Fabrication and In-Vivo Study of Micro-Colloidal Zanthoxylum acanthopodium-Loaded Bacterial Cellulose as a Burn Wound Dressing
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Method
2.2.1. Production of MZA
2.2.2. In-Situ Fabrication of BC-Loaded MZA
2.2.3. BC-MZA Composite Purification
2.2.4. Fourier-Transform Infrared Spectroscopy (FTIR)
2.2.5. X-Ray Diffraction (XRD)
2.2.6. Scanning Electron Microscopy (SEM)
2.2.7. Thermogravimetric Analysis (TGA)
2.2.8. Moisture Content (Mc)
2.2.9. Porosity Assessment
2.2.10. Hemocompatibility Test
2.2.11. In-Vivo Test (Full-Thickness Burn Wound)
2.2.12. Wound Closure Assessment
2.2.13. Microbiological Examination
2.2.14. Histopathological Observation
3. Results
3.1. FTIR BC-MZA Composites
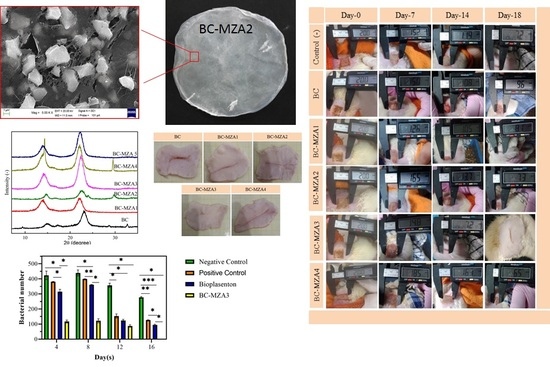
3.2. XRD of BC-MZA Composites
3.3. Morphology of BC-MZA Composite
3.4. TGA/DTGA BC-MZA Composites
3.5. Moisture Content (%) and Porosity (%)
3.6. Hemocompatibility (%)
3.7. Microbiological Examination
3.8. In-Vivo Test of BC-MZA Composites
Wound Closure
3.9. Histopathological Observation
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, L.; Deng, H.; Cui, H.; Fang, J.; Zuo, Z.; Deng, J.; Li, Y.; Wang, X.; Zhao, L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget 2018, 9, 7204–7218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eming, S.A.; Martin, P.; Tomic-canic, M. Wound repair and regeneration: Mechanisms, signaling and translation. Sci. Transl. Med. 2014, 6, 1–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, Y.; Zhao, X.; Hu, T.; Chen, B.; Yin, Z.; Ma, P.X.; Guo, B. Adhesive Hemostatic Conducting Injectable Composite Hydrogels with Sustained Drug Release and Photothermal Antibacterial Activity to Promote Full-Thickness Skin Regeneration During Wound Healing. Small 2019, 15, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Mir, M.; Ali, M.N.; Barakullah, A.; Gulzar, A.; Arshad, M.; Fatima, S.; Asad, M. Synthetic polymeric biomaterials for wound healing: A review. Prog. Biomater. 2018, 7, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Dabiri, G.; Damstetter, E.; Phillips, T. Choosing a Wound Dressing Based on Common Wound Characteristics. Adv. Wound Care 2016, 5, 32–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, H.; Wang, C.; Li, C.; Qin, Y.; Wang, Z.; Yang, F.; Li, Z.; Wang, J. A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing. RSC Adv. 2018, 8, 7533–7549. [Google Scholar] [CrossRef] [Green Version]
- Ehterami, A.; Salehi, M.; Farzamfar, S.; Vaez, A.; Samadian, H.; Sahrapeyma, H.; Mirzaii, M.; Ghorbani, S.; Goodarzi, A. In vitro and in vivo study of PCL/COLL wound dressing loaded with insulin-chitosan nanoparticles on cutaneous wound healing in rats model. Int. J. Biol. Macromol. 2018, 117, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Mohamad, N.; Loh, E.Y.X.; Fauzi, M.B.; Ng, M.H.; Mohd Amin, M.C.I. In vivo evaluation of bacterial cellulose/acrylic acid wound dressing hydrogel containing keratinocytes and fibroblasts for burn wounds. Drug Deliv. Transl. Res. 2019, 9, 444–452. [Google Scholar] [CrossRef]
