Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents
Abstract
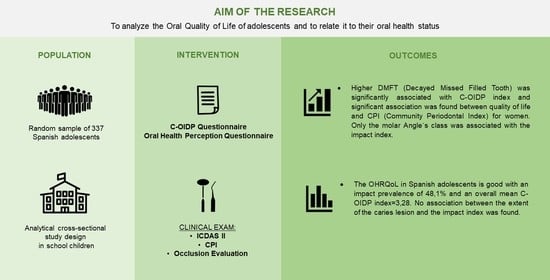
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sample Selection
2.3. Survey Instruments
2.3.1. Oral Health Perception Questionnaire
2.3.2. Child-OIDP Questionnaire
2.4. Clinical Diagnostic Criteria
2.4.1. Dental Status
2.4.2. Periodontal Status
2.4.3. Occlusal Status
2.5. Field Work
2.6. Data Analysis
3. Results
3.1. Psychometric Properties of the Child-OIDP
3.2. Oral Health Perception
3.3. Impact of Oral Health Measured with Child-OIDP Index
3.4. Clinical Exam
3.5. Association between the C-OIDP Index and the Clinical Variables
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| C-OIDP | Child-Oral Impacts on Daily Performances |
| CPI | Community Periodontal Index |
| CS-C-OIDP | Condition Specific Child-Oral Impacts on Daily Performances |
| DMFT | Decayed Missed Filled Tooth |
| ICDAS II | International Caries Detection and Assessment System |
| OHRQoL | Oral-Health-Related Quality of Life |
| QoL | Quality of Life |
| OSS | Oral Satisfaction Scale |
| SESPO | Sociedad Española de Epidemiología y Salud Pública Oral |
| WHO | World Health Organization. |
References
- Kazeminia, M.; Abdi, A.; Shohaimi, S.; Jalali, R.; Vaisi-Raygani, A.; Salari, N.; Mohammadi, M. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: A systematic review and meta-analysis. Head Face Med. 2020, 16, 22. [Google Scholar] [CrossRef]
- Blatz, M.B.; Chiche, G.; Bahat, O.; Roblee, R.; Coachman, C.; Heymann, H.O. Evolution of Aesthetic Dentistry. J. Dent. Res. 2019, 98, 1294–1304. [Google Scholar] [CrossRef]
- Hescot, P. The New Definition of Oral Health and Relationship between Oral Health and Quality of Life. Chin. J. Dent. Res. 2017, 20, 189–192. [Google Scholar]
- The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [CrossRef]
- Locker, D. Concepts of Oral Health, Disease and the Quality of Life. In Measuring Oral Health and Quality of Life; Slade, G.D., Ed.; University of North Carolina: Chapel Hill, NC, USA, 1997; pp. 11–23. [Google Scholar]
- Thomson, W.M.; Broder, H.L. Oral Health-Related Quality of Life in Children and Adolescents. Pediatr. Clin. North 2018, 65, 1073–1084. [Google Scholar] [CrossRef]
- Atchison, K.A.; Dolan, T.A. Development of the Geriatric Oral Health Assessment Index. J. Dent. Educ. 1990, 54, 680–687. [Google Scholar] [CrossRef]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar]
- Leão, A.; Sheiham, A. The development of a socio-dental measure of dental impacts on daily living. Community Dent. Health 1996, 13, 22–26. [Google Scholar]
- Adulyanon, S.; Sheiham, A. Oral Impacts on Daily Performances. In Measuring Oral Health and Quality of Life; Slade, G.D., Ed.; University of North Carolina: Chapel Hill, NC, USA, 1997; pp. 151–160. [Google Scholar]
- Culler, C.S.; Gunarajasingam, D.; Henshaw, M.M. Preschool oral health-related quality of life: A practical guide to measurement tools. J. Public Health Dent. 2021, 81, 29–41. [Google Scholar] [CrossRef]
