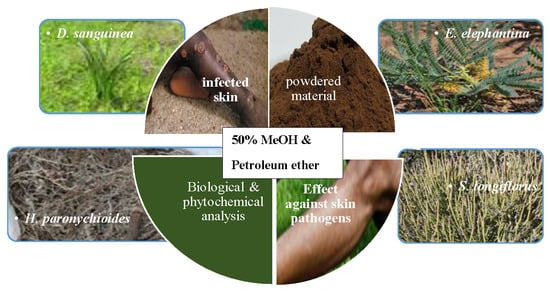
Antimicrobial Activity, Antioxidant Potential, Cytotoxicity and Phytochemical Profiling of Four Plants Locally Used against Skin Diseases
Abstract
:1. Introduction
2. Results and Discussion
2.1. Antibacterial Activity
2.2. Antifungal Activity
2.3. Antioxidant Activity
2.3.1. 2,2-Diphenyl-1-picryl Hydrazyl (DPPH) Radical Scavenging Activity
2.3.2. β-Carotene-Linoleic Acid Assay
2.4. Cytotoxicity Assay
2.5. Total Phenolic and Flavonoid Contents
2.6. Gas Chromatography—Mass Spectrometry Analysis
3. Materials and Methods
3.1. Plant Material Collection and Extraction
3.2. Antimicrobial Assay
3.2.1. Microorganisms and Culture Media
3.2.2. Antibacterial Assay
3.2.3. Antifungal Assay
3.3. Antioxidant Assay
3.3.1. 2,2-Diphenyl-1-picryhydrazyl (DPPH) Free Radical Scavenging (RSA) Assay
3.3.2. β-Carotene-Linoleic Acid Assay
3.4. Cytotoxicity Assay
3.5. Phytochemical Analysis
3.5.1. Determination of Total Phenolic Content
3.5.2. Determination of Flavonoid Content
3.5.3. Gas Chromatography–Mass Spectroscopy (GC–MS) Analysis
3.6. Data Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- De Wet, H.; Nciki, S.; van Vuuren, S.F. Medicinal Plants Used for the Treatment of Various Skin Disorders by a Rural Community in Northern Maputaland, South Africa. J. Ethnobiol. Ethnomed. 2013, 9, 51. [Google Scholar] [CrossRef] [PubMed]
- Hay, R.J.; Johns, N.E.; Williams, H.C.; Bolliger, I.W.; Dellavalle, R.P.; Margolis, D.J.; Marks, R.; Naldi, L.; Weinstock, M.A.; Wulf, S.K. The Global Burden of Skin Disease in 2010: An Analysis of the Prevalence and Impact of Skin Conditions. J. Investig. Dermatol. 2014, 134, 1527–1534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez, A.D.; Mathers, D.C.; Ezzati, M.; Jamison, D.T.; Murray, C.J.L. Global and Regional Burden of Disease and Risk Factors, 2001: Systematic Analysis of Population Health Data. Lancet 2006, 367, 1747–1757. [Google Scholar] [CrossRef]
- Otang, W.M.; Afolayan, A.J. Antimicrobial and Antioxidant Efficacy of Citrus Limon, L. Peel Extracts Used for Skin Diseases by Xhosa Tribe of Amathole District, Eastern Cape, South Africa. S. Afr. J. Bot. 2016, 102, 46–49. [Google Scholar] [CrossRef]
- Ördögh, L.; Galgóczy, G.; Krisch, J.; Papp, T.; Vágvölgyi, C. Antioxidant and Antimicrobial Activities of Fruit Juices and Pomace Extracts against Acne-Inducing Bacteria. Acta Biol. Szeged. 2010, 54, 45–49. [Google Scholar]
- Nesy, E.A.; Mathew, L. Studies on Antimicrobial and Antioxidant Efficacy of Thevetia neriifolia, Juss Leaf Extracts against Human Skin Pathogens. Int. J. Pharm. Sci. Drug Res. 2014, 6, 164–168. [Google Scholar]
- Van Hees, C.; Naafs, B. Common Skin Diseases in Africa: An Illustrated Guide; Total Graphics BV: Houston, TX, USA, 2001. [Google Scholar]
- Grierson, D.S.; Otang, W.M.; Afolayan, A.J. A Review of the Phytochemistry, Botany, Pharmacology and Toxicology of Arctotis arctotoides (Lf) O. Hoffm.(Asteraceae). Afr. J. Tradit. Complement. Altern. Med. 2014, 11, 118–126. [Google Scholar] [CrossRef]
- Otang, W.M.; Grierson, D.S.; Ndip, R.N. Phytochemical Studies and Antioxidant Activity of Two South African Medicinal Plants Traditionally Used for the Management of Opportunistic Fungal Infections in HIV/AIDS Patients. BMC Complement. Altern. Med. 2012, 12, 43. [Google Scholar] [CrossRef]
