Ethyl Cellulose and Hydroxypropyl Methyl Cellulose Blended Methotrexate-Loaded Transdermal Patches: In Vitro and Ex Vivo
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Transdermal Patch
2.3. ATR–FTIR Analysis (Preformulation Study)
2.4. Physicochemical Evaluation of Patches
2.4.1. Surface pH
2.4.2. Physical Appearance
2.4.3. Thickness
2.4.4. Weight Uniformity
2.4.5. Folding Endurance
2.4.6. Moisture Uptake
2.4.7. Moisture Loss
2.4.8. Moisture Content
2.4.9. Tensile Strength and Percent Elongation at Break
2.4.10. Drug Content Uniformity
2.4.11. Water Vapor Transmission Rate
2.5. Stability Studies
2.6. Skin Irritation Studies
2.7. In Vitro Drug Release Studies
Kinetic Model Profiling
2.8. Ex Vivo Permeation Studies
Preparation of Rabbit Skin
2.9. Drug Retention Study
2.10. Statistical Analysis
3. Results
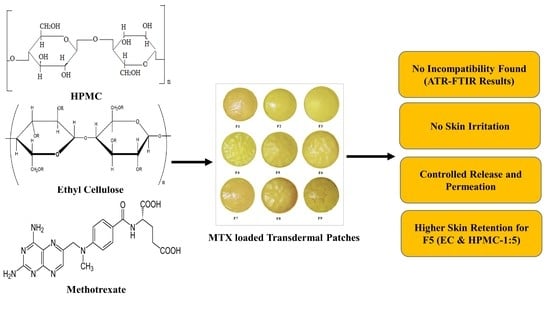
3.1. Drug Excipient Compatibility Studies (ATR–FTIR Analysis)
3.2. Physicochemical Assessment of Methotrexate-Loaded Transdermal Patches
3.3. Stability Studies
3.4. Skin Irritation Study
3.5. In Vitro Drug Release Study
3.6. Drug Release Kinetics
3.7. Ex Vivo Drug Permeation Study
3.8. Drug Retention Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Munguía-Calzada, P.; Drake-Monfort, M.; Armesto, S.; Reguero-del Cura, L.; López-Sundh, A.E.; González-López, M.A. Psoriasis flare after influenza vaccination in COVID-19 era: A report of four cases from a single center. Dermatol. Ther. 2021, 34, e14684. [Google Scholar] [CrossRef]
- Mehrmal, S.; Uppal, P.; Nedley, N.; Giesey, R.L.; Delost, G.R. The global, regional, and national burden of psoriasis in 195 countries and territories, 1990 to 2017: A systematic analysis from the Global Burden of Disease Study 2017. J. Am. Acad. Dermatol. 2021, 84, 46–52. [Google Scholar] [CrossRef]
- Gottlieb, A.B.; Merola, J.F. Axial psoriatic arthritis: An update for dermatologists. J. Am. Acad. Dermatol. 2021, 84, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Dabholkar, N.; Rapalli, V.K.; Singhvi, G. Potential herbal constituents for psoriasis treatment as protective and effective therapy. Phytother. Res. 2021, 35, 2429–2444. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Lai, R.C.; Sim, W.K.; Choo, A.B.H.; Lane, E.B.; Lim, S.K. Topical application of mesenchymal stem cell exosomes alleviates the imiquimod induced psoriasis-like inflammation. Int. J. Mol. Sci. 2021, 22, 720. [Google Scholar] [CrossRef] [PubMed]
- Elmets, C.A.; Korman, N.J.; Prater, E.F.; Wong, E.B.; Rupani, R.N.; Kivelevitch, D.; Armstrong, A.W.; Connor, C.; Cordoro, K.M.; Davis, D.M.; et al. Joint AAD–NPF Guidelines of care for the management and treatment of psoriasis with topical therapy and alternative medicine modalities for psoriasis severity measures. J. Am. Acad. Dermatol. 2021, 84, 432–470. [Google Scholar] [CrossRef] [PubMed]