- Hettiarachchi, R.M.; Kularatna, S.; Byrnes, J.; Scuffham, P.A. Pediatric Quality of Life Instruments in Oral Health Research: A Systematic Review. Value Health 2019, 22, 129–135. [Google Scholar] [CrossRef]
- Thomson, W.M. Subjective oral health measures for use with children: New Zealand´s contribution to a burgeoning field. J. R. Soc. N. Z. 2020, 50, 4–14. [Google Scholar] [CrossRef]
- Jokovic, A.; Locker, D.; Stephens, M.; Kenny, D.; Tompson, B.; Guyatt, G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J. Dent. Res. 2002, 81, 459–463. [Google Scholar] [CrossRef]
- Broder, H.L.; McGrath, C.; Cisneros, G.J. Questionnaire development: Face validity and item impact testing of the Child Oral Health Impact Profile. Community Dent. Oral Epidemiol. 2007, 1, 8–19. [Google Scholar] [CrossRef]
- Gherunpong, S.; Tsakos, G.; Sheiham, A. Developing and evaluating an oral health-related quality of life index for children; the CHILD-OIDP. Community Dent. Health 2004, 21, 161–169. [Google Scholar]
- Bernabé, E.; Krisdapong, S.; Sheiham, A.; Tsakos, G. Comparison of the discriminative ability of the generic and condition-specific forms of the Child-OIDP index: A study on children with different types of normative dental treatment needs. Community Dent. Oral Epidemiol. 2009, 37, 155–162. [Google Scholar] [CrossRef]
- Mbawalla, H.S.; Mtaya, M.; Masalu, J.R.; Brudvik, P.; Astrom, A.N. Discriminative ability of the generic and condition-specific Child-Oral Impacts on Daily Performances (Child-OIDP) by the Limpopo-Arusha School Health (LASH) project: A cross-sectional study. BMC Pediatr. 2011, 11, 45. [Google Scholar] [CrossRef]
- Patil, S.; Kahtani, A.A.; Baeshen, H.A.; Alamir, A.W.; Khan, S.; Bhandi, S.; Hosmani, J.; Raj, A.T.; Gadbail, A.; Gondivkar, S.; et al. Face Validity and Psychometric Evaluation of the Available Oral Health-related Quality of Life Instruments: A Systematic Review. Oral Health Prev. Dent. 2020, 18, 409–416. [Google Scholar]
- Pentapati, K.C.; Yeturu, S.K.; Siddiq, H. A reliability generalization meta-analysis of Child Oral Impacts on Daily Performances (C-OIDP) questionnaire. J. Oral Biol. Craniofac. Res. 2020, 10, 776–781. [Google Scholar] [CrossRef]
- Cortés-Martinicorena, F.J.; Rosel-Gallardo, E.; Artazcoz-Osés, J.; Bravo, M.; Tsakos, G. Adaptation and validation for Spain of the Child-Oral Impact on Daily Performance (C-OIDP) for use with adolescents. Med. Oral Patol. Oral Cir. Bucal 2010, 15, 106–111. [Google Scholar] [CrossRef]
- Montero, J.; Rosel, E.; Barrios, R.; López-Valverde, A.; Albaladejo, A.; Bravo, M. Oral health-related quality of life in 6- to 12-year-old schoolchildren in Spain. Int. J. Paediatr. Dent. 2016, 26, 220–230. [Google Scholar] [CrossRef]
- Bravo, M.; Cortés, F.J.; Casals, E.; Llena, C.; Almerich-Silla, J.M.; Cuenca, E. Basic oral health goals for Spain 2015/2020. Int. Dent. J. 2009, 59, 78–82. [Google Scholar]