- Sharma, S.K.; Singh, L.; Singh, S. A Review on Medicinal Plants Having Antioxidant Potential. Ind. J. Res. Phar. Biotechnol. 2013, 1, 404–409. [Google Scholar]
- Varsha, N.; Sodhi, J.S. Some Medicinal Plants with Antioxidant Activity—A Review. Int. J. Pharm. Biol. Sci. 2014, 4, 173–178. [Google Scholar]
- Atanasov, A.G.; Waltenberger, B.; Pferschy-Wenzig, E.; Linder, T.; Wawrosch, C.; Uhrin, P.; Temml, V.; Wang, L.; Schwaiger, S.; Heiss, E.H.; et al. Discovery and Resupply of Pharmacologically Active Plant-Derived Natural Products: A Review. Biotechnol. Adv. 2015, 33, 1582–1614. [Google Scholar] [CrossRef] [PubMed]
- Lall, N.; Kishore, N. Are Plants Used for Skin Care in South Africa Fully Explored? J. Ethnopharmacol. 2014, 153, 61–84. [Google Scholar] [CrossRef] [PubMed]
- Mabona, U.; van Vuuren, S.F. Southern African Medicinal Plants Used to Treat Skin Diseases. S. Afr. J. Bot. 2013, 87, 175–193. [Google Scholar] [CrossRef]
- Asong, J.A.; Ndhlovu, P.T.; Khosana, N.S.; Aremu, A.O.; Otang-Mbeng, W. Medicinal Plants Used for Skin-Related Diseases among the Batswanas in Ngaka Modiri Molema District Municipality, South Africa. S. Afr. J. Bot. 2019. [Google Scholar] [CrossRef]
- Bozorgi, M.; Amin, G.; Shekarchi, M.; Rahimi, R. Traditional Medical Uses of Drimia Species in Terms of Phytochemistry, Pharmacology and Toxicology. J. Tradit. Chin. Med. 2017, 37, 124–139. [Google Scholar] [CrossRef]
- Aaku, E.; Office, M.; Dharani, S.P.; Majinda, R.R.T.; Motswaiedi, M.S. Chemical and Antimicrobial Studies on Elephantorrhiza elephantina. Fitoterapia 1998, 69, 464–465. [Google Scholar]
- Mpofu, S.; Tantoh, N.D.; van Vuuren, S.F.; Olivier, D.K.; Krause, R.W.M. Interactive Efficacies of Elephantorrhiza elephantina and Pentanisia prunelloides Extracts and Isolated Compounds against Gastrointestinal Bacteria. S. Afr. J. Bot. 2014, 94, 224–230. [Google Scholar] [CrossRef]
- Sevil, A.; Ahmet, A.; Lutfiye, Y.; Abit, Y. A Comparative Study on Antioxidant and Antimicrobial Activities of four Senecio, L. Species from Turkey. Int. J. Secon. Metab. 2015, 2, 26–36. [Google Scholar]
- Lourens, A.C.U.; Viljoen, A.M.; Van Heerden, F.R. South African Helichrysum Species: A Review of the Traditional Uses, Biological Activity and Phytochemistry. J. Ethnopharmacol. 2008, 119, 630–652. [Google Scholar] [CrossRef]
- Runner, R.T.M.; Roger, D.W.; Peter, G.W. Bufadienolides and Other Constituents of Urginea sanguinea. Planta Med. 1997, 63, 188–190. [Google Scholar]
- Aligiannis, N.; Kalpoutzakis, E.; Mitaku, S.; Chinou, I.B. Composition and Antimicrobial Activity of the Essential Oils of Two Origanum Species. J. Agric. Food Chem. 2001, 49, 4168–4170. [Google Scholar] [CrossRef] [PubMed]
- Katerere, D.R.; Eloff, J.N. Anti-Bacterial and Anti-Oxidant Activity of Hypoxis hemerocallidea (Hypoxidaceae): Can Leaves Be Substituted for Corms as a Conservation Strategy? S. Afr. J. Bot. 2008, 74, 613–616. [Google Scholar] [CrossRef]
- Amoo, S.O.; Ndhlala, A.R.; Finnie, J.F.; Van Staden, J. Antibacterial, Antifungal and Anti-Inflammatory Properties of Burchellia bubalina. S. Afr. J. Bot. 2009, 75, 60–63. [Google Scholar] [CrossRef]
