Monoclonal Antibody Combinations that Present Synergistic Neutralizing Activity: A Platform for Next-Generation Anti-Toxin Drugs
Abstract
:1. Introduction
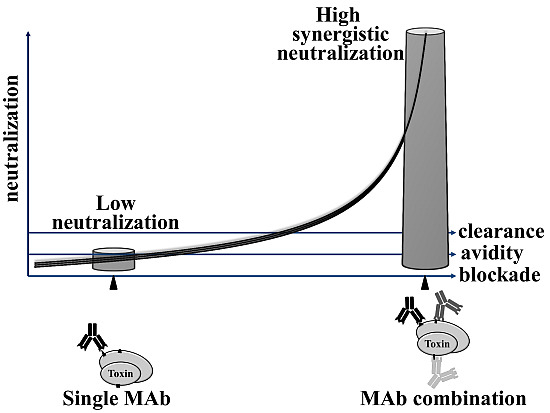
2. Synergistic Neutralization of MAb Cocktails
| Toxin | MAb number a | Fold enhancement b | In vivo/in vitro | Reference |
|---|---|---|---|---|
| Botulinum A | 3 | 20,000 | in vivo | [22] |
| 2–4 | 100 | in vivo | [8] | |
| 2–5 | 10,000 c | in vivo | [23] | |
| 2–4 | >100 | in vivo | [24] | |
| 2 | <10 | in vivo | [25] | |
| 2 | 1 | in vitro | [26] | |
| 2 | 40 | in vivo | [27] | |
| 7 | 150 | in vivo | [16] | |
| 2 d | 166 | in vivo | [28] | |
| Botulinum B | 2–4 | No e | in vivo | [29] |
| 2–3 | 30 | in vivo | [30] | |
| 2–7 | 10 | in vivo | [16] | |
| Botulinum E | 8 | 400 | in vivo | [16] |
| Difficile A | 2 | ~2 | in vitro | [31] |
| Ricin | 2 | 1.5 | in vitro | [32] |
| 3 | 7.5 f | in vivo | [33] | |
| 2 | ~2 | in vitro | [34] | |
| Pertussis toxin | 2–3 | 1 | in vivo | [35] |
| 2 | No e | in vivo | [36] | |
| 2 | >10 | in vivo | [37] | |
| 2 | 4 | in vitro | [38] | |
| 2 | >1.5 | in vivo | [39] | |
| Anthrax | 2–3 | 10–100 | in vivo | [40] |
| 2 | 1 | in vitro | [41] | |
| 2 | 1 | in vivo | [42] | |
| 2 | ~10 | in vivo | [43] | |
| 2 | 7 | in vivo | [44] | |
| 3 | Delay death | in vivo | [45] | |
| 2 | >2 g | in vitro | [46] | |
| 2 | ~10 | in vivo | [47] | |
| 2 | 1.7, 3.8 h | in vitro | [48] | |
| SEB | 2 | <10 | in vivo | [49] |
| 2 | >10 | in vivo | [50] | |
| Tetanus | 2–4 | 20 | in vivo | [51] |
| 2 | <10 | in vivo | [52] | |
| 2 | 3 | in vivo | [53] | |
| PLY | 2–3 | >5 | in vivo | [54] |
| Scorpion Aha venom | 2 | <10 | in vivo | [55] |

2.1. Simultaneous Binding of Interfering MAbs to Multiple Non-Overlapping Functional Epitopes
2.1.1. Functional Neutralizing Epitopes
2.1.2. Simultaneous Interference with Multiple Functional Epitopes

2.2. Increase in Affinity of MAb Cocktails Targeting Multiple Epitopes
2.2.1. Role of Affinity in Toxin Neutralization
2.2.2. Synergistic Neutralization Due to Enhanced Affinity

2.3. Fc-Mediated Clearance of Antibody-Toxin Complexes via Multimeric Antibody Decoration of the Toxin
2.3.1. Fc-Mediated Serum Clearance of ICs
2.3.2. New Evidence for the Role of IgG Fc in Toxin Neutralization
2.3.3. Synergistic Effect of Oligo-Fc Toxin Decoration

3. Conclusions
Author Contributions
Conflicts of Interest
References
- Kohler, G.; Milstein, C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 1975, 296, 495–497. [Google Scholar] [CrossRef]
- Beck, A.; Wurch, T.; Bailly, C.; Corvaia, N. Strategies and challenges for the next generation of therapeutic antibodies. Nat. Rev. Immunol. 2010, 10, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Chow, S.-K.; Casadevall, A. Monoclonal antibodies and toxins—A perspective on function and isotype. Toxins 2012, 4, 430–454. [Google Scholar] [CrossRef] [PubMed]
- Casadevall, A. The third age of antimicrobial therapy. Clin. Infect. Dis. 2006, 42, 1414–1416. [Google Scholar] [CrossRef] [PubMed]
- Berry, J.D.; Gaudet, R.G. Antibodies in infectious diseases: Polyclonals, monoclonals and niche biotechnology. New Biotechnol. 2011, 28, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Gunn, R.A. Hypersensitivity reactions associated with botulinal antitoxin. Am. J. Med. 1980, 69, 567–570. [Google Scholar] [CrossRef]
- Meng, Q.; Garcia-Rodriguez, C.; Manzanarez, G.; Silberg, M.A.; Conrad, F.; Bettencourt, J.; Pan, X.; Breece, T.; To, R.; Li, M.; et al. Engineered domain-based assays to identify individual antibodies in oligoclonal combinations targeting the same protein. Anal. Biochem. 2012, 430, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, J.; Tremblay, J.M.; Leysath, C.E.; Ofori, K.; Baldwin, K.; Feng, X.; Bedenice, D.; Webb, R.P.; Wright, P.M.; Smith, L.A.; et al. A novel strategy for development of recombinant antitoxin therapeutics tested in a mouse botulism model. PLoS ONE 2012, 7, e29941. [Google Scholar] [CrossRef] [PubMed]