- Sudhakar, K.; Fuloria, S.; Subramaniyan, V.; Sathasivam, K.V.; Azad, A.K.; Swain, S.S.; Sekar, M.; Karupiah, S.; Porwal, O.; Sahoo, A.; et al. Ultraflexible Liposome Nanocargo as a Dermal and Transdermal Drug Delivery System. Nanomaterials 2021, 11, 2557. [Google Scholar] [CrossRef]
- Dehshahri, A.; Kumar, A.; Madamsetty, V.S.; Uzieliene, I.; Tavakol, S.; Azedi, F.; Fekri, H.S.; Zarrabi, A.; Mohammadinejad, R.; Thakur, V.K. New horizons in hydrogels for methotrexate delivery. Gels 2021, 7, 2. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.; Mooney, D. Polymeric tissue adhesives. Chemical Reviews. Chem. Rev. 2021, 121, 11336–11384. [Google Scholar] [CrossRef] [PubMed]
- Ezhilarasan, D. Hepatotoxic potentials of methotrexate: Understanding the possible toxicological molecular mechanisms. Toxicology 2021, 458, 152840. [Google Scholar] [CrossRef]
- Biswasroy, P.; Pradhan, D.; Kar, B.; Ghosh, G.; Rath, G. Recent Advancement in Topical Nanocarriers for the Treatment of Psoriasis. AAPS PharmSciTech 2021, 22, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Giri, B.R.; Kim, J.S.; Park, J.H.; Jin, S.G.; Kim, K.S.; Choi, H.G.; Kim, D.W. Improved Bioavailability and High Photostability of Methotrexate by Spray-Dried Surface-Attached Solid Dispersion with an Aqueous Medium. Pharmaceutics 2021, 13, 111. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Qadir, A.; Ali, F.; Aqil, M. Phytoconstituents loaded based nanomedicines for the management of psoriasis. J. Drug Deliv. Sci. Technol. 2021, 64, 102663. [Google Scholar] [CrossRef]
- Imtiaz, M.S.; Shoaib, M.H.; Yousuf, R.I.; Ali, F.R.; Saleem, M.T.; Khan, M.Z.; Sikandar, M. Formulation development and evaluation of drug-in-adhesive-type transdermal patch of metoclopramide HCl. Polym. Bull. 2021, 2, 1–14. [Google Scholar]
- Patel, D.; Chaudhary, S.A.; Parmar, B.; Bhura, N. Transdermal drug delivery system: A review. Pharma Innov. 2012, 1, 66. [Google Scholar] [CrossRef] [Green Version]
- Bernardes, M.T.C.P.; Agostini, S.B.N.; Pereira, G.R.; da Silva, L.P.; da Silva, J.B.; Bruschi, M.L.; Novaes, R.D.; Carvalho, F.C. Preclinical study of methotrexate-based hydrogels versus surfactant based liquid crystal systems on psoriasis treatment. Eur. J. Pharm. Sci. 2021, 165, 105956. [Google Scholar] [CrossRef]
- Malviya, R.; Sundram, S.; Fuloria, S.; Subramaniyan, V.; Sathasivam, K.V.; Azad, A.K.; Sekar, M.; Kumar, D.H.; Chakravarthi, S.; Porwal, O.; et al. Evaluation and Characterization of Tamarind Gum Polysaccharide: The Biopolymer. Polymers 2021, 13, 3023. [Google Scholar] [CrossRef]
- Zaidul, I.S.; Fahim, T.K.; Sahena, F.; Azad, A.K.; Rashid, M.A.; Hossain, M.S. Dataset on applying HPMC polymer to improve encapsulation efficiency and stability of the fish oil: In vitro evaluation. Data Brief 2020, 32, 106111. [Google Scholar] [CrossRef]