- Tshikalange, T.E.; Meyer, J.J.M.; Hussein, A.A. Antimicrobial Activity, Toxicity and the Isolation of a Bioactive Compound from Plants Used to Treat Sexually Transmitted Diseases. J. Ethnopharmacol. 2005, 96, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Aremu, A.O.; Fawole, O.A.; Chukwujekwu, J.C.; Light, M.E.; Finnie, J.F.; Van Staden, J. In Vitro Antimicrobial, Anthelmintic and Cyclooxygenase-Inhibitory Activities and Phytochemical Analysis of Leucosidea sericea. J. Ethnopharmacol. 2010, 131, 22–27. [Google Scholar] [CrossRef]
- Rabe, T.; van Staden, J. Antibacterial Activity of South African Plants Used for Medicinal Purposes. J. Ethnopharmacol. 1997, 56, 81–87. [Google Scholar] [CrossRef]
- Shale, T.L.; Stirk, W.A.; van Staden, J. Screening of Medicinal Plants Used in Lesotho for Anti-Bacterial and Anti-Inflammatory Activity. J. Ethnopharmacol. 1999, 67, 347–354. [Google Scholar] [CrossRef]
- Mathekga, A.D.M.; Meyer, J.J.M.; Horn, M.M.; Drewes, S.E. An Acylated Phloroglucinol with Antimicrobial Properties from Helichrysum caespititium. Phytochemistry 2000, 53, 93–96. [Google Scholar] [CrossRef]
- Loizou, S.; Lekakis, I.; Chrousos, G.P.; Moutsatsou, P. Beta-Sitosterol Exhibits Anti–Inflammatory Activity in Human Aortic Endothelial Cells. Mol. Nutr. Food Res. 2010, 54, 551–558. [Google Scholar]
- Lopez, S.; Lima, B.; Agüero, M.B.; Lopez, M.L.; Hadad, M.; Zygadlo, J.; Caballero, D.; Stariolo, R.; Suero, E.; Feresin, G.E.; et al. Chemical Composition, Antibacterial and Repellent Activities of Azorella trifurcata, Senecio pogonias, and Senecio oreophyton Essential Oils. Arab. J. Chem. 2018, 11, 181–187. [Google Scholar] [CrossRef]
- Rehab, S.A.; Abeer, E.S.; Mohamed, E.; Dina, A.H. Chemical Profile and Biological Activities of the Aerial Parts of Senecio acaulis (L.F.) Sch.Bip. Pharm. Res. 2018, 10, 130. [Google Scholar]
- Grierson, D.S.; Afolayan, A.J. An Ethnobotanical Study of Plants Used for the Treatment of Wounds in the Eastern Cape, South Africa. J. Ethnopharmacol. 2003, 67, 327–332. [Google Scholar] [CrossRef]
- Ojewole, J.A.O. Antinociceptive, Anti-Inflammatory and Antidiabetic Properties of Hypoxis hemerocallidea Fisch. & C.A. Mey. (Hypoxidaceae) Corm [‘African Potato’] Aqueous Extract in Mice and Rats. J. Ethnopharmacol. 2006, 103, 126–134. [Google Scholar] [PubMed]
- Okem, A.; Kulkarni, M.G.; Van Staden, J. Enhancing Phytoremediation Potential of Pennisetum clandestinum Hochst in Cadmium-Contaminated Soil Using Smoke-Water and Smoke-Isolated Karrikinolide. Int. J. Phytoremed. 2015, 17, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Mathabe, M.C.; Nikolova, R.V.; Lall, N.; Nyazema, N.Z. Antibacterial Activities of Medicinal Plants Used for the Treatment of Diarrhoea in Limpopo Province, South Africa. J. Ethnopharmacol. 2006, 105, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Nyila, M.A.; Leonard, C.M.; Hussein, A.A.; Lall, N. Activity of South African Medicinal Plants against Listeria monocytogenes Biofilms, and Isolation of Active Compounds from Acacia Karroo. S. Afr. J. Bot. 2012, 78, 220–227. [Google Scholar] [CrossRef]
- Baskaran, P.; Singh, S.; Van Staden, J. In Vitro Propagation, Proscillaridin A Production and Antibacterial Activity in Drimia robusta. Plant Cell Tiss. Organ Cult. 2013, 114, 259–267. [Google Scholar] [CrossRef]
