidat, R.M.; Alnaief, M.; Albiss, B.A.; Hailat, N. Development, in vitro characterization, and in vivo toxicity evaluation of chitosan-alginate nanoporous carriers loaded with cisplatin for lung cancer treatment. AAPS Pharm. Sci. Tech. 2020, 21, 191. [Google Scholar] [CrossRef]
- Edwards, D.A.; Hanes, J.; Caponetti, G.; Hrkach, J.; Ben-Jebria, A.; Eskew, M.L.; Mintzes, J.; Deaver, D.; Lotan, N.; Langer, R. Large porous particles for pulmonary drug delivery. Science 1997, 276, 1868–1871. [Google Scholar] [CrossRef] [Green Version]
- Edwards, D.A.; Ben-Jebria, A.; Langer, R. Recent advances in pulmonary drug delivery using large, porous inhaled particles. J. Appl. Physiol. 1998, 85, 379–385. [Google Scholar] [CrossRef]
- Yang, M.Y.; Chan, J.G.Y.; Chan, H.-K. Pulmonary drug delivery by powder aerosols. J. Control. Release 2014, 193, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Telko, M.J.; Hickey, A.J. Dry powder inhaler formulation. Respir. Care. 2005, 50, 1209–1227. [Google Scholar] [PubMed]
- Weers, J.G.; Miller, D.P. Formulation design of dry powders for inhalation. J. Pharm. Sci. 2015, 104, 3259–3288. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Kharb, V.; Punjab, G.M. Optimizing drug delivery systems using systematic “Design of Experiments.” Part II: Retrospect and prospects. Ther. Drug Carr. Syst. 2005, 22, 215–293. [Google Scholar] [CrossRef]
- Awotwe-Otoo, D.; Agarabi, C.; Wu, G.K.; Casey, E.; Read, E.; Lute, S.; Brorson, K.A.; Khan, M.A.; Shah, R.B. Quality by design: Impact of formulation variables and their interactions on quality attributes of a lyophilized monoclonal antibody. Int. J. Pharm. 2012, 438, 167–175. [Google Scholar] [CrossRef]
- Wang, H.; Liu, M.; Du, S. Optimization of madecassoside liposomes using response surface methodology and evaluation of its stability. Int. J. Pharm. 2014, 473, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Shekunov, B.Y.; Chattopadhyay, P.; Tong, H.H.Y.; Chow, A.H.L. Particle size analysis in pharmaceutics: Principles, methods and applications. Pharm. Res. 2007, 24, 203–227. [Google Scholar] [CrossRef]
- Mitchell, J.; Bauer, R.; Lyapustina, S.; Tougas, T.; Glaab, V. Non-impactor-based methods for sizing of aerosols emitted from orally inhaled and nasal drug products (OINDPs). AAPS Pharm. Sci. Tech. 2011, 12, 965. [Google Scholar] [CrossRef] [Green Version]
- Heitbrink, W.A.; Baron, P.A.; Willeke, K. Coincidence in time-of-flight aerosol spectrometers: Phantom particle creation. Aerosol Sci. Technol. 1991, 14, 112–126. [Google Scholar] [CrossRef]
- Mitchell, J.P.; Nagel, M.W. Particle size analysis of aerosols from medicinal inhalers. KONA Powder Part. J. 2004, 22, 32–65. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.-C.; John, W. Particle density correction for the aerodynamic particle sizer. Aerosol Sci. Technol. 1987, 6, 191–198. [Google Scholar] [CrossRef]
- Ananth, G.; Wilson, J.C. Theoretical analysis of the performance of the TSI aerodynamic particle sizer the effect of density on response. Aerosol Sci. Technol. 1988, 9, 189–199. [Google Scholar] [CrossRef]
- Yamashita, C.; Ibaragi, S.; Fukunaga, Y.; Akagi, A. Composition, Vessel, Dry Powder Inhalation System, and Related Methods for Transpulmonary Administration. U.S. Patent 7448379, 11 November 2008. [Google Scholar]
- Yamashita, C. Development of Otsuka dry powder inhalation system using technology of freeze-drying. Drug Deliv. Syst. 2009, 24, 468–476. [Google Scholar] [CrossRef]
- Yamashita, C. Low flow rate-dependent dry powder inhalation system using freeze-dried cake. J. Pharm. Sci. Technol. Jpn. 2012, 72, 111–116. [Google Scholar] [CrossRef]
- Claus, S.; Schoenbrodt, T.; Weiler, C.; Friess, W. Novel dry powder inhalation system based on dispersion of lyophilisates. Eur. J. Pharm. Sci. 2011, 43, 32–40. [Google Scholar] [CrossRef] [Green Version]
- Claus, S.; Weiler, C.; Schiewe, J.; Friess, W. Optimization of the fine particle fraction of a lyophilized lysozyme formulation for dry powder inhalation. Pharm. Res. 2013, 30, 1698–1713. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Horiguchi, M.; Ozawa, C.; Akita, T.; Hirota, K.; Shudo, K.; Terada, H.; Makino, K.; Kubo, H.; Yamashita, C. Pulmonary administration of Am80 regenerates collapsed alveoli. J. Control. Release 2014, 196, 154–160. [Google Scholar] [CrossRef]