- Hu, M.; Yang, J.; Xu, J. Structural and biological investigation of chitosan/hyaluronic acid with silanized-hydroxypropyl methylcellulose as an injectable reinforced interpenetrating network hydrogel for cartilage tissue engineering. Drug Deliv. 2021, 28, 607–619. [Google Scholar] [CrossRef]
- Rekhi, G.S.; Jambhekar, S.S. Ethylcellulose-a polymer review. Drug Dev. Ind. Pharm. 1995, 21, 61–77. [Google Scholar] [CrossRef]
- Wasilewska, K.; Winnicka, K. Ethylcellulose–a pharmaceutical excipient with multidirectional application in drug dosage forms development. Materials 2019, 12, 3386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kharia, A.; Singhai, A.K.; Gilhotra, R. Formualtion and evalaution of transdermal patch for the treatment of inflammation. J. Pharm. Sci. Res. 2020, 12, 780–788. [Google Scholar]
- Yang, X.; Tang, Y.; Wang, M.; Wang, Y.; Wang, W.; Pang, M.; Xu, Y. Co-delivery of methotrexate and nicotinamide by cerosomes for topical psoriasis treatment with enhanced efficacy. Int. J. Pharm. 2021, 605, 120826. [Google Scholar] [CrossRef] [PubMed]
- Ullah, W.; Nawaz, A.; Akhlaq, M.; Shah, K.U.; Latif, M.S.; Alfatama, M. Transdermal delivery of gatifloxacin carboxymethyl cellulose-based patches: Preparation and characterization. J. Drug Deliv. Sci. Technol. 2021, 66, 102783. [Google Scholar] [CrossRef]
- Sahu, K.; Pathan, S.; Khatri, K.; Upmanyu, N.; Shilpi, S. Development, characterization, in vitro and ex vivo evaluation of antiemetic transdermal patches of ondansetron hydrochloride and dexamethasone. GSC Biol. Pharm. Sci. 2021, 14, 067–078. [Google Scholar] [CrossRef]
- Jan, S.U.; Gul, R.; Jalaludin, S. Formulation and evaluation of transdermal patches of pseudoephedrine HCL. Int. J. Pharm. 2020, 5, 121–127. [Google Scholar]
- Kulkarni, S. Formulation and evaluation of transdermal patch for atomoxetine hydrochloride. J. Drug Deliv. Ther. 2019, 9, 32–35. [Google Scholar]
- Sakhare, A.D.; Biyani, K.R.; Sudke, S.G. Design and Evaluation of Transdermal Patches of Carvedilol. J. Curr. Pharm. Res. 2019, 9, 3124–3137. [Google Scholar]
- Oxley, J.A.; Ellis, C.F.; McBride, E.A.; McCormick, W.D. A survey of rabbit handling methods within the United Kingdom and the Republic of Ireland. J. Appl. Anim. Welf. Sci. 2019, 22, 207–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramadon, D.; McCrudden, M.T.; Courtenay, A.J.; Donnelly, R.F. Enhancement strategies for transdermal drug delivery systems: Current trends and applications. Drug Deliv. 2021, 1–34. [Google Scholar]
- Azad, A.K.; Al-Mahmood, S.M.; Kennedy, J.F.; Chatterjee, B.; Bera, H. Electro-hydrodynamic assisted synthesis of lecithin-stabilized peppermint oil-loaded alginate microbeads for intestinal drug delivery. Int. J. Biol. Macromol. 2021, 185, 861–875. [Google Scholar] [CrossRef] [PubMed]