- Reichart, P.A. Oral Manifestations in HIV Infection: Fungal and Bacterial Infections, Kaposi’s Sarcoma. Med. Microbiol. Immun. 2003, 192, 165–169. [Google Scholar] [CrossRef]
- Roberto, C.; Evelina, T.; Tumbarello, M.; Morace, G.; De Bernardis, F.; Torosantucci, A.; Antonio, C. Role of Protease Inhibitors in Preventing Recurrent Oral Candidosis in Patients with HIV Infection: A Prospective Case-Control Study. J. Acquired Immune Defic. Syndr. 1999, 21, 20–25. [Google Scholar]
- Tsai, H.; Bobek, L.A. Studies of the Mechanism of Human Salivary Histatin-5 Candidacidal Activity with Histatin-5 Variants and Azole-Sensitive and -Resistant Candida Species. Antimicrob. Agents Chemother. 1997, 41, 2224. [Google Scholar] [CrossRef]
- Hay, R.J. 268—Dermatophytosis (Ringworm) and Other Superficial Mycoses. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 8th ed.; Bennett, J.E., Dolin, R., Blaser, M.J., Eds.; Content Repository Only: Philadelphia, PN, USA, 2015; pp. 2985–2994. [Google Scholar]
- Loizzo, M.R.; Statti, G.A.; Tundis, R.; Conforti, F.; Bonesi, M.; Autelitano, G.; Houghton, P.J.; Miljkovic-Brake, A.; Menichini, F. Antibacterial and Antifungal Activity of Senecio inaequidens DC. and Senecio vulgaris, L. Phytother. Res. 2004, 18, 777–779. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, S.R.; Kameshwari, M.N.S.; Swaminathan, S.; Gupta, M.N. Major Antifungal Activity from the Bulbs of Indian Squill Urginea Indica is a Chitinase. Biotechnol. Prog. 2006, 22, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Shokeen, P.; Bala, M.; Tandon, V. Evaluation of the Activity of 16 Medicinal Plants against Neisseria gonorrhoeae. Int. J. Antimicrob. Agents 2009, 33, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Ndhlala, A.R.; Amoo, S.O.; Stafford, G.I.; Finnie, J.F.; Van Staden, J. Antimicrobial, Anti-Inflammatory and Mutagenic Investigation of the South African Tree Aloe (Aloe barberae). J. Ethnopharmacol. 2009, 124, 404–408. [Google Scholar] [CrossRef] [PubMed]
- Bickers, D.R.; Athar, M. Oxidative Stress in the Pathogenesis of Skin Diseases. J. Invest. Dermatol. 2006, 126, 2565–2575. [Google Scholar] [CrossRef] [PubMed]
- Hakkim, F.L.; Shankar, C.G.; Girija, S. Chemical Composition and Antioxidant Property of Holy Basil (Ocimum sanctum, L.) Leaves, Stems, and Inflorescence and Their In Vitro Callus Cultures. J. Agric. Food Chem. 2007, 55, 9109–9117. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Hameed, E.S.; Salih, A.; Bazaid, S.A.; Shohayeb, M.M.; El-Sayed, M.M.; El-Wakil, E.A. Phytochemical Studies and Evaluation of Antioxidant, Anticancer and Antimicrobial Properties of Conocarpus erectus, L. Growing in Taif, Saudi Arabia. Eur. J. Med. Plants 2012, 2, 93–1123. [Google Scholar] [CrossRef]
- Saheed, S.; Ashafa, A.; Tom, O. Cytotoxicity, Antimicrobial and Antidiarrhoeal Activities of Standardised Aqueous Root Extract of Elephantorrhiza elephantina (Burch.). Trans. R. Soc. S. Afr. 2017, 72, 75–84. [Google Scholar] [CrossRef]
- Maphosa, V.; Masika, P.J.; Moyo, B. Toxicity Evaluation of the Aqueous Extract of the Rhizome of Elephantorrhiza elephantina (Burch.) Skeels. (Fabaceae), in Rats. Food Chem. Toxicol. 2010, 48, 196–201. [Google Scholar] [CrossRef]