- Bravo Pérez, M.; Almerich Silla, J.M.; Canorea Díaz, E.; Casals Peidró, E.; Cortés Martinicorena, F.J.; Expósito Delgado, A.J.; Gómez Santos, G.; Hidalgo Olivares, G.; Lamas Oliveira, M.; Martínez Beneyto, Y.; et al. Encuesta de Salud Oral en España 2020. RCOE 2020, 25, 12–69. [Google Scholar]
- Petersen, P.E.; Baez, R.J.; World Health Organization. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013; pp. 42–56. [Google Scholar]
- Álvarez-Azaustre, M.P.; Greco, R.; Llena, C. Oral Health-Related Quality of Life in Adolescents as Measured with the Child-OIDP Questionnaire: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12995. [Google Scholar] [CrossRef]
- Almerich-Silla, J.M.; Boronat-Ferrer, T.; Montiel-Company, J.M.; Iranzo-Cortés, J.E. Caries prevalence in children from Valencia (Spain) using ICDAS II criteria, 2010. Med. Oral Patol Oral Cir. Bucal 2014, 19, 574–580. [Google Scholar] [CrossRef]
- Almerich-Torres, T.; Montiel-Company, J.M.; Bellot-Arcís, C.; Iranzo-Cortés, J.E.; Ortolá-Siscar, J.C.; Almerich-Silla, J.M. Caries Prevalence Evolution and Risk Factors among Schoolchildren and Adolescents from Valencia (Spain): Trends 1998–2018. Int. J. Environ. Res. Public Health 2020, 17, 6561. [Google Scholar] [CrossRef]
- Dikmen, B. Icdas II criteria (International Caries Detection and Assessment System). J. Istanb. Univ. Fac. Dent. 2015, 49, 63–72. [Google Scholar] [CrossRef]
- Ismail, A.I.; Sohn, W.; Tellez, M.; Amaya, A.; Sen, A.; Hasson, H.; Pitts, N.B. The International Caries Detection and Assessment System (ICDAS): An integrated system for measuring dental caries. Community Dent. Oral Epidemiol. 2007, 35, 170–178. [Google Scholar] [CrossRef] [Green Version]
- Pitts, N.B.; Carter, N.L.; Tsakos, G. The Brussels Statement on the Future Needs for Caries Epidemiology and Surveillance in Europe. Community Dent. Health 2018, 35, 66. [Google Scholar]
- Montero, J.; Bravo, M.; Albaladejo, A. Validation of two complementary oral-health related quality of life indicators (OIDP and OSS 0-10) in two qualitatively distinct samples of the Spanish population. Health Qual. Life Outcomes 2008, 6, 101. [Google Scholar] [CrossRef]
- ICCMS™ Caries Management. Available online: https://www.iccms-web.com (accessed on 11 August 2022).
- Proffit, W.R.; Fields, H.W., Jr.; Sarver, D.M.; Tello-Rodríguez, A.I. Contemporary Orthodontics, 6th ed.; Elsevier: Philadelphia, PA, USA, 2019. [Google Scholar]
- Bernabé, E.; Sheiham, A.; Tsakos, G. A comprehensive evaluation of the validity of Child-OIDP: Further evidence from Peru. Community Dent. Oral Epidemiol. 2008, 36, 317–325. [Google Scholar] [CrossRef]
- Castro, R.A.L.; Cortes, M.I.S.; Leão, A.T.; Portela, M.C.; Souza, I.P.R.; Tsakos, G.; Marcenes, W.; Sheiham, A. Child-OIDP index in Brazil: Cross-cultural adaptation and validation. Health Qual. Life Outcomes 2008, 6, 68. [Google Scholar] [CrossRef]
- Yusuf, H.; Gherunpong, S.; Tsakos, G.; Sheiham, A. Validation of an English version of Child-OIDP index, an oral health related quality of life measure for children. Health Qual. Life Outcomes 2006, 4, 38. [Google Scholar] [CrossRef]