- Marks, J.D. Deciphering antibody properties that lead to potent botulinum neurotoxin neutralization. Mov. Disord. 2004, 19 (Suppl. 8), S101–S108. [Google Scholar] [CrossRef] [PubMed]
- Chiarella, P.; Fazio, V.M. Mouse monoclonal antibodies in biological research: Strategies for high-throughput production. Biotechnol. Lett. 2008, 30, 1303–1310. [Google Scholar] [CrossRef] [PubMed]
- Harding, F.A.; Stickler, M.M.; Razo, J.; DuBridge, R.B. The immunogenicity of humanized and fully human antibodies: Residual immunogenicity resides in the CDR regions. MAbs 2010, 2, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Saylor, C.; Dadachova, E.; Casadevall, A. Monoclonal antibody-based therapies for microbial diseases. Vaccine 2009, 27 (Suppl. 6), G38–G46. [Google Scholar] [CrossRef] [PubMed]
- Fox, J.L. Anthrax drug first antibacterial mAb to win approval. Nat. Biotechnol. 2013, 31, 8. [Google Scholar] [CrossRef] [PubMed]
- Reichert, J.M. Antibody-based therapeutics to watch in 2011. MAbs 2011, 3, 76–99. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.; Li, M.; Silberg, M.A.; Conrad, F.; Bettencourt, J.; To, R.; Huang, C.; Ma, J.; Meyer, K.; Shimizu, R.; et al. Domain-based assays of individual antibody concentrations in an oligoclonal combination targeting a single protein. Anal. Biochem. 2012, 421, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Diamant, E.; Lachmi, B.E.; Keren, A.; Barnea, A.; Marcus, H.; Cohen, S.; David, A.B.; Zichel, R. Evaluating the synergistic neutralizing effect of anti-botulinum oligoclonal antibody preparations. PLoS ONE 2014, 9, e87089. [Google Scholar] [CrossRef] [PubMed]
- Arnon, S.S.; Schechter, R.; Inglesby, T.V.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Hauer, J.; Layton, M.; et al. Botulinum toxin as a biological weapon: Medical and public health managment. J. Am. Med. Assoc. 2001, 285, 1059–1070. [Google Scholar] [CrossRef]
- Gill, D.M. Bacterial toxins: A table of lethal amounts. Microbiol. Rev. 1982, 46, 86–94. [Google Scholar] [PubMed]
- Darling, R.G.; Catlett, C.L.; Huebner, K.D.; Jarrett, D.G. Threats in bioterrorism. I: CDC category A agents. Emerg. Med. Clin. North Am. 2002, 20, 273–309. [Google Scholar] [CrossRef]
- Dembek, Z.F.; Smith, L.A.; Rusnak, J.M. Botulism: Cause, effects, diagnosis, clinical and laboratory identification, and treatment modalities. Disaster Med. Public Health Prep. 2007, 1, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Logtenberg, T. Antibody cocktails: Next-generation biopharmaceuticals with improved potency. Trends Biotechnol. 2007, 25, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Nowakowski, A.; Wang, C.; Powers, D.B.; Amersdorfer, P.; Smith, T.J.; Montgomery, V.A.; Sheridan, R.; Blake, R.; Smith, L.A.; Marks, J.D. Potent neutralization of botulinum neurotoxin by recombinant oligoclonal antibody. Proc. Natl. Acad. Sci. USA 2002, 99, 11346–11350. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, J.; McCann, C.; Ofori, K.; Hill, J.; Baldwin, K.; Shoemaker, C.B.; Harrison, P.; Tzipori, S. Sheep monoclonal antibodies prevent systemic effects of botulinum neurotoxin A1. Toxins Basel 2012, 4, 1565–1581. [Google Scholar] [CrossRef] [PubMed]
- Sepulveda, J.; Mukherjee, J.; Tzipori, S.; Simpson, L.L.; Shoemaker, C.B. Efficient serum clearance of botulinum neurotoxin achieved using a pool of small antitoxin binding agents. Infect. Immun. 2010, 78, 756–763. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.W.; Stanker, L.H.; Henderson, T.D., 2nd; Lou, J.; Marks, J.D. Antibody protection against botulinum neurotoxin intoxication in mice. Infect. Immun. 2009, 77, 4305–4313. [Google Scholar] [CrossRef] [PubMed]