- Pohl, T.; Koorbanally, C.; Crouch, N.R.; Mulholland, D.A. Bufadienolides from Drimia robusta and Urginea altissima (Hyacinthaceae). Phytochemistry 2001, 58, 557–561. [Google Scholar] [CrossRef]
- Kellerman, T.S.; Coetzer, J.A.W.; Naudé, T.W.; Botha, C.J. Plant Poisonings and Mycotoxicoses of Livestock in Southern Africa; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Botha, C.J.; Naudé, T.W. Plant Poisonings and Mycotoxicoses of Importance in Horses in Southern Africa. J. S. Afr. Vet. Assoc. 2002, 73, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Pereira, W.K.V.; Lonardoni, M.V.C.; Grespan, R.; Caparroz-Assef, S.M.; Cuman, R.K.N.; Bersani-Amado, C.A. Immunomodulatory Effect of Canova Medication on Experimental Leishmania amazonensis Infection. J. Infect. 2005, 51, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Elisha, I.L.; Jambalang, A.R.; Botha, F.S.; Buys, E.M.; McGaw, L.J.; Eloff, J.N. Potency and Selectivity Indices of Acetone Leaf Extracts of Nine Selected South African Trees against Six Opportunistic Enterobacteriaceae Isolates from Commercial Chicken Eggs. BMC Complement. Altern. Med. 2017, 17, 90. [Google Scholar] [CrossRef] [PubMed]
- Cho-Ngwa, F.; Abongwa, M.; Ngemenya, M.N.; Nyongbela, K.D. Selective Activity of extracts of Margaritaria discoidea and Homalium africanum on Onchocerca ochengi. BMC Complement. Altern. Med. 2010, 10. [Google Scholar] [CrossRef] [PubMed]
- Kuete, V. Potential of Cameroonian Plants and Derived Products against Microbial Infections: A Review. Planta Med. 2010, 76, 1479–1491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negi, J.S.; Singh, P.; Rawat, B. Chemical Constituents and Biological Importance of Swertia: A Review. Curr. Res. Chem. 2011, 3, 1–15. [Google Scholar] [CrossRef]
- Harborne, J.B. New Naturally Occurring Plant Polyphenols. In Polyphenolic Phenomena; Scalbert, A., Ed.; INRA: Paris, France, 1993. [Google Scholar]
- Robards, K.; Prenzler, P.D.; Tucker, G.; Swatsitang, P.; Glover, W. Phenolic Compounds and Their Role in Oxidative Processes in Fruits. Food Chem. 1999, 66, 401–436. [Google Scholar] [CrossRef]
- Gallo, M.B.C.; Sarachine, M.J. Biological Activities of Lupeol. Int. J. Biomed. Pharm. Sci. 2009, 3, 46–66. [Google Scholar]
- Bujdáková, H.; Kuchta, T.; Sidóová, E.; Gvozdjaková, A. Anti-Candida Activity of Four Antifungal Benzothiazoles. Fed. Eur. Microbiol. Soc. Microbiol. Lett. 1993, 112, 329–333. [Google Scholar] [CrossRef]
- Eloff, J.N. A Sensitive and Quick Microplate Method to Determine the Minimal Inhibitory Concentration of Plant Extracts for Bacteria. Planta Med. 1998, 64, 711–713. [Google Scholar] [CrossRef] [Green Version]
- McGaw, L.J.; Van der Merwe, D.; Eloff, J.N. In Vitro Anthelmintic, Antibacterial and Cytotoxic Effects of Extracts from Plants Used in South African Ethnoveterinary Medicine. Vet J. 2007, 173, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Masoko, P.; Picard, J.; Eloff, J.N. The Antifungal Activity of Twenty-Four Southern African Combretum Species (Combretaceae). S. Afr. J. Bot. 2007, 73, 173–183. [Google Scholar] [CrossRef]
- Karioti, A.; Hadjipavlou-Litina, D.; Mensah, M.L.K.; Fleischer, T.C.; Skaltsa, H. Composition and Antioxidant Activity of the Essential Oils of Xylopia aethiopica (Dun) A. Rich. (Annonaceae) Leaves, Stem Bark, Root Bark, and Fresh and Dried Fruits, Growing in Ghana. J. Agric. Food Chem. 2004, 52, 8094–8098. [Google Scholar] [CrossRef] [PubMed]