- Sood, A.; Granick, M.S.; Tomaselli, N.L. Wound Dressings and Comparative Effectiveness Data. Adv. Wound Care 2014, 3, 511–529. [Google Scholar] [CrossRef] [Green Version]
- Marin, S.; Kaya, M.G.A.; Ghica, M.V.; Dinu-Pîrvu, C.; Popa, L.; Udeanu, D.I.; Mihai, G.; Enachescu, M. Collagen-Polyvinyl Alcohol-Indomethacin Biohybrid Matrices as Wound Dressings. Pharmaceutics 2018, 10, 224. [Google Scholar] [CrossRef] [Green Version]
- Amaturrahim, S.A.; Gea, S.; Nasution, D.Y.; Hutape, Y.A. Preparation of Graphene Oxide/Bacterial Cellulose Nanocomposite via in situ Process in Agitated Culture. Asian J. Chem. 2018, 27, 3188–3196. [Google Scholar] [CrossRef]
- Gea, S.; Pasaribu, K.M.; Sebayang, K.; Julianti, E.; Amaturahim, S.A.; Rahayu, S.U.; Hutapea, Y.A. Enhancing the quality of nata de coco starter by channeling the oxygen into the bioreactor through agitation method. AIP Conf. Proc. 2018, 2049, 020064. [Google Scholar]
- Wang, B.; Lin, F.; Li, X.; Zhang, Z.; Xue, X.; Liu, S.; Ji, X.; Yu, Q.; Yuan, Z.; Chen, X.; et al. Isothermal crystallization and rheology properties of isotactic polypropylene/bacterial cellulose composite. Polymers 2018, 10, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gea, S.; Sari, R.M.; Piliang, A.F.; Indrawan, D.P.; Hutapea, Y.A. Study of bacterial cellulose as scaffold on cartilage tissue engineering. AIP Conf. Proc. 2018, 2049, 020061. [Google Scholar]
- Lv, X.; Yang, J.; Feng, C.; Li, Z.; Chen, S.; Xie, M.; Huang, J.; Li, H.; Wang, H.; Xu, Y. Bacterial Cellulose-Based Biomimetic Nanofibrous Scaffold with Muscle Cells for Hollow Organ Tissue Engineering. ACS Biomater. Sci. Eng. 2016, 2, 19–29. [Google Scholar] [CrossRef]
- Picheth, G.F.; Pirich, C.L.; Sierakowski, M.R.; Woehl, M.A.; Sakakibara, C.N.; De Souza, C.F.; Martin, A.A.; Da Silva, R. Bacterial cellulose in biomedical applications: A review. Int. J. Biol. Macromol. 2017, 104, 97–106. [Google Scholar] [CrossRef]
- Wang, J.; Zhao, L.; Zhang, A.; Huang, Y.; Tavakoli, J.; Tang, Y. Novel bacterial cellulose/gelatin hydrogels as 3D scaffolds for tumor cell culture. Polymers 2018, 10, 6. [Google Scholar] [CrossRef] [Green Version]
- Sukhtezari, S.; Almasi, H.; Pirsa, S.; Zandi, M.; Pirouzifard, M.K. Development of bacterial cellulose based slow-release active films by incorporation of Scrophularia striata Boiss. extract. Carbohydr. Polym. 2017, 156, 340–350. [Google Scholar] [CrossRef]
- Numata, Y.; Mazzarino, L.; Borsali, R. A Slow-Release System of Bacterial Cellulose Gel and Nanoparticles for Hydrophobic Active Ingredients. Int. J. Pharm. 2015, 486, 217–225. [Google Scholar] [CrossRef]