- Amersdorfer, P.; Wong, C.; Chen, S.; Smith, T.; Deshpande, S.; Sheridan, R.; Finnern, R.; Marks, J.D. Molecular characterization of murine humoral immune response to botulinum neurotoxin type A binding domain as assessed by using phage antibody libraries. Infect. Immun. 1997, 65, 3743–3752. [Google Scholar] [PubMed]
- Adekar, S.P.; Takahashi, T.; Jones, R.M.; Al-Saleem, F.H.; Ancharski, D.M.; Root, M.J.; Kapadnis, B.P.; Simpson, L.L.; Dessain, S.K. Neutralization of botulinum neurotoxin by a human monoclonal antibody specific for the catalytic light chain. PLoS ONE 2008, 3, e3023. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Zhao, H.; Al-Saleem, F.H.; Ubaid, A.S.; Puligedda, R.D.; Segan, A.T.; Lindorfer, M.A.; Bermudez, R.; Elias, M.; Adekar, S.P.; et al. Mechanisms of enhanced neutralization of botulinum neurotoxin by monoclonal antibodies conjugated to antibodies specific for the erythrocyte complement receptor. Mol. Immunol. 2014, 57, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Noah, C.W.; Poteet, S.S.; Ramos, N.C.; Perez, J.C.; Huang, S.Y. Production of monoclonal antibodies specific to Clostridium botulinum type B neurotoxin. J. AOAC Int. 1995, 78, 381–385. [Google Scholar] [PubMed]
- Chen, C.; Wang, S.; Wang, H.; Mao, X.; Zhang, T.; Ji, G.; Shi, X.; Xia, T.; Lu, W.; Zhang, D.; et al. Potent neutralization of botulinum neurotoxin/B by synergistic action of antibodies recognizing protein and ganglioside receptor binding domain. PLoS ONE 2012, 7, e43845. [Google Scholar] [CrossRef] [PubMed]
- Demarest, S.J.; Hariharan, M.; Elia, M.; Salbato, J.; Jin, P.; Bird, C.; Short, J.M.; Kimmel, B.E.; Dudley, M.; Woodnutt, G.; et al. Neutralization of Clostridium difficile toxin A using antibody combinations. MAbs 2010, 2, 190–198. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, C.R.; Mantis, N.J. Characterization of a novel high-affinity monoclonal immunoglobulin G antibody against the ricin B subunit. Infect. Immun. 2006, 74, 3463–3470. [Google Scholar] [CrossRef] [PubMed]
- Prigent, J.; Panigai, L.; Lamourette, P.; Sauvaire, D.; Devilliers, K.; Plaisance, M.; Volland, H.; Creminon, C.; Simon, S. Neutralising antibodies against ricin toxin. PLoS ONE 2011, 6, e20166. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.G.; Yin, J.; Chau, D.; Hu, C.C.; Lillico, D.; Yu, J.; Negrych, L.M.; Cherwonogrodzky, J.W. Conformation-dependent high-affinity potent ricin-neutralizing monoclonal antibodies. BioMed Res. Int. 2013, 2013. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Ito, A.; Chiba, J.; Sato, Y. Monoclonal antibody against pertussis toxin: Effect on toxin activity and pertussis infections. Infect. Immun. 1984, 46, 422–428. [Google Scholar] [PubMed]
- Frank, D.W.; Parker, C.D. Interaction of monoclonal antibodies with pertussis toxin and its subunits. Infect. Immun. 1984, 46, 195–201. [Google Scholar] [PubMed]
- Sato, H.; Sato, Y.; Ito, A.; Ohishi, I. Effect of monoclonal antibody to pertussis toxin on toxin activity. Infect. Immun. 1987, 55, 909–915. [Google Scholar] [PubMed]
- Kenimer, J.G.; Kim, K.J.; Probst, P.G.; Manclark, C.R.; Burstyn, D.G.; Cowell, J.L. Monoclonal antibodies to pertussis toxin: Utilization as probes of toxin function. Hybridoma 1989, 8, 37–51. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Sato, Y. Protective activities in mice of monoclonal antibodies against pertussis toxin. Infect. Immun. 1990, 58, 3369–3374. [Google Scholar] [PubMed]