- Amarowicz, R.; Pegg, R.B.; Rahimi-Moghaddam, P.; Barl, B.; Weil, J.A. Free-Radical Scavenging Capacity and Antioxidant Activity of Selected Plant Species from the Canadian Prairies. Food Chem. 2004, 84, 551–562. [Google Scholar] [CrossRef]
- Mosmann, T. Rapid Colorimetric Assay for Cellular Growth and Survival: Application to Proliferation and Cytotoxicity Assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Makkar, H.P.S. Quantification of Tannins in Tree Foliage: A Laboratory Manual for the Fao/Iaea Co-Ordinated Research Project on Use of Nuclear and Related Techniques to Develop Simple Tannin Assay for Predicting and Improving the Safety and Efficiency of Feeding Ruminants on the Tanniniferous Tree Foliage; Joint Food Agricultural Organisation/International Atomic Energy Agency Division of Nuclear Techniques in Food and Agriculture: Vienna, Austria, 1999; pp. 1–29. [Google Scholar]
- Zhishen, J.; Mengcheng, T.; Jianming, W. The Determination of Flavonoid Contents in Mulberry and Their Scavenging Effects on Superoxide Radicals. Food Chem. 1999, 64, 555–559. [Google Scholar] [CrossRef]
- Mwinga, J.L.; Asong, J.A.; Amoo, S.O.; Nkadimeng, S.M.; McGaw, L.J.; Aremu, A.O.; Otang-Mbeng, W. In Vitro Antimicrobial Effects of Hypoxis hemerocallidea against Six Pathogens with Dermatological Relevance and Its Phytochemical Characterization and Cytotoxicity Evaluation. J. Ethnopharmacol. 2019, 242, 112048. [Google Scholar] [CrossRef]

| Plant, Voucher No., Family | Plant Part | Extract Yield (% w/w) | Solvent Extract | Antibacterial Activity MIC (mg/mL) | Antifungal Activity MIC (mg/mL) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Bacillus cereus | Shigella flexneri | Candida glabrata | Candida krusei | Trichophyton rubrum | Trichophyton tonsurans | ||||
| Drimia sanguinea (Schinz) Jessop Ja004, Asparagaceae | Bulb | 7 | 50% MeOH | 6.25 | 6.25 | 3.125 | 1.56 | 1.56 | 6.25 |
| 6 | PE | 6.25 | 6.25 | 6.25 | 3.125 | 3.125 | 6.25 | ||
| Elephantorrhiza elephantina Benth (Burch) Ja015, Fabaceae | Rhizome | 22 | 50% MeOH | 0.20 | 0.20 | 0.10 | 3.125 | 0.10 | 0.10 |
| 6 | PE | 3.125 | 3.125 | 3.125 | 6.25 | 3.125 | 6.25 | ||
| Helichrysum paronychioides DC. Humbert Ja037, Asteraceae | Whole plant | 9 | 50% MeOH | 0.39 | 0.39 | 6.25 | 6.25 | 6.25 | 0.39 |
| 3 | PE | 1.56 | 0.10 | 1.56 | 0.39 | 3.125 | 0.39 | ||
| Senecio longiflorus (DC). Sch.Bip Ja071, Asteraceae | Stem & leaves | 10 | 50% MeOH | 6.25 | 0.10 | 3.125 | 6.25 | 3.125 | 3.125 |
| 4 | PE | 6.25 | 6.25 | 6.25 | 12.5 | 3.125 | 6.25 | ||
| * Neomycin (μg/mL) | 1.56 | 0.78 | na | na | na | na | |||
| * Amphotericin B (μg/mL) | na | na | 0.78 | 1.56 | 0.78 | 0.78 | |||
| Plant | Plant Part Used | DPPH (EC50 µg/mL) | # Antioxidant (%) |
|---|---|---|---|
| Drimia sanguinea | Bulb | 92.6 ± 4.34 d | 64.8 ± 1.05 c |
| Elephantorrhiza elephantina | Rhizome | 5.8 ± 0.46 a | 84.7 ± 0.59 a |
| Helichrysum paronychioides | Whole plant | 20.1 ± 0.42 b,c | 84.4 ± 0.69 a |
| Senecio longiflorus | Stem and leaves | 12.1 ± 0.35 a,b | 75.3 ± 0.25 b |
| Plant | Part Used | Extract Type | LC50 (µg/mL) |
|---|---|---|---|
| Drimia sanguinea | Bulb | 50% MeOH | 0.015 ± 0.01 |
| PE | 552.4 ± 48.00 | ||