- Wijaya, C.H.; Napitupulu, F.I.; Karnady, V.; Indariani, S. A review of the bioactivity and flavor properties of the exotic spice “andaliman” (Zanthoxylum acanthopodium DC.). Food Rev. Int. 2019, 35, 1–19. [Google Scholar] [CrossRef]
- Yanti; Yonzone, R.; Pramudito, T.E.; Nuriasari, N.; Juliana, K. Lemon Pepper Fruit Extract (Zanthoxylum acanthopodium DC.) Suppresses the Expression of Inflammatory Mediators in Lipopolysaccharide-Induced Macrophages In Vitro. Am. J. Biochem. Biotechnol. 2011, 7, 190–195. [Google Scholar]
- Yonzone, R.; Rai, S. Zanthoxylum Acanthopodium DC. (Rutaceae)—A Favourable Ethnomedicinal Fruit for The Local Inhabitants of Darjeeling Himalaya of West Bengal, India. J. Complement. Med. Altern. Healthc. 2016, 1, 7–10. [Google Scholar]
- Majumder, M.; Sharma, H.K.; Zaman, K.; Lyngdoh, W. Evaluation of physico-chemical properties and antibacterial activity of the essential oil obtained from the fruits of Zanthoxyllum acanthopodium DC. collected from Meghalaya, India. Int. J. Pharm. Pharm. Sci. 2014, 6, 543–546. [Google Scholar]
- Gea, S.; Reynolds, C.T.; Roohpour, N.; Wirjosentono, B.; Soykeabkaew, N.; Bilotti, E.; Peijs, T. Investigation Into the Structural, Morphological, Mechanical and Thermal Behaviour of Bacterial Cellulose After A Two-Step Purification Process. Bioresour. Technol. 2011, 102, 9105–9110. [Google Scholar] [CrossRef]
- Chuah, C.; Wang, J.; Tavakoli, J.; Tang, Y. Novel bacterial cellulose-poly (acrylic acid) hybrid hydrogels with controllable antimicrobial ability as dressings for chronic wounds. Polymers 2018, 10, 12. [Google Scholar] [CrossRef] [Green Version]
- Marins, J.A.; Soares, B.G.; Dahmouche, K.; Ribeiro, S.J.L.; Barud, H.; Bonemer, D. Structure and Properties of Conducting Bacterial Cellulose-Polyaniline Nanocomposites. Cellulose 2011, 18, 1285–1294. [Google Scholar] [CrossRef]
- Costa, A.F.S.; Almeida, F.C.G.; Vinhas, G.M.; Sarubbo, L.A. Production of Bacterial Cellulose by Gluconacetobacter Hansenii Using Corn Steep Liquor as Nutrient Sources. Front. Microbiol. 2017, 8, 1–12. [Google Scholar] [CrossRef]
- Yang, J.; Lv, X.; Chen, S. In situ fabrication of a microporous bacterial cellulose/potato starch composite scaffold with enhanced cell compatibility. Cellulose 2014, 21, 1823–1835. [Google Scholar] [CrossRef]
- Grande, C.J.; Torres, F.G.; Gomez, C.M.; Troncoso, O.P.; Canet-Ferrer, J.; Martínez-Pastor, J. Development of self-assembled bacterial cellulose-starch nanocomposites. Mater. Sci. Eng. 2009, 29, 1098–1104. [Google Scholar] [CrossRef]
- Cai, Z.; Chen, P.; Jin, H.J.; Kim, J. The effect of chitosan content on the crystallinity, thermal stability, and mechanical properties of bacterial cellulose-chitosan composites. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2009, 223, 2225–2230. [Google Scholar] [CrossRef]