- Brossier, F.; Levy, M.; Landier, A.; Lafaye, P.; Mock, M. Functional analysis of Bacillus anthracis protective antigen by using neutralizing monoclonal antibodies. Infect. Immun. 2004, 72, 6313–6317. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, M.T.; Li, H.; Williamson, E.D.; LeButt, C.S.; Flick-Smith, H.C.; Quinn, C.P.; Westra, H.; Galloway, D.; Mateczun, A.; Goldman, S.; et al. Human monoclonal antibodies against anthrax lethal factor and protective antigen act independently to protect against Bacillus anthracis infection and enhance endogenous immunity to anthrax. Infect. Immun. 2007, 75, 5425–5433. [Google Scholar] [PubMed]
- Staats, H.F.; Alam, S.M.; Scearce, R.M.; Kirwan, S.M.; Zhang, J.X.; Gwinn, W.M.; Haynes, B.F. In vitro and in vivo characterization of anthrax anti-protective antigen and anti-lethal factor monoclonal antibodies after passive transfer in a mouse lethal toxin challenge model to define correlates of immunity. Infect. Immun. 2007, 75, 5443–5452. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Moayeri, M.; Crown, D.; Emerson, S.; Gorshkova, I.; Schuck, P.; Leppla, S.H.; Purcell, R.H. Novel chimpanzee/human monoclonal antibodies that neutralize anthrax lethal factor, and evidence for possible synergy with anti-protective antigen antibody. Infect. Immun. 2009, 77, 3902–3908. [Google Scholar] [CrossRef] [PubMed]
- Winterroth, L.; Rivera, J.; Nakouzi, A.S.; Dadachova, E.; Casadevall, A. Neutralizing monoclonal antibody to edema toxin and its effect on murine anthrax. Infect. Immun. 2010, 78, 2890–2898. [Google Scholar] [CrossRef] [PubMed]
- Leysath, C.E.; Chen, K.H.; Moayeri, M.; Crown, D.; Fattah, R.; Chen, Z.; Das, S.R.; Purcell, R.H.; Leppla, S.H. Mouse monoclonal antibodies to anthrax edema factor protect against infection. Infect. Immun. 2011, 79, 4609–4616. [Google Scholar] [CrossRef] [PubMed]
- Ngundi, M.M.; Meade, B.D.; Little, S.F.; Quinn, C.P.; Corbett, C.R.; Brady, R.A.; Burns, D.L. Analysis of defined combinations of monoclonal antibodies in anthrax toxin neutralization assays and their synergistic action. Clin. Vaccine Immunol. 2012, 19, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Pohl, M.A.; Rivera, J.; Nakouzi, A.; Chow, S.K.; Casadevall, A. Combinations of monoclonal antibodies to anthrax toxin manifest new properties in neutralization assays. Infect. Immun. 2013, 81, 1880–1888. [Google Scholar] [CrossRef] [PubMed]
- Mazor, O.; Ben-Arie, E.; Mechaly, A.; Rosenfled, R.; Marcus, H.; Ordentlich, A. Combination of Anthrax-Toxin Neutralizing Antibodies: Analysis of Synergism/Antagonism effect. In The Challenge of Highly Pathogenic Microorganisms: Mechanisms of Virulence and Novel Medical Countermeasures; Shafferman, A., Ordentlich, A., Velan, B., Eds.; Springer: Dordrecht, The Netherlands, 2010; pp. 275–285. [Google Scholar]
- Tilahun, M.E.; Rajagopalan, G.; Shah-Mahoney, N.; Lawlor, R.G.; Tilahun, A.Y.; Natarajan, K.; Xie, C.; Margulies, D.H.; Ratner, D.I.; Osborne, B.A.; et al. Potent neutralization of staphylococcal enterotoxin B by synergistic action of chimeric antibodies. Infect. Immun. 2010, 78, 2801–2811. [Google Scholar] [CrossRef] [PubMed]
- Varshney, A.K.; Wang, X.; Cook, E.; Dutta, K.; Scharff, M.D.; Goger, M.J.; Fries, B.C. Generation, characterization, and epitope mapping of neutralizing and protective monoclonal antibodies against staphylococcal enterotoxin B-induced lethal shock. J. Biol. Chem. 2011, 286, 9737–9747. [Google Scholar] [CrossRef] [PubMed]
- Volk, W.A.; Bizzini, B.; Snyder, R.M.; Bernhard, E.; Wagner, R.R. Neutralization of tetanus toxin by distinct monoclonal antibodies binding to multiple epitopes on the toxin molecule. Infect. Immun. 1984, 45, 604–609. [Google Scholar] [PubMed]
- Yousefi, M.; Khosravi-Eghbal, R.; Reza Mahmoudi, A.; Jeddi-Tehrani, M.; Rabbani, H.; Shokri, F. Comparative in vitro and in vivo assessment of toxin neutralization by anti-tetanus toxin monoclonal antibodies. Hum. Vaccines Immunother. 2013, 10, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.B.; Cryz, S.J., Jr.; Schurch, U.; Ganss, M.T.; Bruderer, U. Immunotherapy with human monoclonal antibodies. Fragment A specificity of polyclonal and monoclonal antibodies is crucial for full protection against tetanus toxin. J. Immunol. 1993, 151, 466–472. [Google Scholar] [PubMed]