| Elephantorrhiza elephantina | Rhizome | 50% MeOH | 9.4 ± 3.90 |
| PE | 173.5 ± 13.00 | ||
| Helichrysum paronychioides | Whole plant | 50% MeOH | 24.6 ± 0.40 |
| PE | 50.2 ± 1.80 | ||
| Senecio longiflorus | Stem and leaves | 50% MeOH | 5622.0 ± 44.00 |
| PE | 105.2 ± 79.00 |
| Plant Species (Plant Part) | Extract Type | Selectivity Index (LC50/MIC) | |||||
|---|---|---|---|---|---|---|---|
| Bacterial Species | Fungal Species | ||||||
| Bacillus cereus | Shigella flexneri | Candida glabrata | Candida krusei | Trichophyton rubrum | Trichophyton tonsurans | ||
| Drimia sanguinea (Bulb) | 50% MeOH | 0.0002 | 0.0002 | 0.0005 | 9.6 | 9.6 | 0.0002 |
| PE | 0.09 | 0.09 | 0.09 | 0.18 | 0.18 | 0.09 | |
| Elephantorrhiza elephantina (Rhizome) | 50% MeOH | 0.047 | 0.047 | 0.094 | 0.003 | 0.047 | 0.047 |
| PE | 0.05 | 0.05 | 0.05 | 0.3 | 0.05 | 0.3 | |
| Helichrysum paronychioides (Whole plant) | 50% MeOH | 0.06 | 0.06 | 0.004 | 0.004 | 0.004 | 0.06 |
| PE | 0.03 | 0.5 | 0.03 | 0.1 | 0.01 | 0.1 | |
| Senecio longiflorus (Stem and leaves) | 50% MeOH | 0.9 | 56.2 | 1.8 | 0.9 | 1.8 | 1.8 |
| PE | 0.4 | 0.4 | 0.4 | 0.008 | 0.03 | 0.4 | |
| Name of Compound | A% ≥ 3 | MF | SI (%) | DT(s) |
|---|---|---|---|---|
| A. Drimia sanguinea (PE) | ||||
| (1) Pentanoic acid | 3.8 | C5H10O2 | 91.2 | 171.5 |
| (2) n-Hexadecanoic acid | 5.9 | C16H32O2 | 92.4 | 972.0 |
| (3) 1-Nonadecene | 5.1 | C19H38 | 76.1 | 977.1 |
| (4) Hexadecanoic acid, ethyl ester | 5.0 | C18H36O2 | 89.5 | 977.5 |
| (5) Diisooctyl phthalate | 5.2 | C24H38O4 | 92.1 | 1302.7 |
| (6) α-Sitosterol | 3.5 | C29H50O | 89.8 | 1657.9 |
| B1. Elephantorrhiza elephantina (PE) | ||||
| (7) Diisooctyl phthalate | 16.8 | C24H38O4 | 92.6 | 1304.5 |
| (8) Pregnenolone | 7.9 | C21H32O2 | 54.5 | 1657.3 |
| (9) α-Sitosterol | 7.8 | C29H50O | 77.1 | 1659.3 |
| (10) Lupeol | 7.9 | C30H50O | 90.7 | 1686.6 |
| (11) Cycloeucalenol acetate | 8.2 | C32H52O2 | 77.3 | 1687.7 |
| (12) Unknown 2 | 3.6 | C24H28O3S | 46.8 | 1684.6 |
| B2. Elephantorrhiza elephantina (50% MeOH) | ||||
| (13) Pentanoic acid, 2-methyl-, anhydride | 7.7 | C12H22O3 | 80.3 | 233.4 |
| (14) Pentanoic acid, 4-oxo- | 3.5 | C5H8O3 | 92.6 | 235.9 |
| (15) 1H-Imidazole-4-ethanamine, α-methyl- | 3.1 | C6H11N3 | 60.5 | 237.2 |
| (16) Benzothiazole | 3.0 | C7H5NS | 96.2 | 327.0 |
| (17) Carbonic acid, but-3-yn-1-yl heptadecyl ester | 4.3 | C22H40O3 | 64.3 | 613.6 |
| C1. Helichrysum paronychioides (PE) | ||||
| (18) Methyl 2,4,6-trihydroxybenzoate | 3.1 | C8H8O5 | 72.5 | 899.4 |
| (19) 2-Chloroethanol, triisobutylsilyl ether | 6.7 | C14H31CIC | 62.6 | 1152.7 |
| (20) (1-Cyclohexylmethyl-3-methylbut-2-enylthio)benzene | 6.7 | C18H26S | 56.1 | 1153.3 |
| (21) Benzenamine, 2-iodo- | 5.2 | C6H6IN | 65.2 | 1172.8 |
| (22) 2(3H)-Benzofuranone, 3α,4,5,6-tetrahydro-3α,6,6-trimethyl- | 9.0 | C11H16O2 | 64.7 | 1199.3 |
| (23) 4,5,6,7-Tetrahydro-benzo[c]thiophene-1-carboxylic acid allylamide | 8.6 | C12H15NOS | 60.8 | 1200.0 |
| (24) 3-Buten-2-one,4-(3-hydroxy-6,6-dimethyl-2-methylenecyclohexyl)- | 3.9 | C13H20O2 | 60.6 | 1211.2 |
| (25) Unknown 6 | 3.7 | C17H17N3O | 29.5 | 1211.5 |
| C2. Helychrysum paronychioides (50% MeOH) | ||||
| (26) Methyl 2,4,6-trihydroxybenzoate | 4.5 | C8H8O5 | 72.5 | 899.4 |