- Sakai, H.; Horiguchi, M.; Akita, T.; Ozawa, C.; Hirokawa, M.; Oiso, Y.; Kumagai, H.; Takeda, Y.; Tachibana, I.; Maeda, N.; et al. Effect of 4-[(5,6,7,8-tetrahydro-5,5,8,8-tetramethyl-2-naphthalenyl) carbamoyl] benzoic acid (Am80) on alveolar regeneration in adiponectin deficient-mice showing a chronic obstructive pulmonary disease-like pathophysiology. J. Pharmacol. Exp. Ther. 2017, 361, 501–505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunber, C.A.; Hickey, A.J.; Holzner, P. Dispersion and characterization of pharmaceutical dry powder aerosols. KONA Powder Part. J. 1998, 16, 7–45. [Google Scholar] [CrossRef] [Green Version]
- Pilcer, G.; Vanderbist, F.; Amighi, K. Correlations between cascade impactor analysis and laser diffraction techniques for the determination of the particle size of aerosolised powder formulations. Int. J. Pharm. 2008, 358, 75–81. [Google Scholar] [CrossRef]
- Patel, S.M.; Nail, S.L.; Pikal, M.J.; Geidobler, R.; Winter, G.; Hawe, A.; Davagnino, J.; Rambhatla Gupta, S. Lyophilized drug product cake appearance: What is acceptable? J. Pharm. Sci. 2017, 106, 1706–1721. [Google Scholar] [CrossRef] [PubMed]
- Ullrich, S.; Seyferth, S.; Lee, G. Measurement of shrinkage and cracking in lyophilized amorphous cakes. Part I: Final-product assessment. J. Pharm. Sci. 2015, 104, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Tsapis, N.; Bennett, D.; Jackson, B.; Weitz, D.A.; Edwards, D.A. Trojan particles: Large porous carriers of nanoparticles for drug delivery. Proc. Natl. Acad. Sci. USA 2002, 99, 12001–12005. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, J.P.; Nagel, M. Time-of-flight aerosol analyzers: Their use and limitations for the measurement of medical aerosols. J. Aerosol Med. 1999, 12, 217–240. [Google Scholar] [CrossRef]
- Lawrence, M.; Jiang, Y. Porosity, pore size distribution, micro-structure. In Bio-Aggregates Based Building Materials: State-of-the-Art Report of the RILEM Technical Committee 236-BBM; Amziane, S., Collet, F., Eds.; RILEM State-of-the-Art Reports; Springer: Dordrecht, The Netherlands, 2017; pp. 39–71. ISBN 978-94-024-1031-0. [Google Scholar]
- Markl, D.; Strobel, A.; Schlossnikl, R.; Bøtker, J.; Bawuah, P.; Ridgway, C.; Rantanen, J.; Rades, T.; Gane, P.; Peiponen, K.-E.; et al. Characterisation of pore structures of pharmaceutical tablets: A review. Int. J. Pharm. 2018, 538, 188–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamashita, C. The present state and future of dry powder inhalation system. Drug Deliv. Syst. 2006, 21, 417–425. [Google Scholar] [CrossRef] [Green Version]







| Drug or Compound | MMAD (µm) | D50 (µm) | Particle Density (g/cm3) |
|---|---|---|---|
| hGhrelin | 4.85 | 4.01 | 1.4628 |
| VB3 | 4.19 | 5.95 | 0.4959 |
| VB12 | 3.93 | 4.14 | 0.9011 |
| Am80 | 2.98 | 3.55 | 0.7047 |
| Drug or Compound | Density at Prepared Solution | Particle Density on Inhalation (g/cm3) |
|---|---|---|
| hGhrelin | 0.00120 | 0.00450 |
| VB3 | 0.00120 | 0.00450 |
| VB12 | 0.00140 | 0.00525 |
| Am80 | 0.00040 | 0.00150 |
| Placebo (Phe 0.2 mg/vial) | 0.00040 | 0.00150 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyamoto, K.; Taga, H.; Akita, T.; Yamashita, C. Simple Method to Measure the Aerodynamic Size Distribution of Porous Particles Generated on Lyophilizate for Dry Powder Inhalation. Pharmaceutics 2020, 12, 976. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12100976
Miyamoto K, Taga H, Akita T, Yamashita C. Simple Method to Measure the Aerodynamic Size Distribution of Porous Particles Generated on Lyophilizate for Dry Powder Inhalation. Pharmaceutics. 2020; 12(10):976. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12100976
Chicago/Turabian StyleMiyamoto, Kahori, Hiroaki Taga, Tomomi Akita, and Chikamasa Yamashita. 2020. "Simple Method to Measure the Aerodynamic Size Distribution of Porous Particles Generated on Lyophilizate for Dry Powder Inhalation" Pharmaceutics 12, no. 10: 976. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics12100976