- Garcia-Suarez Mdel, M.; Cima-Cabal, M.D.; Florez, N.; Garcia, P.; Cernuda-Cernuda, R.; Astudillo, A.; Vazquez, F.; de los Toyos, J.R.; Mendez, F.J. Protection against pneumococcal pneumonia in mice by monoclonal antibodies to pneumolysin. Infect. Immun. 2004, 72, 4534–4540. [Google Scholar] [CrossRef] [PubMed]
- Clot-Faybesse, O.; Juin, M.; Rochat, H.; Devaux, C. Monoclonal antibodies against the Androctonus australis hector scorpion neurotoxin I: Characterisation and use for venom neutralisation. FEBS Lett. 1999, 458, 313–318. [Google Scholar] [CrossRef]
- Chou, T.C.; Talalay, P. Quantitative analysis of dose-effect relationships: The combined effects of multiple drugs or enzyme inhibitors. Adv. Enzyme Regul. 1984, 22, 27–55. [Google Scholar] [CrossRef]
- Zichel, R.; Mimran, A.; Keren, A.; Barnea, A.; Steinberger-Levy, I.; Marcus, D.; Turgeman, A.; Reuveny, S. Efficacy of a potential trivalent vaccine based on Hc fragments of botulinum toxins A, B, and E produced in a cell-free expression system. Clin. Vaccine Immunol. 2010, 17, 784–792. [Google Scholar] [CrossRef] [PubMed]
- Strohl, W.R. Optimization of Fc-mediated effector functions of monoclonal antibodies. Curr. Opin. Biotechnol. 2009, 20, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Pincus, S.H.; Smallshaw, J.E.; Song, K.; Berry, J.; Vitetta, E.S. Passive and active vaccination strategies to prevent ricin poisoning. Toxins 2011, 3, 1163–1184. [Google Scholar] [CrossRef] [PubMed]
- Lacy, D.B.; Stevens, R.C. Sequence homology and structural analysis of the clostridial neurotoxins. J. Mol. Biol. 1999, 291, 1091–1104. [Google Scholar] [CrossRef] [PubMed]
- Atassi, M.Z.; Dolimbek, B.Z.; Hayakari, M.; Middlebrook, J.L.; Whitney, B.; Oshima, M. Mapping of the antibody-binding regions of botulinum neorotoxin H-chain domain 855 to 1296 with anti-toxin antibodies from three host species. J. Prot. Chem. 1996, 15, 691–700. [Google Scholar] [CrossRef]
- Ben David, A.; Diamant, E.; Barnea, A.; Rosen, O.; Torgeman, A.; Zichel, R. The receptor binding domain of botulinum neurotoxin serotype A (BoNT/A) inhibits BoNT/A and BoNT/E intoxications in vivo. Clin. Vaccine Immunol. 2013, 20, 1433–1452. [Google Scholar] [CrossRef] [PubMed]
- Froude, J.W., 2nd; Thullier, P.; Pelat, T. Antibodies against anthrax: Mechanisms of action and clinical applications. Toxins Basel 2011, 3, 1433–1452. [Google Scholar] [CrossRef] [PubMed]
- Kelly-Cirino, C.D.; Mantis, N.J. Neutralizing monoclonal antibodies directed against defined linear epitopes on domain 4 of anthrax protective antigen. Infect. Immun. 2009, 77, 4859–4867. [Google Scholar] [CrossRef] [PubMed]
- Mechaly, A.; Levy, H.; Epstein, E.; Rosenfeld, R.; Marcus, H.; Ben-Arie, E.; Shafferman, A.; Ordentlich, A.; Mazor, O. A novel mechanism for antibody-based anthrax toxin neutralization: Inhibition of prepore-to-pore conversion. J. Biol. Chem. 2012, 287, 32665–32673. [Google Scholar] [CrossRef] [PubMed]
- Reason, D.; Liberato, J.; Sun, J.; Keitel, W.; Zhou, J. Frequency and domain specificity of toxin-neutralizing paratopes in the human antibody response to anthrax vaccine adsorbed. Infect. Immun. 2009, 77, 2030–2035. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, J.N.; Maynard, J.A. Characterization of a key neutralizing epitope on pertussis toxin recognized by monoclonal antibody 1B7. Biochemistry 2009, 48, 11982–11993. [Google Scholar] [CrossRef] [PubMed]