- Tubert-Jeannin, S.; Pegon-Machat, E.; Gremeau-Richard, C.; Lecuyer, M.M.; Tsakos, G. Validation of a French version of Child-OIDP index. Eur. J. Oral Sci. 2005, 113, 355–362. [Google Scholar] [CrossRef]
- Rosel, E.; Tsakos, G.; Bernabé, E.; Sheiham, A.; Bravo, M. Assessing the level of agreement between the self- and interview-administered Child-OIDP. Community Dent. Oral Epidemiol. 2010, 38, 340–347. [Google Scholar] [CrossRef]
- Pitts, N.B.; Banerjee, A.; Mazevet, M.E.; Goffin, G.; Martignon, S. From ‘ICDAS’ to ‘Caries Care International’: The 20-year journey building international consensus to take caries evidence into clinical practice. Br. Dent. J. 2021, 231, 769–774. [Google Scholar] [CrossRef]
- Bianco, A.; Fortunato, L.; Nobile, C.G.A.; Pavia, M. Prevalence and determinants of oral impacts on daily performance: Results from a survey among school children in Italy. Eur. J. Public Health 2010, 20, 595–600. [Google Scholar] [CrossRef]
- Pavithran, V.K.; Murali, R.; Krishna, M.; Shamala, A.; Yalamalli, M.; Kumar, A.V.; Raina, R. Impact of oral diseases on daily activities among 12- to 15-year-old institutionalized orphan and non-orphan children in Bengaluru city: A cross-sectional analytical study. Indian J. Dent. Res. 2020, 31, 396–402. [Google Scholar] [CrossRef]
- Alzahrani, A.A.H.; Alhassan, E.M.; Albanghali, M.A. Association between oral diseases and impact on daily performance among male Saudi schoolchildren. Clin. Exp. Dent. Res. 2019, 5, 655–664. [Google Scholar] [CrossRef] [Green Version]
- Dumitrache, M.A.; Comes, C.; Teodorescu, E.; Dumitrascu, L.; Cuculescu, M.; Ionescu, E. Life quality related to oral health of schoolchildren from Bucharest. Rev. Romana Bioet. 2009, 7, 169–178. [Google Scholar]
- Hamamci, N.; Başaran, G.; Uysal, E. Dental Aesthetic Index scores and perception of personal dental appearance among Turkish university students. Eur. J. Orthod. 2009, 31, 168–173. [Google Scholar] [CrossRef]
- Bakhtiar, M.; Mohammadi, T.M.; Hajizamani, A.; Vossoughi, M. Association of Oral Health Indicators with Quality-of-Life Related to Oral Health among Iranian Adolescent. J. Int. Oral Health 2014, 6, 5–9. [Google Scholar]
- Basavaraj, P.; Sunil, M.K.; Nagarajappa, R.; Ashish, S.; Ramesh, G. Correlation between oral health and Child-OIDP Index in 12-and 15-year-old children from Modinagar, India. Asia Pac. J. Public Health 2014, 26, 390–400. [Google Scholar] [CrossRef]
- Alrashed, M.; Alqerban, A. The relationship between malocclusion and oral health-related quality of life among adolescents: A systematic literature review and meta-analysis. Eur. J. Orthod. 2021, 43, 173–183. [Google Scholar] [CrossRef]
- Cronbach, L. Coefficient alpha and the internal structure of tests. Psychometrica 2006, 16, 297–333. [Google Scholar] [CrossRef]
- Athira, S.; Jayakumar, H.L.; Chandra, M.; Gupta, T.; Dithi, C.; Anand, P.J.S. Oral Health-Related Quality of Life of School Children Aged 12–17 Years According to the Child-Oral Impacts on Daily Performances Index and the Impact of Oral Health Status on Index Scores. Int. J. Prev. Public Health Sci. 2015, 1, 25–30. [Google Scholar]