- Bera, H.; Abbasi, Y.F.; Gajbhiye, V.; Liew, K.F.; Kumar, P.; Tambe, P.; Azad, A.K.; Cun, D.; Yang, M. Carboxymethyl fenugreek galactomannan-g-poly (N-isopropylacrylamide-co-N, N′-methylene-bis-acrylamide)-clay based pH/temperature-responsive nanocomposites as drug-carriers. Mater. Sci. Eng. C 2020, 110, 110628. [Google Scholar] [CrossRef] [PubMed]
- Rashid, S.A.; Bashir, S.; Ullah, H.; Ullah Shah, K.; Khan, D.H.; Shah, P.A.; Danish, M.Z.; Khan, M.H.; Mahmood, S.; Sohaib, M.; et al. Development, characterization and optimization of methotrexate-olive oil nano-emulsion for topical application. Pak. J. Pharm. Sci. 2021, 34, 205–215. [Google Scholar] [PubMed]
- Sivasankarapillai, V.S.; Das, S.S.; Sabir, F.; Sundaramahalingam, M.A.; Colmenares, J.C.; Prasannakumar, S.; Rajan, M.; Rahdar, A.; Kyzas, G.Z. Progress in natural polymer engineered biomaterials for transdermal drug delivery systems. Mater. Today Chem. 2021, 19, 100382. [Google Scholar] [CrossRef]
- Yadav, K.; Soni, A.; Singh, D.; Singh, M.R. Polymers in topical delivery of anti-psoriatic medications and other topical agents in overcoming the barriers of conventional treatment strategies. Prog. Biomater. 2021, 10, 1–17. [Google Scholar] [CrossRef]
- Latha, A.V.S.; Ravikiran, T.N.; Kumar, J.N. Formulation, Optimization and Evaluation of Glibenclamide Transdermal Patches by using chitosan Polymer. Asian J. Pharm. Technol. 2019, 9, 1–7. [Google Scholar] [CrossRef]
- Pünnel, L.C.; Lunter, D.J. Film-forming systems for dermal drug delivery. Pharmaceutics 2021, 13, 932. [Google Scholar] [CrossRef]
- Azad, A.K.; Al-Mahmood, S.M.; Chatterjee, B.; Wan Sulaiman, W.M.; Elsayed, T.M.; Doolaanea, A.A. Encapsulation of black seed oil in alginate beads as a ph-sensitive carrier for intestine-targeted drug delivery: In vitro, in vivo and ex vivo study. Pharmaceutics 2020, 12, 219. [Google Scholar] [CrossRef] [Green Version]
- Altun, E.; Yuca, E.; Ekren, N.; Kalaskar, D.M.; Ficai, D.; Dolete, G.; Ficai, A.; Gunduz, O. Kinetic Release Studies of Antibiotic Patches for Local Transdermal Delivery. Pharmaceutics 2021, 13, 613. [Google Scholar] [CrossRef]
- Haroon, M.; Batool, S.; Asif, S.; Hashmi, F.; Ullah, S. Combination of Methotrexate and Leflunomide Is Safe and Has Good Drug Retention Among Patients with Psoriatic Arthritis. J. Rheumatol. 2021, 48, 1–2. [Google Scholar] [CrossRef]
- Sabir, F.; Qindeel, M.; Rehman, A.U.; Ahmad, N.M.; Khan, G.M.; Csoka, I.; Ahmed, N. An efficient approach for development and optimisation of curcumin-loaded solid lipid nanoparticles’ patch for transdermal delivery. J. Microencapsul. 2021, 38, 233–248. [Google Scholar] [CrossRef] [PubMed]