- Olsnes, S.; Pappenheimer, A.M., Jr.; Meren, R. Lectins from Abrus precatorius and Ricinus communis. II. Hybrid toxins and their interaction with chain-specific antibodies. J. Immunol. 1974, 113, 842–847. [Google Scholar] [PubMed]
- O’Hara, J.M.; Neal, L.M.; McCarthy, E.A.; Kasten-Jolly, J.A.; Brey, R.N., 3rd; Mantis, N.J. Folding domains within the ricin toxin A subunit as targets of protective antibodies. Vaccine 2010, 28, 7035–7046. [Google Scholar] [CrossRef] [PubMed]
- Mazuet, C.; Dano, J.; Popoff, M.R.; Créminon, C.; Volland, H. Characterization of botulinum neurotoxin type a neutralizing monoclonal antibodies and influence of their half-lives on therapeutic activity. PLoS ONE 2010, 5, e12416. [Google Scholar] [CrossRef] [PubMed]
- Chow, S.K.; Smith, C.; MacCarthy, T.; Pohl, M.A.; Bergman, A.; Casadevall, A. Disease-enhancing antibodies improve the efficacy of bacterial toxin-neutralizing antibodies. Cell Host Microbe 2013, 13, 417–428. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Tepp, W.H.; Liu, H.; Johnson, E.A.; Chapman, E.R. Mechanism of botulinum neurotoxin B and G entry into hippocampal neurons. J. Cell Biol. 2007, 179, 1511–1522. [Google Scholar] [CrossRef] [PubMed]
- Chanh, T.C.; Romanowski, M.J.; Hewetson, J.F. Monoclonal antibody prophylaxis against the in vivo toxicity of ricin in mice. Immunol. Investig. 1993, 22, 63–72. [Google Scholar] [CrossRef]
- Swaminathan, S. Molecular structures and functional relationships in clostridial neurotoxins. FEBS J. 2011, 278, 4467–4485. [Google Scholar] [CrossRef] [PubMed]
- Bavari, S.; Ulrich, R.G.; LeClaire, R.D. Cross-reactive antibodies prevent the lethal effects of Staphylococcus aureus superantigens. J. Infect. Dis. 1999, 180, 1365–1369. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.G. The significance of superantigens. Trends Microbiol. 1998, 6, 134. [Google Scholar] [CrossRef]
- Katinger, H.; Posner, M.R.; Cavacini, L.; Zolla-Pazner, S.; Gorny, M.K.; Sodroski, J.; Chou, T.C.; Li, A.; Baba, T.W.; Ruprecht, R.M. Synergistic neutralization of simian-human immunodeficiency virus SHIV-vpu+ by triple and quadruple combinations of human monoclonal antibodies and high-titer anti-human immunodeficiency virus type 1 immunoglobulins. J. Virol. 1998, 72, 3235–3240. [Google Scholar]
- Ter Meulen, J.; van den Brink, E.N.; Poon, L.L.; Marissen, W.E.; Leung, C.S.; Cox, F.; Cheung, C.Y.; Bakker, A.Q.; Bogaards, J.A.; van Deventer, E.; et al. Human monoclonal antibody combination against SARS coronavirus: Synergy and coverage of escape mutants. PLoS Med. 2006, 3, e237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faleri, A.; Santini, L.; Brier, S.; Pansegrau, W.; lo Surdo, P.; Scarselli, M.; Buricchi, F.; Volpini, G.; Genovese, A.; van der Veen, S.; et al. Two cross-reactive monoclonal antibodies recognize overlapping epitopes on Neisseria meningitidis factor H binding protein but have different functional properties. FASEB J. 2014, 28, 1644–1653. [Google Scholar] [CrossRef] [PubMed]
- McNeil, L.K.; Zagursky, R.J.; Lin, S.L.; Murphy, E.; Zlotnick, G.W.; Hoiseth, S.K.; Jansen, K.U.; Anderson, A.S. Role of factor H binding protein in Neisseria meningitidis virulence and its potential as a vaccine candidate to broadly protect against meningococcal disease. Microbiol. Mol. Biol. Rev. 2013, 77, 234–252. [Google Scholar] [CrossRef] [PubMed]
- Pless, D.D.; Torres, E.R.; Reinke, E.K.; Bavari, S. High-affinity, protective antibodies to the binding domain of botulinum neurotoxin type A. Infect. Immun. 2001, 69, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Amersdorfer, P.; Wong, C.; Smith, T.; Chen, S.; Deshpande, S.; Sheridan, R.; Marks, J.D. Genetic and immunological comparison of anti-botulinum type A antibodies from immune and non-immune human phage libraries. Vaccine 2002, 20, 1640–1648. [Google Scholar] [CrossRef]