- Dhawan, P.; Singh, A.; Agarwal, A.; Aeran, H. Psychometric properties of Hindi version of child oral impact on daily performances (C-OIDP) index amongst school children in North India. J. Oral Biol. Craniofac. Res. 2019, 9, 10–13. [Google Scholar] [CrossRef]
- Simangwa, L.D.; Johansson, A.K.; Johansson, A.; Minja, I.K.; Åstrøm, A.N. Oral impacts on daily performances and its socio-demographic and clinical distribution: A cross-sectional study of adolescents living in Maasai population areas, Tanzania. Health Qual. Life Outcomes 2020, 18, 181. [Google Scholar] [CrossRef]
- Reinoso-Vintimilla, N.; del Castillo-López, C. Calidad de vida relacionada a la salud bucal en escolares de Sayausí, Cuenca Ecuador. Quality of life related to the oral health in school from Sayausí, Cuenca Ecuador. Rev. Estomatol. Hered. 2017, 27, 227–234. [Google Scholar] [CrossRef]
- Kumar, S.; Kumar, A.; Badiyani, B.; Kumar, A.; Basak, D.; Ismail, L.M.B. Oral health impact, dental caries experience, and associated factors in 12–15-year-old school children in India. Int. J. Adolesc. Med. Health 2017, 29, 2. [Google Scholar] [CrossRef]
- Paredes-Martínez, E.R.; Díaz-Pizán, M.E. Impact of oral conditions on the quality of life in schoolchildren in San Juan de Miraflores. Lima, Perú. Rev. Estomatol. Hered. 2014, 24, 171–177. [Google Scholar] [CrossRef]
- Naidoo, S.; Sheiham, A.; Tsakos, G. The relation between oral impacts on daily performances and perceived clinical oral conditions in primary school children in the Ugu District, Kwazulu Natal, South Africa. SADJ 2013, 68, 214–218. [Google Scholar]
- Nordin, E.A.B.; Shoaib, L.A.; Yusof, Z.Y.M.; Manan, N.M.; Othman, S.A. Oral health-related quality of life among 11–12 years old indigenous children in Malaysia. BMC Oral Health 2019, 19, 152. [Google Scholar]
- Bernabé, E.; Tsakos, G.; Sheiham, A. Intensity and extent of oral impacts on daily performances by type of self-perceived oral problems. Eur. J. Oral Sci. 2007, 115, 111–116. [Google Scholar] [CrossRef]
- Marcelo-Ingunza, J.; del Castillo-López, C.; Evangelista-Alva, A.; Sánchez-Borjas, P. Oral Health Related Quality of Life in school children of urban-marginal area. Rev. Estomatol. Hered. 2015, 25, 194–204. [Google Scholar]
- Moreno-Ruiz, X.; Vera-Abara, C.; Cartes-Velásquez, R. Oral health impact on the quality of life of 11 to 14 years-old schoolchildren, Licantén, 2013. Rev. Clin. Periodoncia Implantol. Rehabil. Oral 2014, 7, 142–148. [Google Scholar]
- Arumrahayu, W.; Maharani, D.A.; Adiatman, M. An Indonesian version of child oral impact on daily performances (C-OIDP): Assessing validity and reliability. J. Int. Dent. Med. Res. 2018, 11, 1049–1052. [Google Scholar]
- Vera, C.; Moreno, X.; Rivera, D.C. Adaptation and validation of Child Oral Impact on Daily Performance index in 11-14-year-old Chilean school children. J. Oral Res. 2013, 2, 119–124. [Google Scholar] [CrossRef]