- Andrade, F.K.; Silva, J.P.; Carvalho, M.; Castanheira, E.M.S.; Soares, R.; Gama, M. Studies on the hemocompatibility of bacterial cellulose. J. Biomed. Mater. Res. Part A. 2011, 98A, 554–566. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Liang, Y.; Shi, M.; Guo, B. Anti-oxidant electroactive and antibacterial nanofibrous wound dressings based on poly(ε-caprolactone)/quaternized chitosan-graft-polyaniline for full-thickness skin wound healing. Chem. Eng. J. 2020, 385, 123464. [Google Scholar] [CrossRef]
- Zhao, X.; Guo, B.; Wu, H.; Liang, Y.; Ma, P.X. Injectable antibacterial conductive nanocomposite cryogels with rapid shape recovery for noncompressible hemorrhage and wound healing. Nat. Commun. 2018, 9, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]







| Sample Name | BC (g/L MZA) |
|---|---|
| BC-MZA1 | 5 |
| BC-MZA2 | 10 |
| BC-MZA3 | 15 |
| BC-MZA4 | 20 |
| BC-MZA5 | 25 |
| Sample | CrI (%) |
|---|---|
| BC | 82.88 |
| BC-MZA1 | 73.30 |
| BC-MZA2 | 70.27 |
| BC-MZA3 | 75.84 |
| BC-MZA4 | 75.22 |
| BC-MZA5 | 72.85 |
| Sample | BC | BC-MZA1 | BC-MZA2 | BC-MZA3 | BC-MZA4 | BC-MZA5 |
|---|---|---|---|---|---|---|
| Tmax (°C) | 357.8 | 328.7 | 332.5 | 334.5 | 334.4 | 332.2 |
| Residual mass (%) | 27.98 | 13.08 | 13.32 | 27.93 | 24.49 | 14.63 |
| Sample | Moisture Content (%) | Porosity (%) | Hemocompatibility (%) |
|---|---|---|---|
| BC | 98.9 ± 0.15 | 78.2 ± 0.13 | 1.52 ± 0.02 |
| BC-MZA1 | 97.8 ± 0.08 | 77.8 ± 0.08 | 1.52 ± 0.01 |
| BC-MZA2 | 97.5 ± 0.10 | 77.5 ± 0.02 | 1.55 ± 0.03 |
| BC-MZA3 | 96.7 ± 0.07 | 76.3 ± 0.05 | 1.58 ± 0.03 |
| BC-MZA4 | 96.5 ± 0.08 | 74.2 ± 0.06 | 1.7 ± 0.02 |
| BC-MZA5 | 95.2 ± 0.05 | 73.9 ± 0.08 | 2.05 ± 0.05 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pasaribu, K.M.; Gea, S.; Ilyas, S.; Tamrin, T.; Sarumaha, A.A.; Sembiring, A.; Radecka, I. Fabrication and In-Vivo Study of Micro-Colloidal Zanthoxylum acanthopodium-Loaded Bacterial Cellulose as a Burn Wound Dressing. Polymers 2020, 12, 1436. https://0-doi-org.brum.beds.ac.uk/10.3390/polym12071436
Pasaribu KM, Gea S, Ilyas S, Tamrin T, Sarumaha AA, Sembiring A, Radecka I. Fabrication and In-Vivo Study of Micro-Colloidal Zanthoxylum acanthopodium-Loaded Bacterial Cellulose as a Burn Wound Dressing. Polymers. 2020; 12(7):1436. https://0-doi-org.brum.beds.ac.uk/10.3390/polym12071436
Chicago/Turabian StylePasaribu, Khatarina Meldawati, Saharman Gea, Syafruddin Ilyas, Tamrin Tamrin, Appealwan Altruistis Sarumaha, Ardiansyah Sembiring, and Izabela Radecka. 2020. "Fabrication and In-Vivo Study of Micro-Colloidal Zanthoxylum acanthopodium-Loaded Bacterial Cellulose as a Burn Wound Dressing" Polymers 12, no. 7: 1436. https://0-doi-org.brum.beds.ac.uk/10.3390/polym12071436