- Maynard, J.A.; Maassen, C.B.; Leppla, S.H.; Brasky, K.; Patterson, J.L.; Iverson, B.L.; Georgiou, G. Protection against anthrax toxin by recombinant antibody fragments correlates with antigen affinity. Nat. Biotechnol. 2002, 20, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Scott, N.; Qazi, O.; Wright, M.J.; Fairweather, N.F.; Deonarain, M.P. Characterisation of a panel of anti-tetanus toxin single-chain Fvs reveals cooperative binding. Mol. Immunol. 2010, 47, 1931–1941. [Google Scholar] [CrossRef] [PubMed]
- Greenspan, N.S. Affinity, complementarity, cooperativity, and specificity in antibody recognition. Curr. Top. Microbiol. Immunol. 2001, 260, 65–85. [Google Scholar] [PubMed]
- Eisen, H.N. Affinity enhancement of antibodies: How low-affinity antibodies produced early in immune responses are followed by high-affinity antibodies later and in memory B-cell responses. Cancer Immunol. Res. 2014, 2, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Karush, F. The Affinity of Antibody: Range, Variability, and the Role of Multivalence. In Immunoglobulins; Litman, G.W., Good, R.A., Eds.; Springer: New York, NY, USA, 1978; pp. 85–116. [Google Scholar]
- Crothers, D.M.; Metzger, H. The influence of polyvalency on the binding properties of antibodies. Immunochemistry 1972, 9, 341–357. [Google Scholar] [CrossRef]
- Moyle, W.R.; Anderson, D.M.; Ehrlich, P.H. A circular antibody-antigen complex is responsible for increased affinity shown by mixtures of monoclonal antibodies to human chorionic gonadotropin. J. Immunol. 1983, 131, 1900–1905. [Google Scholar] [PubMed]
- Daeron, M. Fc receptor biology. Annu. Rev. Immunol. 1997, 15, 203–234. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, S.B.; Kimberly, R.P.; Valinsky, J.E.; Witmer, M.D.; Bussel, J.B.; Nachman, R.L.; Unkeless, J.C. Blockade of clearance of immune complexes by an anti-Fc gamma receptor monoclonal antibody. J. Exp. Med. 1986, 164, 474–489. [Google Scholar] [CrossRef] [PubMed]
- Mousavi, S.A.; Sporstol, M.; Fladeby, C.; Kjeken, R.; Barois, N.; Berg, T. Receptor-mediated endocytosis of immune complexes in rat liver sinusoidal endothelial cells is mediated by FcgammaRIIb2. Hepatology 2007, 46, 871–884. [Google Scholar] [CrossRef] [PubMed]
- Tomita, M.; Yamamoto, K.; Kobashi, H.; Ohmoto, M.; Tsuji, T. Immunohistochemical phenotyping of liver macrophages in normal and diseased human liver. Hepatology 1994, 20, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Finbloom, D.S.; Plotz, P.H. Studies of reticuloendothelial function in the mouse with model immune complexes. I. Serum clearance and tissue uptake in normal C3H mice. J. Immunol. 1979, 123, 1594–1599. [Google Scholar] [PubMed]
- Mannik, M.; Arend, M.P.; Hall, A.P.; Gilliland, B.C. Studies on antigen-antibody complexes. I. Elimination of soluble complexes from rabbit circulation. J. Exp. Med. 1971, 133, 713–739. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.G.; Lovdal, T.; Magnusson, K.E.; Berg, T.; Skogh, T. Liver cell uptake and degradation of soluble immunoglobulin G immune complexes in vivo and in vitro in rats. Hepatology 1996, 24, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Ravetch, J.V.; Clynes, R.A. Divergent roles for Fc receptors and complement in vivo. Annu. Rev. Immunol. 1998, 16, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Ravichandran, E.; Gong, Y.; Al Saleem, F.H.; Ancharski, D.M.; Joshi, S.G.; Simpson, L.L. An initial assessment of the systemic pharmacokinetics of botulinum toxin. J. Pharmacol. Exp. Ther. 2006, 318, 1343–1351. [Google Scholar] [CrossRef] [PubMed]