- Peker, K.; Eden, E.; Ak, A.S.; Uysal, Ö.; Bermek, G. Psychometric evaluation of the child oral impacts on daily performances (C-OIDP) for use in Turkish primary school children: A cross sectional validation study. BMC Oral Health 2020, 20, 173. [Google Scholar] [CrossRef]
- Chaudhary, F.A.; Iqbal, A.; Khalid, M.D.; Noor, N.; Syed, J.; Baig, M.N.; Khattak, O.; Din, S.U. Validation and Reliability Testing of the Child Oral Impacts on Daily Performances (C-OIDP): Cross-Cultural Adaptation and Psychometric Properties in Pakistani School-Going Children. Children 2022, 9, 631. [Google Scholar] [CrossRef]
- Nasia, A.A.; Arumrahayu, W.; Rosalien, R.; Maharani, A.; Adiatman, M. Child-oral impacts on daily performances index in indonesia: Cross-cultural adaptation and initial validation. Malays. J. Public Health Med. 2019, 2, 68–77. [Google Scholar] [CrossRef]
- Alade, O.; Ajoloko, E.; Dedeke, A.; Uti, O.; Sofola, O. Self-reported halitosis and oral health related quality of life in adolescent students from a suburban community in Nigeria. Afr. Health Sci. 2020, 20, 2044–2049. [Google Scholar] [CrossRef]
- Kragt, L.; Dhamo, B.; Wolvius, E.B.; Ongkosuwito, E.M. The impact of malocclusions on oral health-related quality of life in children-a systematic review and meta-analysis. Clin. Oral Investig. 2016, 20, 1881–1894. [Google Scholar] [CrossRef]

| ICDAS II | |||
|---|---|---|---|
| Restoration Code | Criteria | Caries Code | Criteria |
| 0 | No restoration or sealant | 0 | Healthy |
| 1 | Sealant in poor condition | 1 | Visual change in enamel after drying |
| 2 | Sealant in good condition | 2 | Visual change in enamel with wet tooth |
| 3 | Tooth-coloured filling | 3 | Localized enamel break |
| 4 | Amalgam | 4 | Underlying dark shade in dentine |
| 5 | Steel crown | 5 | Cavity with exposed dentine |
| 6 | Porcelain restoration | 6 | Extensive cavity |
| 7 | Lost or fractured filling | ||
| 8 | Temporary restoration | ||
| C-OIDP | Eating | Speaking | Brushing | Sleeping | Emotion | Schoolwork | Smiling | Playing |
|---|---|---|---|---|---|---|---|---|
| Eating | 1.00 | |||||||
| Speaking | 0.28 | 1.00 | ||||||
| Brushing | 0.16 | 0.47 | 1.00 | |||||
| Sleeping | 0.23 | 0.41 | 0.15 | 1.00 | ||||
| Emotion | 0.39 | 0.48 | 0.43 | 0.41 | 1.00 | |||
| Schoolwork | 0.32 | 0.41 | 0.42 | 0.06 | 0.34 | 1.00 | ||
| Smiling | 0.09 | 0.08 | 0.05 | 0.06 | 0.16 | 0.00 | 1.00 | |
| Playing | 0.15 | 0.13 | 0.09 | 0.08 | 0.07 | 0.07 | 0.00 | 1.000 |
| Corrected Item-Total Correlation | Cronbach’s Alpha If Item is Deleted | |
|---|---|---|
| Eating | 0.38 | 0.59 |
| Speaking | 0.57 | 0.56 |
| Brushing | 0.40 | 0.59 |
| Spleeping | 0.36 | 0.60 |
| Emotion | 0.61 | 0.50 |
| Schoolwork | 0.39 | 0.62 |
| Smiling | 0.13 | 0.70 |
| Playing | 0.13 | 0.65 |
| ICDAS 1–3 | ICDAS 4–6 | ||||
|---|---|---|---|---|---|
| N° of Teeth | n | % | N° of Teeth | n | % |
| 0 | 221 | 65.6 | 0 | 296 | 87.8 |
| 1 | 62 | 18.4 | 1 | 25 | 7.4 |
| 2 | 29 | 8.6 | 2 | 10 | 3 |
| 3 | 12 | 3.6 | 3 | 4 | 1.2 |
| 4 | 8 | 2.4 | 4 | 1 | 0.3 |
| 5 | 3 | 0.9 | 10 | 1 | 0.3 |
| 6 | 1 | 0.3 | |||