| Batch | Amount of MTX (mg) | Total Amount of Polymers | Plasticizer PEG-400 (%) | Amount of Solvents (v/v) mL | |||
|---|---|---|---|---|---|---|---|
| EC (mg) | HPMC (mg) | Combination EC/HPMC | Dichloromethane | Ethanol | |||
| F1 (Control) | 5 | 100 | 100 | 1:1 | 25 | 20 | 20 |
| F2 | 5 | 100 | 200 | 1:2 | 25 | 20 | 20 |
| F3 | 5 | 100 | 300 | 1:3 | 25 | 20 | 20 |
| F4 | 5 | 100 | 400 | 1:4 | 25 | 20 | 20 |
| F5 | 5 | 100 | 500 | 1:5 | 25 | 20 | 20 |
| F6 | 5 | 200 | 100 | 2:1 | 25 | 20 | 20 |
| F7 | 5 | 300 | 100 | 3:1 | 25 | 20 | 20 |
| F8 | 5 | 400 | 100 | 4:1 | 25 | 20 | 20 |
| F9 | 5 | 500 | 100 | 5:1 | 25 | 20 | 20 |
| Formulation Code | Characteristics | |||||||
|---|---|---|---|---|---|---|---|---|
| Thickness (mm) | Weight Uniformity (mg) | % Moisture Absorbance | % Moisture Loss | % Drug Content | Water Transmission Rate | Folding Endurance | Tensile Strength, Kg/cm2 | |
| F1 | 0.51 ± 0.03 | 73.86 ± 0.05 | 9.25 ± 1.62 | 6.28 ± 0.85 | 97.17 ± 3.21 | 3.58 ± 0.23 | 83 ± 2.03 | 10.43 ± 0.71 |
| F2 | 0.52 ± 0.02 | 74.37 ± 0.03 | 10.81 ± 1.12 | 7.31 ± 0.21 | 99.13 ± 2.34 | 3.77 ± 0.65 | 92 ± 1.21 | 9.36 ± 0.83 |
| F3 | 0.54 ± 0.07 | 76.55 ± 0.08 | 11.36 ± 1.32 | 7.82 ± 0.38 | 96.97 ± 2.24 | 3.89 ± 0.34 | 78 ± 3.24 | 11.35 ± 0.85 |
| F4 | 0.55 ± 0.04 | 77.15 ± 0.05 | 11.56 ± 0.73 | 8.25 ± 0.22 | 97.11 ± 3.23 | 3.97 ± 0.54 | 86 ± 2.32 | 12.75 ± 0.72 |
| F5 | 0.56 ± 0.04 | 78.67 ± 0.04 | 12.79 ± 1.46 | 8.94 ± 0.62 | 95.42 ± 2.23 | 4.23 ± 0.37 | 89 ± 2.54 | 10.93 ± 0.76 |
| F6 | 0.50 ± 0.05 | 72.75 ± 0.08 | 8.45 ± 1.22 | 6.22 ± 0.15 | 99.54 ± 2.56 | 4.13 ± 0.41 | 64 ± 4.62 | 9.45 ± 0.81 |
| F7 | 0.51 ± 0.02 | 73.57 ± 0.04 | 8.99 ± 1.44 | 6.58 ± 0.45 | 97.25 ± 3.43 | 3.93 ± 0.18 | 58 ± 5.12 | 12.34 ± 0.77 |
| F8 | 0.52 ± 0.04 | 73.48 ± 0.08 | 9.67 ± 0.52 | 7.10 ± 0.23 | 98.64 ± 1.65 | 3.69 ± 0.32 | 52 ± 5.32 | 10.87 ± 0.83 |
| F9 | 0.53 ± 0.09 | 74.86 ± 0.04 | 10.24 ± 0.97 | 7.31 ± 0.57 | 97.67 ± 4.36 | 3.84 ± 0.69 | 56 ± 5.35 | 11.66 ± 0.74 |
| Evaluation Parameters | F. Code | 30 Days | 60 Days | 90 Days | 120 Days | 150 Days | 180 Days |
|---|---|---|---|---|---|---|---|
| Drug content (%) | F1 | 97.17 ± 3.21 | 97.02 ± 1.99 | 96.89 ± 1.11 | 96.72 ± 3.22 | 96.61 ± 1.21 | 96.55 ± 2.11 |
| F2 | 99.13 ± 2.01 | 99.04 ± 1.65 | 98.85 ± 1.28 | 98.77 ± 2.14 | 98.58 ± 3.11 | 98.49 ± 2.01 | |
| F3 | 96.97 ± 2.11 | 96.86 ± 2.56 | 96.71 ± 1.32 | 96.59 ± 2.14 | 96.42 ± 3.01 | 96.32 ± 2.46 | |
| F4 | 97.11 ± 3.10 | 96.89 ± 2.35 | 96.73 ± 2.12 | 96.64 ± 2.98 | 96.59 ± 2.76 | 96.47 ± 3.23 | |
| F5 | 95.42 ± 1.23 | 95.33 ± 2.27 | 95.09 ± 2.32 | 94.89 ± 2.65 | 94.76 ± 2.35 | 94.66 ± 2.87 | |
| F6 | 98.92 ± 2.11 | 98.14 ± 3.11 | 97.76 ± 2.46 | 96.56 ± 2.45 | 95.78 ± 2.26 | 95.23 ± 3.43 | |
| F7 | 99.19 ± 3.01 | 98.89 ± 1.02 | 97.93 ± 2.75 | 97.45 ± 3.46 | 96.69 ± 2.33 | 96.21 ± 3.10 | |