| (27) Falcarinol, trimethylsaline | 5.8 | C20H32OSi | 50.1 | 1150.4 |
| (28) 1-(5-Hexyl-2,4-dihydroxyphenyl) ethanone | 5.8 | C14H20O3 | 62.8 | 1151.0 |
| (29) Unknown 4 | 5.4 | C12H14N4O4 | 44.4 | 1152.3 |
| (30) 2,5-Cyclohexadiene-1,4-dione, 2,5-bis(1,1-dimethylpropyl)- | 3.3 | C16H24O2 | 64.5 | 1192.3 |
| (31) Pyrimidine-5-carboxylicacid,1,2,3,4-tetrahydro-6-methyl-2-oxo-4-(2-thienyl)-, isopropyl ester | 5.3 | C13H16N2O3S | 62.4 | 1197.6 |
| (32) 4,5,6,7-Tetrahydro-benzo[c]thiophene-1-carboxylic acid allylamide | 5.4 | C12H15NO | 63.7 | 1197.8 |
| (33) 5H-Benzo[b]pyran-8-ol,2,3,5,5,8α-pentamethyl-6,7,8,8α-tetrahydro- | 3.2 | C14H22O2 | 60.4 | 1209.5 |
| (34) Olivetol, [Tert-butyl (dimethyl)silyl] | 5.9 | C17H30O2Si | 56.0 | 1240.2 |
| (35) 4,5,6,7-Tetrahydro-benzo[c]thiophene-1-carboxylic acid allylamide | 5.9 | C12H15NO | 62.0 | 1241.5 |
| (36) 4′-hydroxy-2′,6′-dimethoxy-3′-(3-methyl-2-butenyl)-acetophenone | 4.3 | C15H20O4 | 55.9 | 1282.2 |
| (37) 4,5,6,7-Tetrahydro-benzo[c]thiophene-1-carboxylic acid allylamide | 4.3 | C12H15NO | 55.7 | 1284.3 |
| (38) 4,5,6,7-Tetrahydro-benzo[c]thiophene-1-carboxylic acid allylamide | 4.2 | C12H15NO | 62.0 | 1285.0 |
| (39) 2,5-cyclohexadien-1-one,2,6-bis(1,1-dimethylethyl)-4-hydroxy-4methyl- | 3.5 | C15H24O2 | 60.1 | 1296.4 |
| D1. Senecio longiflorus (PE) | ||||
| (40) Dotriacontane | 13.6 | C32H66 | 94.7 | 1604.0 |
| (41) 6 βBicyclo [4.3.0] nonane, 5β-iodomethyl-1β-41) isopropenyl-4α,5α-dimethyl-, | 3.0 | C15H25I | 68.3 | 1676.0 |
| (42) Lupeol | 7.4 | C30H50O | 88.7 | 1680.2 |
| (43) 1,3,6,10-Cyclotetradecatetraene, 14-isopropyl-3,7,11-trimethyl- | 7.8 | C20H32 | 79.5 | 1680.6 |
| (44) 9,19-Cyclolanostan-3-ol, acetate, (3β)- | 4.2 | C32H54O2 | 69.7 | 1688.9 |
| (45) Heptacosane | 3.6 | C27H56 | 90.1 | 1689.8 |
| (46) Lup-20(29)-en-3-one | 4.0 | C30H48O | 82.1 | 1692.1 |
| (47) Lupeol | 6.8 | C30H50O | 86.8 | 1697.5 |
| (48) 1,3,6,10-Cyclotetradecatetraene, 14-isopropyl-3,7,11-trimethyl- | 8.5 | C20H32 | 82.8 | 1698.4 |
| D2. Senecio longiflorus (50% MeOH) | ||||
| (49) 1-Hydroxymethyl-2-methyl-1-cyclohexene | 11.1 | C8H14O | 70.1 | 272.3 |
| (50) 4H-Pyran-4-one, 2,3-dihydro-3,5-dihydroxy-6-methyl- | 11.1 | C6H8O4 | 87.9 | 272.6 |
| (51) 4-Hydroxy-4-methylhex-5-enoic acid, tert.-butyl ester | 10.0 | C11H20O3 | 68.7 | 274.0 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asong, J.A.; Amoo, S.O.; McGaw, L.J.; Nkadimeng, S.M.; Aremu, A.O.; Otang-Mbeng, W. Antimicrobial Activity, Antioxidant Potential, Cytotoxicity and Phytochemical Profiling of Four Plants Locally Used against Skin Diseases. Plants 2019, 8, 350. https://0-doi-org.brum.beds.ac.uk/10.3390/plants8090350
Asong JA, Amoo SO, McGaw LJ, Nkadimeng SM, Aremu AO, Otang-Mbeng W. Antimicrobial Activity, Antioxidant Potential, Cytotoxicity and Phytochemical Profiling of Four Plants Locally Used against Skin Diseases. Plants. 2019; 8(9):350. https://0-doi-org.brum.beds.ac.uk/10.3390/plants8090350
Chicago/Turabian StyleAsong, John A., Stephen O. Amoo, Lyndy J. McGaw, Sanah M. Nkadimeng, Adeyemi O. Aremu, and Wilfred Otang-Mbeng. 2019. "Antimicrobial Activity, Antioxidant Potential, Cytotoxicity and Phytochemical Profiling of Four Plants Locally Used against Skin Diseases" Plants 8, no. 9: 350. https://0-doi-org.brum.beds.ac.uk/10.3390/plants8090350