| 8 | 1 | 0.3 | |||
| Total | 337 | 100 | Total | 337 | 100 |
| CPI = 0 (Healthy) | CPI = 1 (Bleeding) | CPI = 2 (Calculus) | |
|---|---|---|---|
| Index Teeth | % Participants | ||
| 1.6 | 49.6 | 40.7 | 9.8 |
| 1.1 | 60.5 | 35.3 | 4.2 |
| 2.6 | 37.4 | 50.4 | 12.2 |
| 4.6 | 53.7 | 43.3 | 3 |
| 3.1 | 46.3 | 16 | 37.7 |
| 3.6 | 49.3 | 47.8 | 3 |
| C-OIDP | ||||||
|---|---|---|---|---|---|---|
| Variables | n | Mean ± SD | 95%CI | Median | Interq. Range | p |
| DMF-T Index = 0 | 234 | 3.16 ± 7.07 | 2.25–4.08 | 0 | 2.78 | 0.03 |
| DMF-T Index > 0 | 103 | 3.53 ± 5.21 | 2.51–4.55 | 1.38 | 5.56 | |
| ICDAS 1–3 = 0 | 221 | 3.45 ± 7.34 | 2.47–4.42 | 0 | 3.47 | 0.69 |
| ICDAS 1–3 > 0 | 116 | 2.95 ± 4.71 | 2.09–3.82 | 1.38 | 4.17 | |
| ICDAS 4–6 = 0 | 296 | 3.27 ± 6.74 | 2.50–4.04 | 0 | 2.78 | 0.89 |
| ICDAS 4–6 > 0 | 41 | 3.31 ± 5.10 | 1.70–4.93 | 0 | 5.56 | |
| CPI Index = 0 | 52 | 1.73 ± 2.47 | 1.04–2.42 | 0 | 2.78 | 0.36 |
| CPI Index > 0 | 285 | 3.56 ± 7.01 | 2.74–4.38 | 0 | 4.17 | |
| Malocclusion | 86 | 3.1 ± 7.5 | 1.5–4.7 | 0 | 4.5 | 0.37 |
| No malocclusion | 251 | 3.3 ± 6.1 | 2.5–4.1 | 0 | 4.1 | |
| No incisor crowding | 249 | 3.37 ± 6.98 | 2.50–4.24 | 0 | 4.17 | 0.90 |
| Incisor crowding | 88 | 3.01 ± 5.17 | 1.91–4.11 | 0 | 2.78 | |
| No incisor diastema | 278 | 3.39 ± 6.89 | 2.58–4.21 | 0 | 4.17 | 0.88 |
| Incisor diastema | 59 | 2.73 ± 4.67 | 1.51–3.94 | 0 | 2.78 | |
| No increased overbite | 226 | 3.52 ± 7.30 | 2.57–4.48 | 0 | 4.17 | 0.68 |
| Increased overbite | 111 | 2.77 ± 4.66 | 1.89–3.65 | 0 | 4.17 | |
| No increased overjet | 219 | 3.19 ± 6.49 | 2.33–4.06 | 0 | 4.17 | 0.56 |
| Increased overjet | 118 | 3.43 ± 6.69 | 2.21–4.66 | 0 | 2.78 | |
| No anterior open bite | 315 | 3.21 ± 6.65 | 2.47–3.95 | 0 | 2.78 | 0.12 |
| Anterior open bite | 22 | 4.22 ± 4.93 | 2.04–6.41 | 0 | 8.33 | |
| No posterior crossbite | 310 | 3.19 ± 6.41 | 2.47–3.91 | 0 | 2.78 | 0.33 |
| Posterior crossbite | 27 | 4.28 ± 8.10 | 1.06–7.47 | 0 | 4.17 | |
| Angle’s Class I | 111 | 2.6 ± 5.1 | 1.6–3.6 | 0 | 2.7 | 0.04 |
| Angle’s Class II | 121 | 3.6 ± 5.2 | 2.7–4.6 | 1.3 | 5.5 | |
| Angle’s Class III | 105 | 3.4 ± 8.8 | 1.7–5.1 | 0 | 2.7 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alvarez-Azaustre, M.P.; Greco, R.; Llena, C. Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents. Int. J. Environ. Res. Public Health 2022, 19, 12450. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph191912450
Alvarez-Azaustre MP, Greco R, Llena C. Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents. International Journal of Environmental Research and Public Health. 2022; 19(19):12450. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph191912450
Chicago/Turabian StyleAlvarez-Azaustre, María Paloma, Rossana Greco, and Carmen Llena. 2022. "Oral-Health-Related Quality of Life as Measured with the Child-OIDP Index and Oral Health Status in Spanish Adolescents" International Journal of Environmental Research and Public Health 19, no. 19: 12450. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph191912450