| F8 | 97.25 ± 2.76 | 96.87 ± 3.15 | 95.87 ± 2.46 | 95.22 ± 3.25 | 94.76 ± 3.11 | 94.32 ± 2.33 | |
| F9 | 96.63 ± 1.90 | 96.34 ± 2.32 | 95.82 ± 3.56 | 95.25 ± 2.31 | 94.78 ± 2.10 | 94.21 ± 2.19 | |
| Appearance | F1 | No change | No change | No change | No change | No change | No change |
| F2 | |||||||
| F3 | |||||||
| F4 | |||||||
| F5 | |||||||
| F6 | |||||||
| F7 | |||||||
| F8 | |||||||
| F9 |
| Rabbit Groups | Visual Observation | |
|---|---|---|
| Erythema | Edema | |
| Result of Skin Irritation Studies | ||
| Control | 0.00 ± 0.00 | 0.00 ± 0.00 |
| Adhesive tape | 0.46 ± 0.62 | 1.02 ± 0.19 |
| Blank patch | 1.12 ± 0.46 | 1.06 ± 0.31 |
| F1 Patch | 0.83 ± 0.28 | 1.25 ± 0.16 |
| F2 Patch | 0.93 ± 0.67 | 1.08 ± 0.24 |
| F3 Patch | 1.03 ± 0.82 | 0.83 ± 0.69 |
| F4 Patch | 1.25 ± 0.71 | 1.12 ± 0.33 |
| F5 Patch | 0.37 ± 0.54 | 0.72 ± 0.26 |
| F6 Patch | 0.85 ± 0.43 | 1.05 ± 0.16 |
| F7 Patch | 0.94 ± 0.83 | 1.22 ± 0.35 |
| F8 Patch | 1.04 ± 0.74 | 1.06 ± 0.66 |
| F9 Patch | 0.98 ± 0.64 | 0.86 ± 0.27 |
| Formalin | 3.05 ± 0.23 | 3.21 ± 0.51 |
| Formulations | K ± SO | R2 | N | |
|---|---|---|---|---|
| F1 | 0.001 ± 2.8337 | 0.943 | 0.307 | Fickian diffusion |
| F2 | 0.001 ± 5.0820 | 0.949 | 0.317 | Fickian diffusion |
| F3 | 0.002 ± 0.0001 | 0.940 | 0.342 | Fickian diffusion |
| F4 | 0.001 ± 0.0002 | 0.941 | 0.345 | Fickian diffusion |
| F5 | 0.001 ± 0.0005 | 0.974 | 0.501 | Anomalous non-Fickian diffusion |
| F6 | 0.001 ± 0.0001 | 0.929 | 0.301 | Fickian diffusion |
| F7 | 0.001 ± 0.0001 | 0.924 | 0.301 | Fickian diffusion |
| F8 | 0.002 ± 0.0003 | 0.933 | 0.303 | Fickian diffusion |
| F9 | 0.001 ± 0.0006 | 0.967 | 0.303 | Fickian diffusion |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Latif, M.S.; Azad, A.K.; Nawaz, A.; Rashid, S.A.; Rahman, M.H.; Al Omar, S.Y.; Bungau, S.G.; Aleya, L.; Abdel-Daim, M.M. Ethyl Cellulose and Hydroxypropyl Methyl Cellulose Blended Methotrexate-Loaded Transdermal Patches: In Vitro and Ex Vivo. Polymers 2021, 13, 3455. https://0-doi-org.brum.beds.ac.uk/10.3390/polym13203455
Latif MS, Azad AK, Nawaz A, Rashid SA, Rahman MH, Al Omar SY, Bungau SG, Aleya L, Abdel-Daim MM. Ethyl Cellulose and Hydroxypropyl Methyl Cellulose Blended Methotrexate-Loaded Transdermal Patches: In Vitro and Ex Vivo. Polymers. 2021; 13(20):3455. https://0-doi-org.brum.beds.ac.uk/10.3390/polym13203455
Chicago/Turabian StyleLatif, Muhammad Shahid, Abul Kalam Azad, Asif Nawaz, Sheikh Abdur Rashid, Md. Habibur Rahman, Suliman Y. Al Omar, Simona G. Bungau, Lotfi Aleya, and Mohamed M. Abdel-Daim. 2021. "Ethyl Cellulose and Hydroxypropyl Methyl Cellulose Blended Methotrexate-Loaded Transdermal Patches: In Vitro and Ex Vivo" Polymers 13, no. 20: 3455. https://0-doi-org.brum.beds.ac.uk/10.3390/polym13203455