- Datta-Mannan, A.; Witcher, D.R.; Tang, Y.; Watkins, J.; Wroblewski, V.J. Monoclonal antibody clearance. Impact of modulating the interaction of IgG with the neonatal Fc receptor. J. Biol. Chem. 2007, 282, 1709–1717. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.; DiLillo, D.J.; Bournazos, S.; Li, F.; Ravetch, J.V. Mouse model recapitulating human Fcgamma receptor structural and functional diversity. Proc. Natl. Acad. Sci. USA 2012, 109, 6181–6186. [Google Scholar] [CrossRef] [PubMed]
- Bournazos, S.; Chow, S.K.; Abboud, N.; Casadevall, A.; Ravetch, J.V. Human IgG Fc domain engineering enhances antitoxin neutralizing antibody activity. J. Clin. Investig. 2014, 124, 725–729. [Google Scholar] [CrossRef] [PubMed]
- Vitale, L.; Blanset, D.; Lowy, I.; O’Neill, T.; Goldstein, J.; Little, S.F.; Andrews, G.P.; Dorough, G.; Taylor, R.K.; Keler, T. Prophylaxis and therapy of inhalational anthrax by a novel monoclonal antibody to protective antigen that mimics vaccine-induced immunity. Infect. Immun. 2006, 74, 5840–5847. [Google Scholar] [CrossRef] [PubMed]
- Abboud, N.; Chow, S.K.; Saylor, C.; Janda, A.; Ravetch, J.V.; Scharff, M.D.; Casadevall, A. A requirement for FcgammaR in antibody-mediated bacterial toxin neutralization. J. Exp. Med. 2010, 207, 2395–2405. [Google Scholar] [CrossRef] [PubMed]
- Akiyoshi, D.E.; Sheoran, A.S.; Rich, C.M.; Richard, L.; Chapman-Bonofiglio, S.; Tzipori, S. Evaluation of Fab and F(ab')2 fragments and isotype variants of a recombinant human monoclonal antibody against Shiga toxin 2. Infect. Immun. 2010, 78, 1376–1382. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, J.M.; Mukherjee, J.; Leysath, C.E.; Debatis, M.; Ofori, K.; Baldwin, K.; Boucher, C.; Peters, R.; Beamer, G.; Sheoran, A.; et al. A single VHH-based toxin-neutralizing agent and an effector antibody protect mice against challenge with Shiga toxins 1 and 2. Infect. Immun. 2013, 81, 4592–4603. [Google Scholar] [CrossRef] [PubMed]
- Vance, D.J.; Tremblay, J.M.; Mantis, N.J.; Shoemaker, C.B. Stepwise engineering of heterodimeric single domain camelid VHH antibodies that passively protect mice from ricin toxin. J. Biol. Chem. 2013, 288, 36538–36547. [Google Scholar] [CrossRef] [PubMed]
- Lindorfer, M.A.; Hahn, C.S.; Foley, P.L.; Taylor, R.P. Heteropolymer-mediated clearance of immune complexes via erythrocyte CR1: Mechanisms and applications. Immunol. Rev. 2001, 183, 10–24. [Google Scholar] [CrossRef] [PubMed]
- Muller, T.; Dietzschold, B.; Ertl, H.; Fooks, A.R.; Freuling, C.; Fehlner-Gardiner, C.; Kliemt, J.; Meslin, F.X.; Franka, R.; Rupprecht, C.E.; et al. Development of a mouse monoclonal antibody cocktail for post-exposure rabies prophylaxis in humans. PLoS Negl. Trop. Dis. 2009, 3, e542. [Google Scholar] [CrossRef] [PubMed]
- Varshney, A.K.; Wang, X.; MacIntyre, J.; Zollner, R.S.; Kelleher, K.; Kovalenko, O.V.; Pechuan, X.; Byrne, F.R.; Fries, B.C. Humanized Staphylococcal Enterotoxin B (SEB)-Specific Monoclonal Antibodies Protect From SEB Intoxication and Staphylococcus aureus Infections Alone or as Adjunctive Therapy With Vancomycin. J. Infect. Dis. 2014, 210, 973–981. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diamant, E.; Torgeman, A.; Ozeri, E.; Zichel, R. Monoclonal Antibody Combinations that Present Synergistic Neutralizing Activity: A Platform for Next-Generation Anti-Toxin Drugs. Toxins 2015, 7, 1854-1881. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins7061854
Diamant E, Torgeman A, Ozeri E, Zichel R. Monoclonal Antibody Combinations that Present Synergistic Neutralizing Activity: A Platform for Next-Generation Anti-Toxin Drugs. Toxins. 2015; 7(6):1854-1881. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins7061854
Chicago/Turabian StyleDiamant, Eran, Amram Torgeman, Eyal Ozeri, and Ran Zichel. 2015. "Monoclonal Antibody Combinations that Present Synergistic Neutralizing Activity: A Platform for Next-Generation Anti-Toxin Drugs" Toxins 7, no. 6: 1854-1881. https://0-doi-org.brum.beds.ac.uk/10.3390/toxins7061854